536 Abrupt Lesions PT Implications
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
130 Terms
mild TBI
TBI that causes concussion without structural injury
moderate
TBI that often involves structural injury
severe
TBI that involves loss of consciousness for longer than 6 hours
headache, disorientation & disturbances in cognition, dizziness, nausea, vomiting, mood and attention disorders, pain
common symptoms of concussion
True
True or false? The severity of amnesia related to the severity of the head injury?
retrograde amnesia
Refers to the loss of memories formed before the injury.
anterograde amnesia
Refers to the inability to form memories after the injury
neuropathic pain
common pain sensed with TBIs as a result of damage to sensory pathways (specifically, the thalamus)
ventral posterior nucleus
specific area of the thalamus that, when damaged, causes sensory abnormalities including hypoesthesia, hypoalgesia, and hyperalgesia
Glasgow Coma Scale (GCS)
How can altered consciousness and mental status be assessed after a TBI?
coma
Disorder of consciousness characterized by the following:
- Eyes do not open at all
- No communication
- No awareness, command following, or purposeful responses
Unresponsive Wakefulness
Disorder of consciousness characterized by the following:
- Eyes open at times but not sustained, sluggish
- No communication
- No awareness, command following, or purposeful responses
Minimally Conscious State
Disorder of consciousness characterized by the following:
- Eyes open more frequently, potentially progressing to normal eye opening/trackin
- Potential for yes/no nodding or gestures/verbal responses that may be inconsistent or unreliable
- purposeful but inconsistent awareness
ascending reticular activating system
