L1: Calcium homeostasis
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
61 Terms
Around 99% of the the total calcium in the body is stored as (1 kg)
Calcium phosphate salts in bones
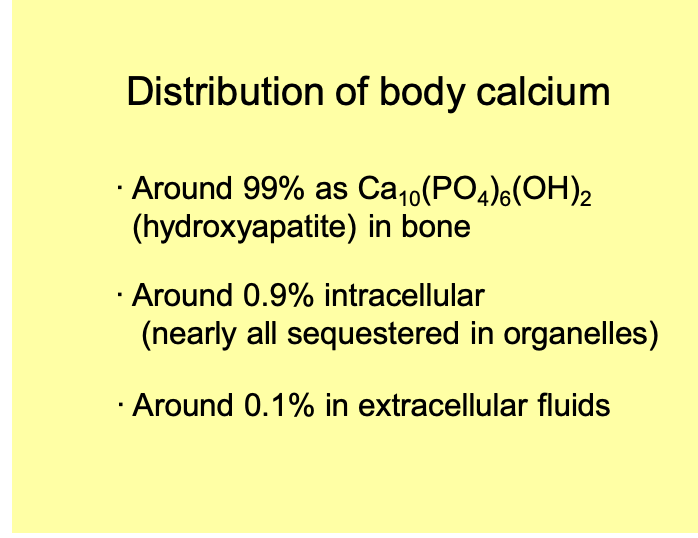
Where is the rest of the calcium?
mainly in cells
sequested inside organelles
THEREFORE→ cytoplasmic [Ca2+] is very low
arounf 0.1 microM
![<ul><li><p>mainly in cells</p></li><li><p>sequested inside organelles</p></li></ul><p>THEREFORE→ cytoplasmic [Ca2+] is very low</p><ul><li><p>arounf 0.1 microM</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/d8d36083-be43-48ea-b211-06a09493d007.png)
What does this very low Ca2+ conc provide
steep gradient for calcium entry
from organelles or from extracellular fluids
Importance of calcium: what happens to extracellular calcium
binds to be fixed
negative charges on the extracellular surface of plasma membranes
altering the actual size of the membrane potential
Importance of calcium: what is the importance of this surface charge screening
calcium stabilizes the membranes of excitable cells
→ making it slightly more difficult to open ion channels
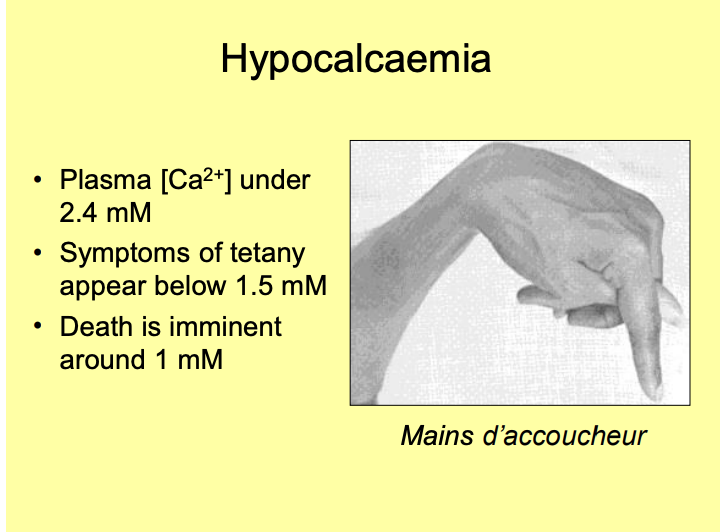
Importance of calcium: Hypocalcaemia
Concentrations <2.4 mM
if it drops to around 1.5mM:
nervous system becomes progressivley excitable
→ tetanic contraction of muscles
SEVERE hypocalcaemia:
tetany of the laryngeal muscles and Asphyxiation
Death is immenant around 1mM
Isn’t this the opposite of what we expect?
Wouldn’t low Ca2+ mean less vesicles so less Neurotransmitter across synapses?
Low extracellular Ca2+
so proteins now have negative charges
charges proteins
more excitable channels
AP to muscles→
Importance of calcium: Hypercalcaemia
Concentration >2.4mM
lead to depression of nervous and muscular activity
If rise ABOVE 3mM
calcium salts precipitate out
E.g calcium phosphate or calcium oxalate kidney stones
SEVERE: fatal → but this is unusual!
painful and unpleasant but not usually fatal!