Collection of brainstem nuclei that provide excitatory input to the cortex; damage at midbrain leads to altered states of consciousness.
Cushing's Triad
Signs of increased intracranial pressure or brainstem compression
hypertension, bradycardia, irregular respiration
Cushing's Triad symptoms
respiratory
These issues associated with TBI must be controlled immediately (especially when the pons and medulla are involved)
Cheyne-Stokes breathing
a distinct pattern of breathing characterized by oscillating patterns between rapid breathing and momentary pauses
hyperventilation
the condition of taking abnormally fast, deep breaths

apneustic breathing
a distinct pattern of breathing characterized by prolonged pauses occurring following inspiration
ataxic breathing
a distinct pattern of breathing characterized by irregular breathing rates and tidal volumes
Glasgow Coma Scale, CT first, MRI second, clinical symptoms
How do we diagnose TBIs
highest: 14
lowest: 3
highest and lowest score on glasgow coma scale
3-8
glasgow coma scale score indicating a minimally conscious state
cranial nerve reflexes, abnormal posturing
in comatose patients, how can the level of TBI damage be estimated?
flaccidity
Limpness or loss of muscle tone that often occurs at the onset of the brain injury
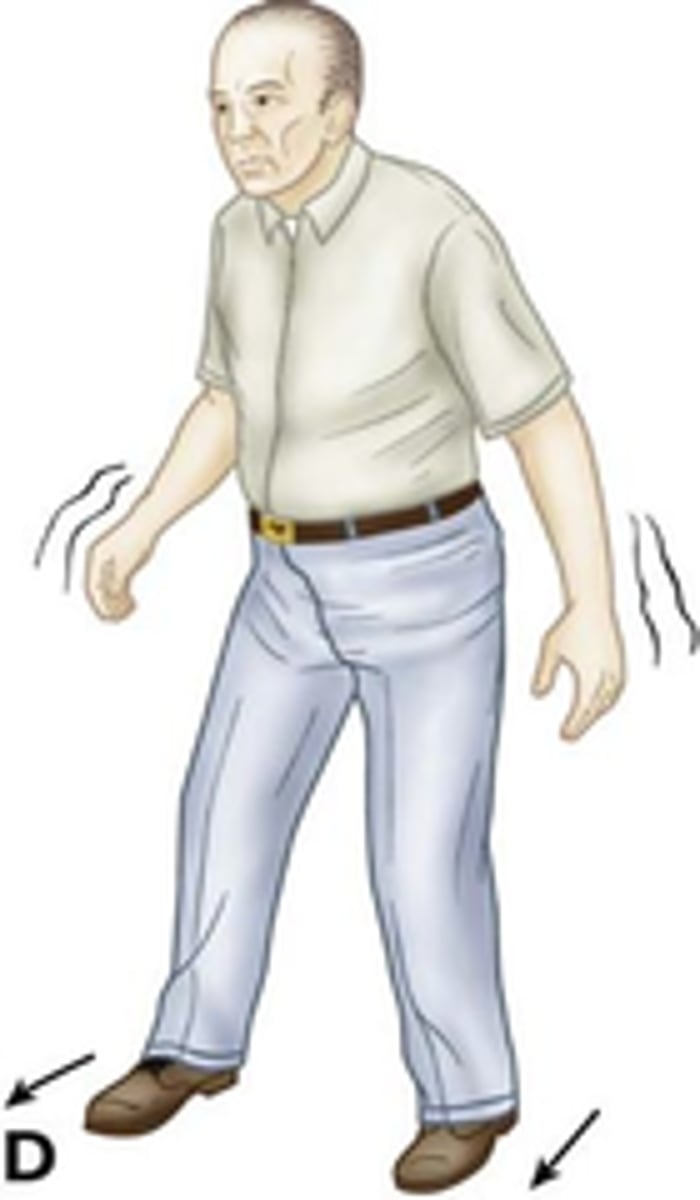
decorticate posturing
abnormal posturing that involves flexion of the arms, clenched hands,
and extended legs with pointed toes (TBI)

decerebrate posturing
Abnormal posturing that involves clenching the jaw and extension of the
arms and legs. That patient is rigid, and limbs are rotated internally (TBI)
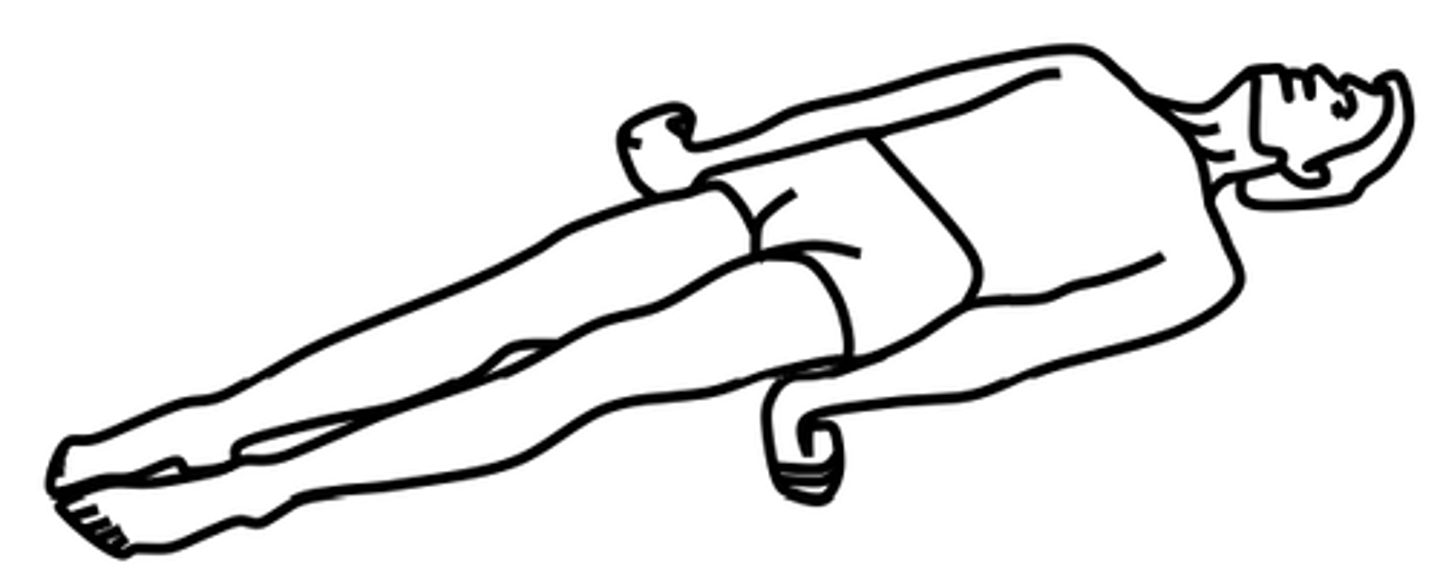
decorticate posturing
Abnormal posturing that suggests severe injury above the midbrain.
decerebrate posturing
Abnormal posturing that suggests severe injury at or below the level of the midbrain; poor prognosis
more accurately estimates herniation, minimizing secondary brain damage
Why would MRI potentially be a better for TBI diagnosing?
diffusion tensor imaging (MRI)
method to detect diffuse axonal injury that tracks the diffusion of water in order to trace myelinated axon
tracts; not routinely used in practice
N-acetylaspartate (NAA)
levels that correlate with the severity of damage and neurological outcomes of a TBI (second-most abundant amino acid in the CNS, after glutamate)
False (decrease)
True or false? Following TBI, NAA levels increase.
catheters in lateral ventricles/subarachnoid space, transcranial color doppler
How can ICP be monitored after a TBI?
infection
risk of catheters to monitor ICP
concussion
SCI in which a blow or violent shaking results in temporary loss of function
contusion
SCI in which the cord surface remains intact while the white or gray matter is damaged
laceration
SCI in which the spinal cord surface and tissue is torn
1. light touch/pinprick sensitivity
2. myotomes
How can we test for injury level of a SCI?
True
True or False? complete lesions cause loss of sensory and motor function while incomplete lesions leave some axons intact
paraplegia
Affects the lower trunk and limbs and is caused by
damage in the thoracic or lumbar regions of the spine
Quadriplegia
Affects all four limbs and the
trunk and is caused by injury in the cervical spine
80%
Symptoms of SCI common in 80% of SCI patients.
denervates phrenic n → paralysis of diaphragm → requires ventilator
How can SCIs at C4 affect the respirator system?
weak/paralyzed abdominal or intercostal mm → impaired coughing → secretion build-up & obstructive sleep apnea
How can SCIs between C5 and T12 affect the respiratory system?
pain, weakness, fatigue
common complaints that reduce the quality of life following SCI
autonomic dysfunction, depression, decreased mobility
what causes fatigue for those with a SCI
sleep, bladder & bowel function, cardiopulmonary function, sexual activity
Autonomic dysreflexia is a common syndrome in SCI that affects what aspects of life?
1. increased BP, heart rhythm
2. pounding headache
3. sweating/flushing of face, neck, shoulders
4. visual disturbances
5. anxiety
6. bladder/bowel incontinence
7. sexual dysfunction
8. compromised immune function
Following SCI, descending regulation of autonomic activity is lost, leading to what symptoms?
UMN: spastic bladders & bowels, erectile function preserved without ejaculation
bowel/bladder/sexual function symptoms of SCI above T12
LMN: flaccid bladders, bowels, and genitals.
bowel/bladder/sexual function symptoms of SCI below T12 (S1-S2)
CT scans (reliable)
MRI (better detect soft tissue damage, syringomyelia, & hematoma
What are good diagnostic methods for SCI?
UMN
Damage to the corticospinal tract creates UMN or LMN signs?
hyperreflexia or clonus, increase muscle tone, plantar reflex (Babinski), weakness w/o muscle wasting
UMN signs resulting from damage to the corticospinal tract
LMN injuries, partial UMN lesions that cause paralysis
What type of SCI injuries are more likely to cause "muscle wasting".