Importance of calcium: What is Hypercalcaemia a result of
primary hyperparathyroidism
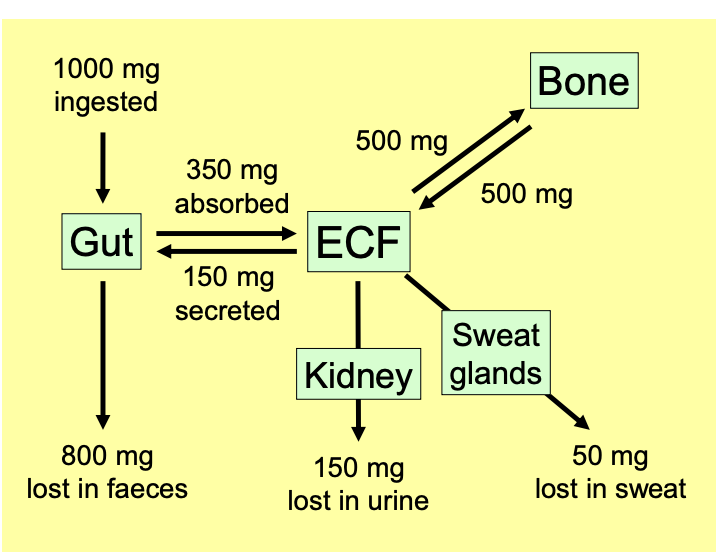
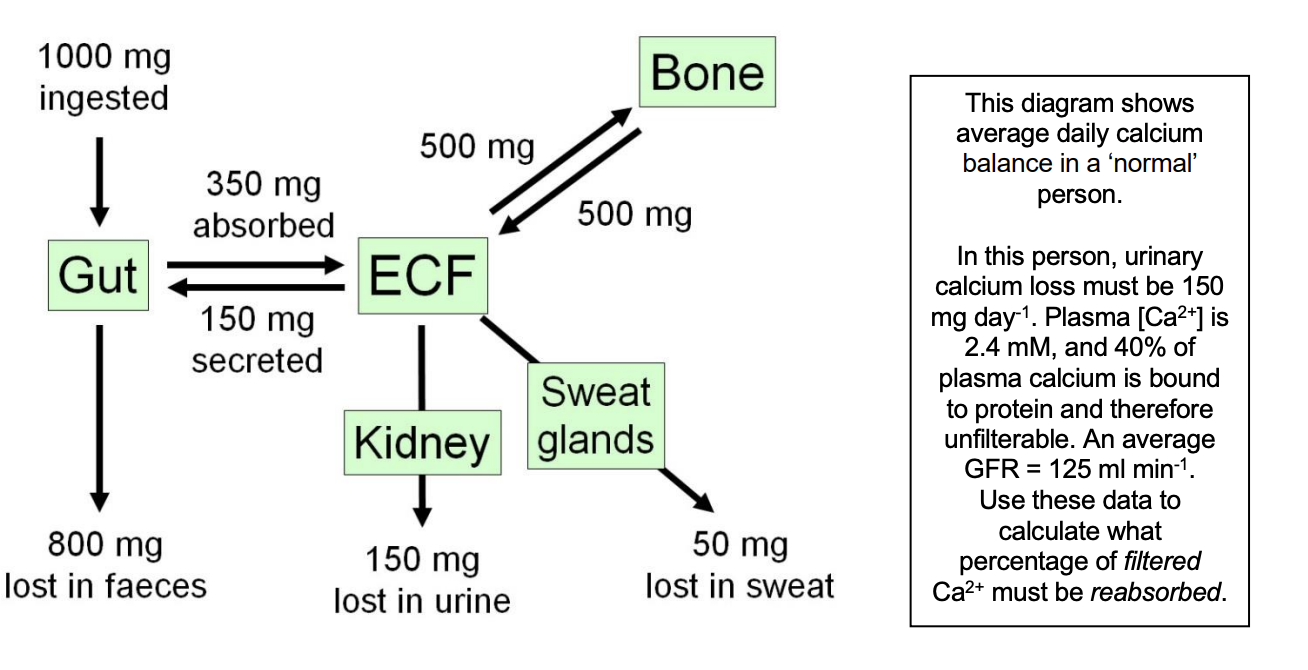
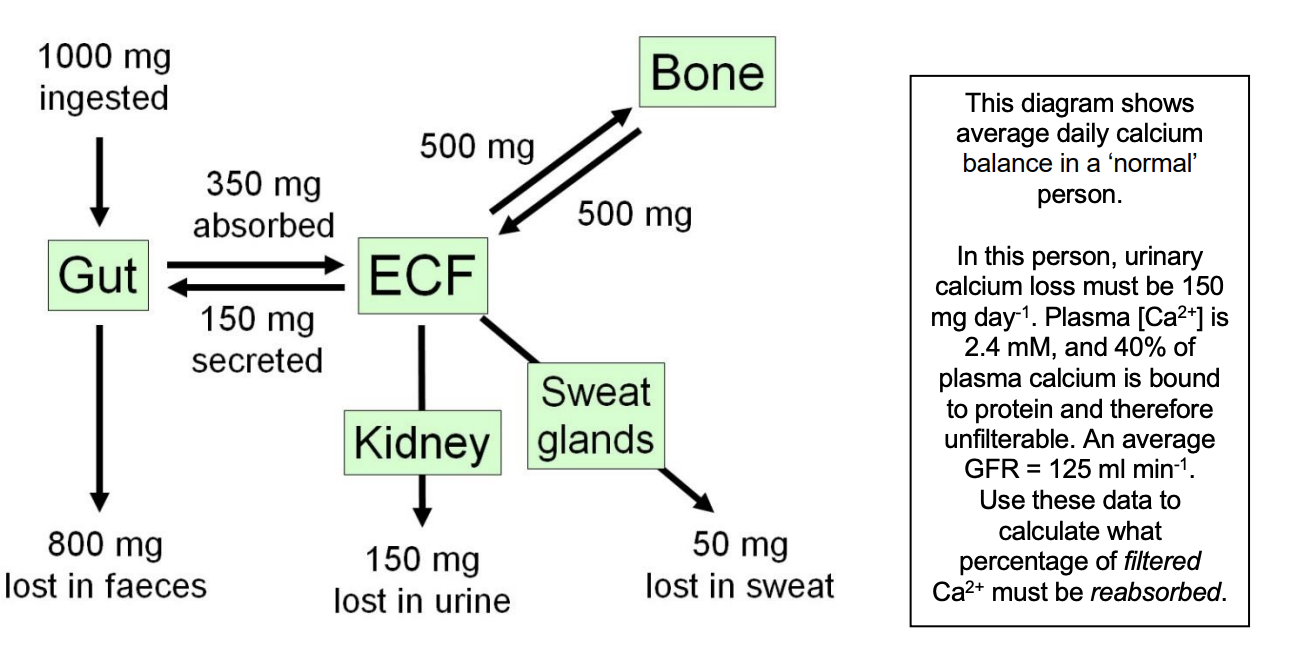
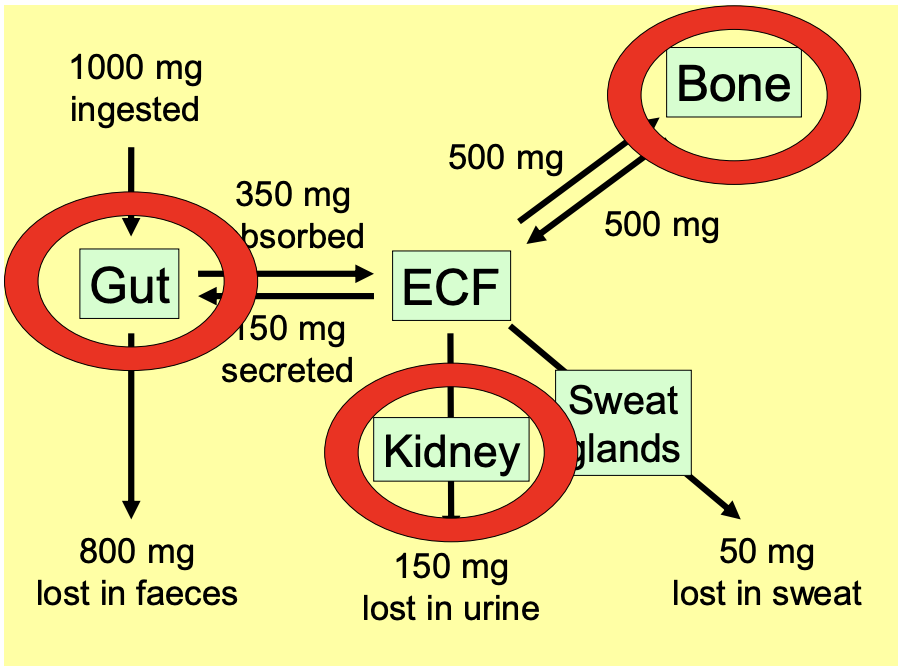
Cycle of plasma calcium levels
1000 mg ingested in gut
350mg Absorbed
150 secreted due to shed of epithelial cells
Bone is constantly making and eording bone
Sweat glands and kidney out
lost in faeces
→ overall a balance
Control of plasma calcium levels: Ca homeostasis involves 3 chemical messengers
parathyroid hormone
calcitriol
calcitonin
Control of plasma calcium levels: these messengers work on targets…
Gut→ absorb more or less calcium
Kidney→ modulate out high rate of reabsorption