False (rapid onset)
True or False? Ischemic stroke symptoms are typically delayed.
aorta → ICA → (carotid foramina) → circle of Willis → MCA & ACA
flow of the significant arteries from the aorta to the brain (that run through the carotid foramina)
aorta → vertebral arteries → (foramen magnum) → basilar artery → joins Circle of Willis
flow of the significant arteries from the aorta to the brain (that run through the foramen magnum)
middle cerebral artery
artery that is the most common source of ischemic events, serving the lateral portions of the cerebrum
- CL weakness (UE/face > LE)
- CL sensory loss (UE/face > LE)
- Aphasia
- hemineglect
generalized deficits of the MCA
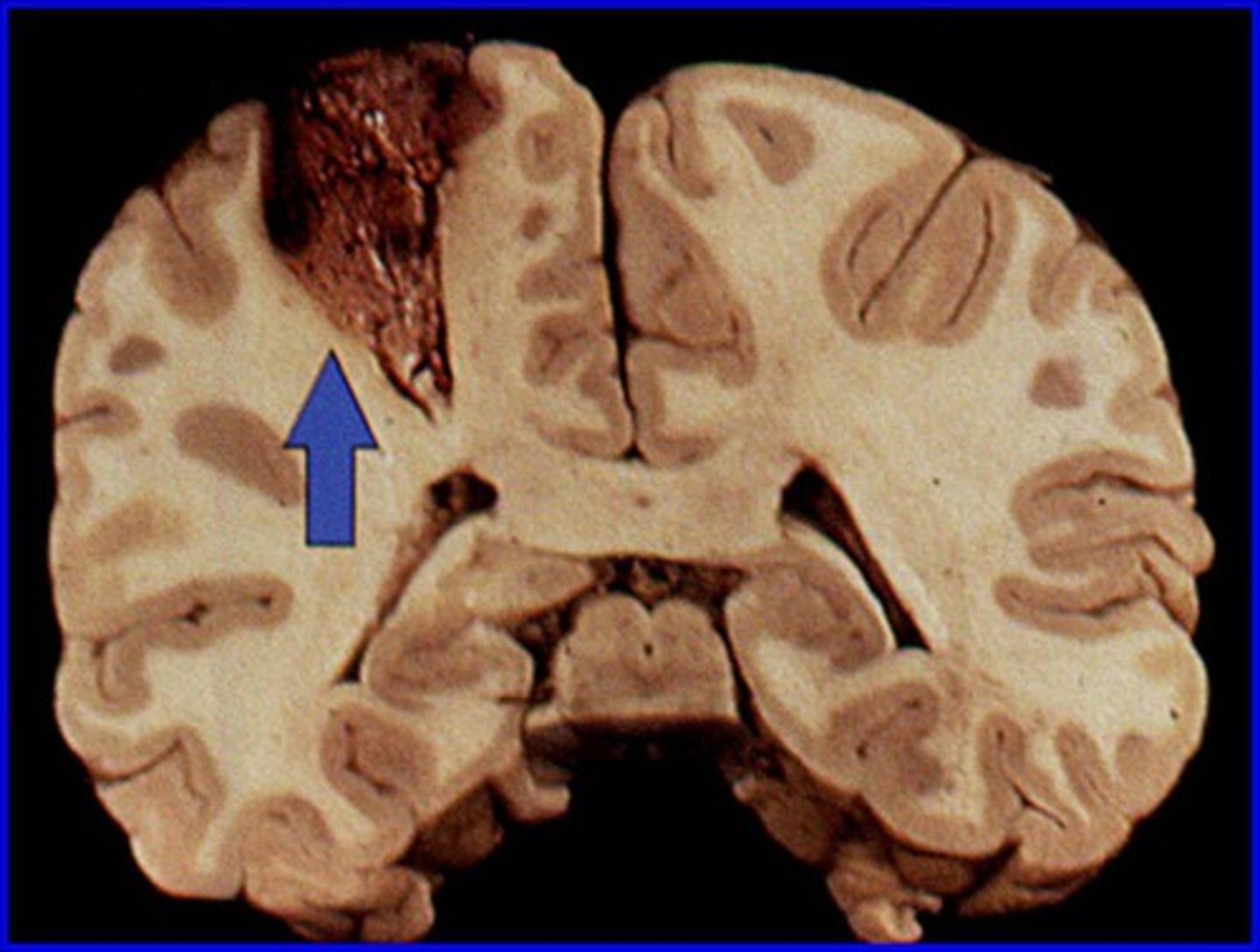
stem infarcts
proximal MCA occlusions that affect all 3 divisions (superior, inferior, deep)
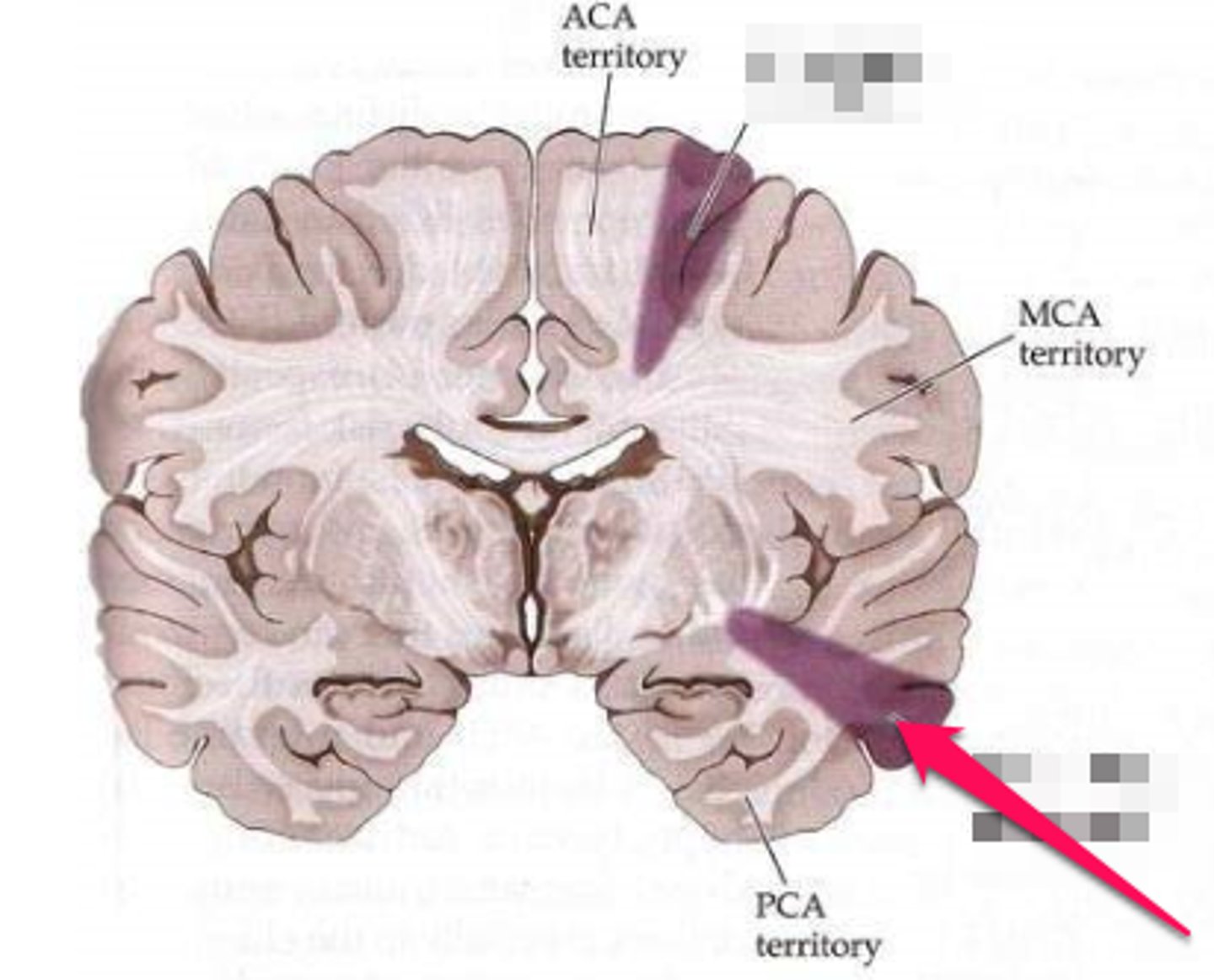
anterior cerebral artery
Infarcts in this artery affect the medial frontal lobes, parietal lobes and anterior basal ganglia
- CL weakness (LE>UE)
- CL sensory loss (LE>UE)
- Apathy, lack of motivation
generalized deficits of infarcts in the ACA
occipital lobes
what does the PCA supply?
- visual deficits, field cuts
- apathy and personality changes
- memory loss
generalized deficits of infarcts in the PCA
watershed zones
Intermediate regions between two adjacent blood vessels.
drop in BP
common cause of infarcts in watershed zones
true
true or false? terminal arteries in the watershed zones are very fine and have high internal resistance
proximal arm and leg weakness
Watershed infarcts in ACA-MCA watershed zone region cause these symptoms:
higher-order visual processing
Watershed infarcts in MCA-PCA watershed zone region cause these symptoms:
long tract signs
signs referable to the pyramidal tracts (corticospinal and corticobulbar), posterior column-medial lemniscus pathway, and the spinothalamic tracts
posterior
long tract signs occur when there is damage to posterior or anterior circulation of the brain
third nerve palsy, cerebellar ataxia
smaller infarcts in the midbrain cause what symptoms?
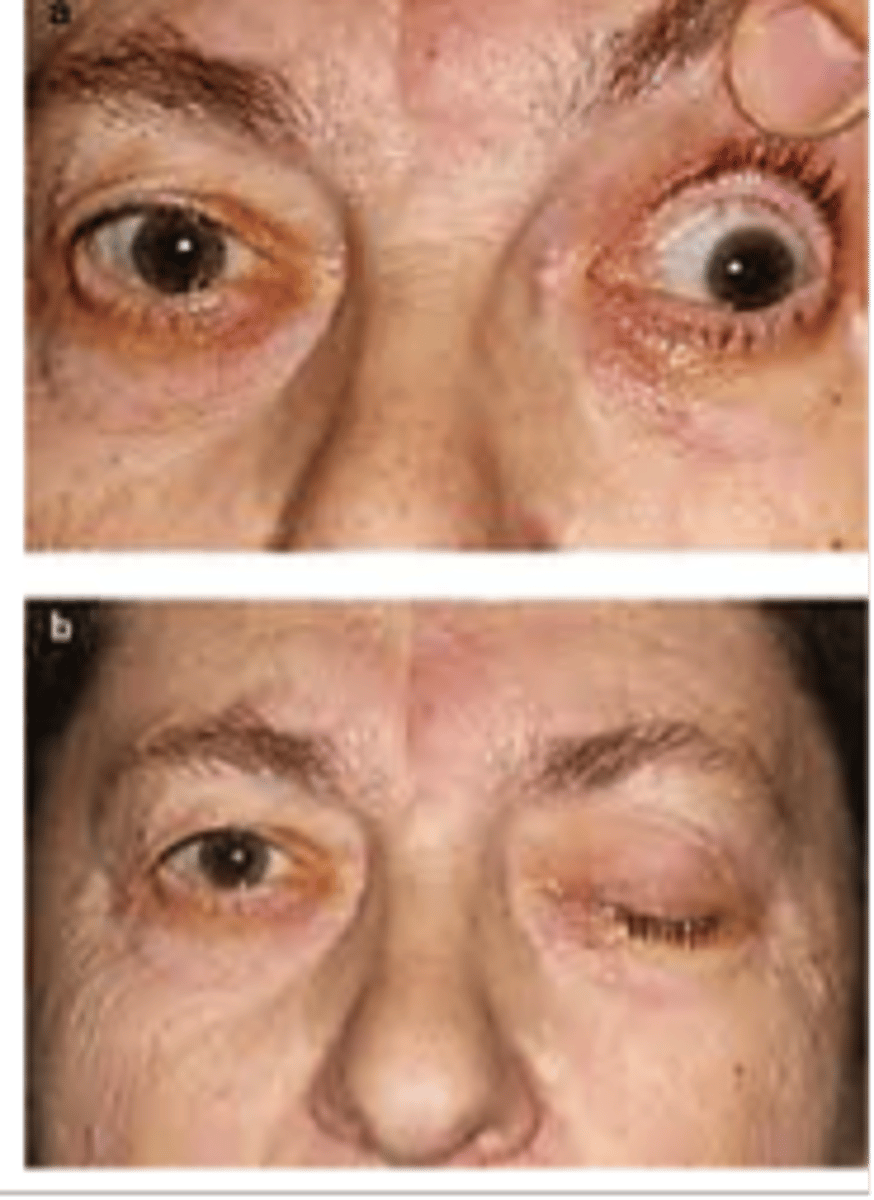
facial, abducens, mandibular palsy
smaller infarcts in the pons cause what symptoms?