Bone→ change balance between erosion and deposition
Control of plasma calcium levels: bone→ daily turnover of bone remodelling can change due to…
Greatly increased by:
bone repair
lactating
Challenges to calcium homeostasis
Pregnancy and lactation
Egg-laying
Poor absorption
Oxalate poisoning
Pregnancy and lactation
At height of nursing:
secrete 500-600 mg calcidum per day into milk
x3 usual daily net intake
Dairy cows:
lactation → milk fever
Pregnant dogs and cats
subject to hypocalcaemic fits
→ eclampsia
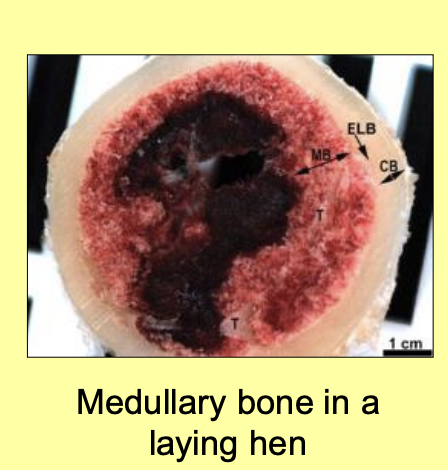
Egg-laying
hen egg contain 2g of Ca
calcium deposited as a special type of bone→ medullary bone
this calcium is mobilized to allow egg production to continue at night
Poor absorption
Vitamin D3 Definiciency
result in difficulty absorbing dietry calcium
Dietry calcium can bind to phytates
in cerals, reducing absorption
Oxalate poisoning
Many plants accumulate oxalate as a defence
Calcium oxalate precipitates out in the gut
excreted
but, unbound oxalate can be absorbed→ leading to calcium oxalate crystals forming within the body too
RESULT→ hypocalcaemia and kidney stones
Sources:
spinach, rhubarb, strawberries
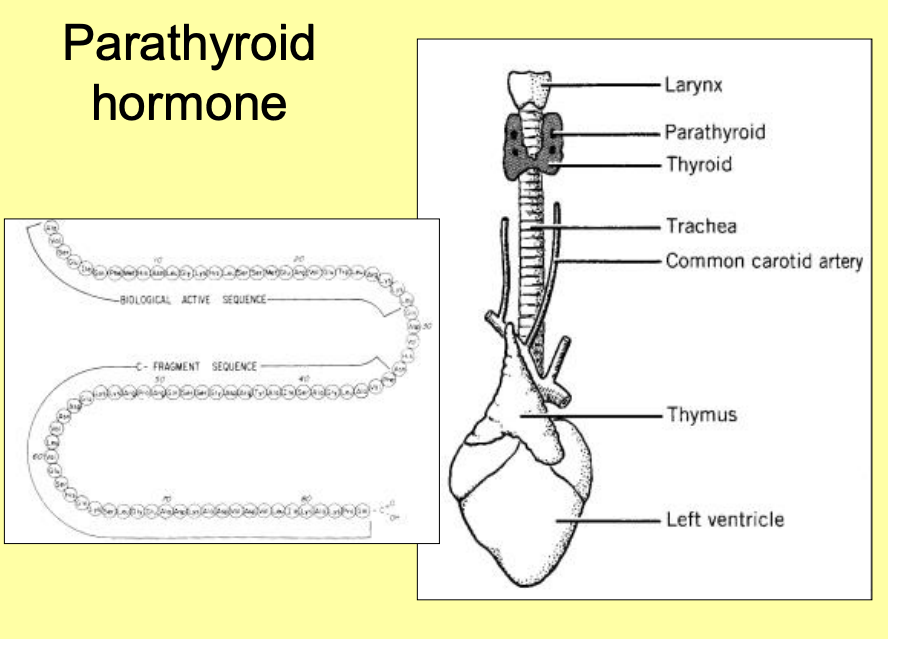
Parathyroid hormone (PTH): features
84 amino acid polypeptide
secreted by parathyroid glands
ESSENTIAL for life
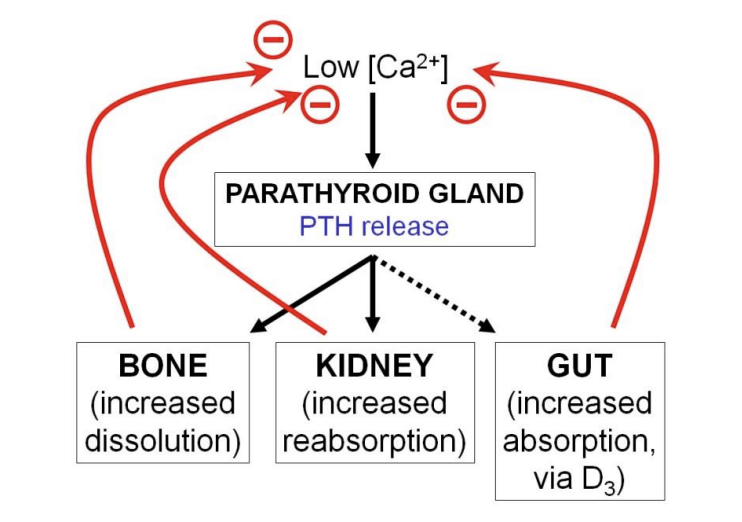
Ways to get calcium
Gut→ increased absorption via D3
Kidney→ increased reabsorption (don’t lose as much)