lateral medullary syndrome, ipsilateral facial deficits, CL body deficits, deafness, vertigo
smaller infarcts in the medulla cause what symptoms?
ipsilateral cerebellar ataxia, nausea, vomiting, dizziness, vertigo
smaller infarcts in the cerebellum cause what symptoms?
coma
symptoms of larger infarcts in the midbrain
locked syndrome, death
symptoms of larger infarcts in the pontine
death
symptoms of larger infarcts in the medullary
sudden, severe headache
what specific symptoms characterizes a subarachnoid hemorrhage
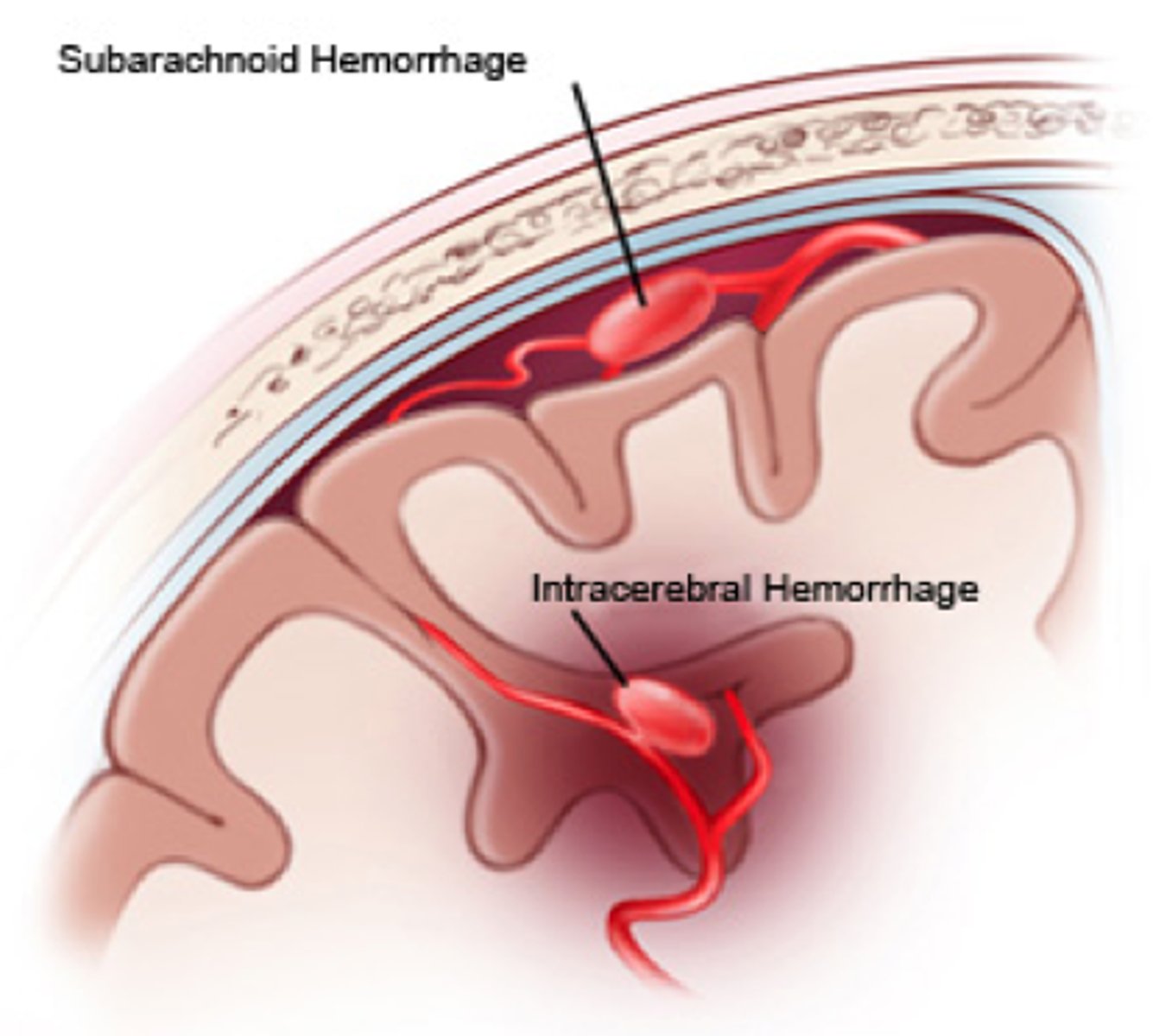
nausea, vomiting, syncope, neck pain, coma, confusion, lethargy, motor weakness, cranial nerve palsies, seizures
additional symptoms of subarachnoid hemorrhage
3 months
around 90% of neurological recovery occurs in what time period following a stroke
neuroplasticity
changes in the synaptic connectivity of the nervous system
true
True or False? The brain is able to change its pattern of synaptic connectivity, which allows us to store new information.
Hebbian plasticity
If a synapse is repeatedly activated at the same time that the postsynaptic cell fires an action potential, that synapse will become "stronger" and increase the likelihood of causing an action potential in the postsynaptic cell; neurons that fire together wire together
increasing strength of existing synapses, unsilencing silent synapses, modifying inhibitory input
what are the 3 ways in which Hebbian plasticity occur?
taken over by nearby neurons