Bone→ increased dissolution
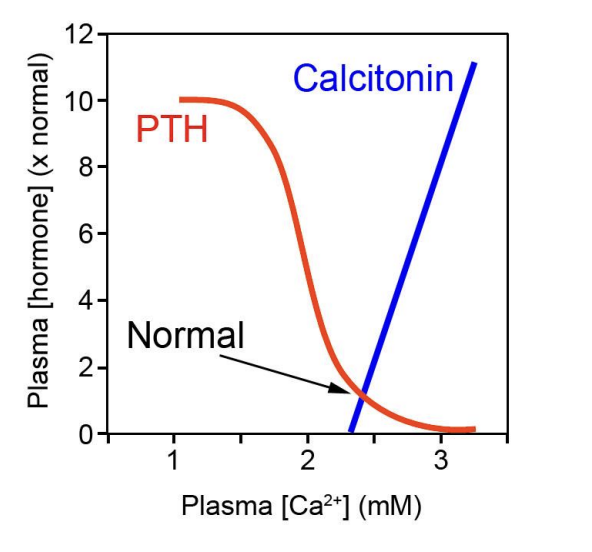
Parathyroid hormone (PTH): features of its release
circadian rhythm to its release
released in pulses
glands are innervated by autonomic nerves
→ help to modulate the rhythms
Parathyroid hormone (PTH): What is the only significant external stimulus to promote increased PTH release
decrease in plasma free calcium levels
Parathyroid hormone (PTH): Response to this
G1 protein linked calcium receptor → in plasma membrane
respond to increased free Ca in the plasma
increasing internal calcium levels
Low extracellular calcium leads to
Low internal calcium levels
→ usually promotes vesicular release:
less Ca2+ causing vesicle release
different SNARE
no nervous input→ WHYYYY???