When neurons are lost, how can their function be preserved
cognitive, associative, autonomous
3 stages of motor learning
cognitive
stage of motor learning in which existing neural patterns are used to try to execute a movement carried out by the damaged area(s)
associative
stage of motor learning in which the correct sequence of neural activity
in the cortex has been figured out, but the motor program has not been stored in subcortical structures
autonomous
stage of motor learning in which the motor program is solidified in the cortex and subcortical motor areas
1. align symptoms to infarct location
2. symptom onset suggest suggest the infarct type
3. CT (ideal)
4. MRI (follow-up imaging)
diagnosis of both ischemic and hemorrhagic strokes
30 minutes
How soon can an MRI detect an ischemia
2-6 hours
How soon can an MRI detect an infarct
rapid
embolic infarcts cause slow or rapid symptom onset?
slow
thrombotic infarcts cause slow or rapid symptom onset?
- typically slower onset
- signs of ICP elevation
- same signs as ischemic stroke
symptoms of hemorrhagic stroke
- reduce ICP surgically or w/ mannitol
- avoid glucocorticoids (increases mortality)
Treatment for TBIs
1. severity of impaired responsiveness
2. duration of alt. consciousness
3. duration of posttraumatic amnesia
4. degree of brainstem damage
5. degree of hypoxemia/hypotension
6. cerebral edema & hematoma
7. epilepsy w/in 7 days of injury
8. older age at injury
9. brain injury history
10. ICP increase > 20 mmHg
10 factors that determine prognosis after a TBI