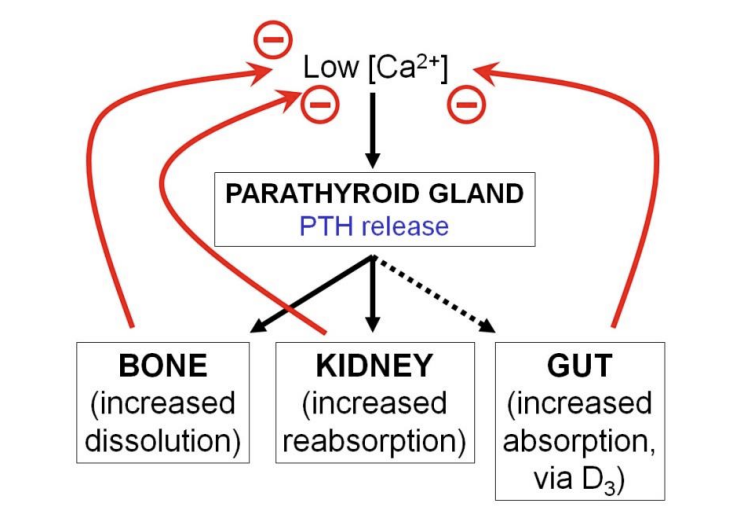
Parathyroid hormone (PTH): Where does PTH work
bone
kidney
The gut→ via vit D3
→ to increase plasma calcium levels in a negative feedback system
PTH receptors are G-protein linked and located on the plasma membrane
PTH and bone: what do osteoblasts and bone remodelling
lay down organic matrix of bone
→ composed of collagen and proteoglycans
Calcium phosphate salts precipitate on the collagen fibres
ultimately→ form hydroxapatite crystals Ca10(PO4)6(OH)2
Some osteoblasts become trapped within the bone and become→ osteocytes
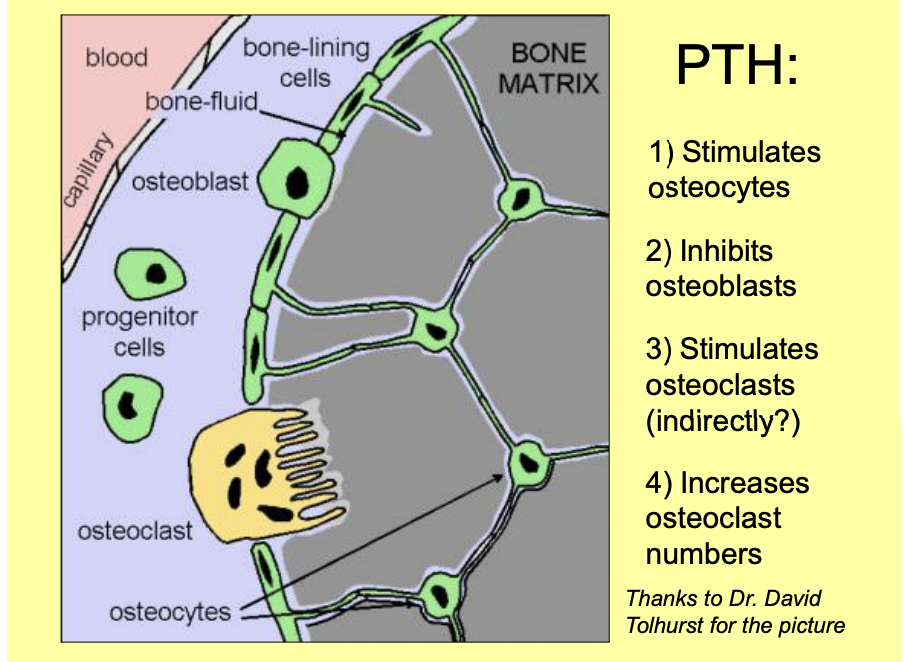
PTH and bone: Osteocytes and osteoblasts Arrangement/strucuture
connected by long processes
running in tiny canals throughout the bone
→ form continuous network of very large surface area
running throughout the bone
over its surface
they separate bone fluid adjacent to the bone surface
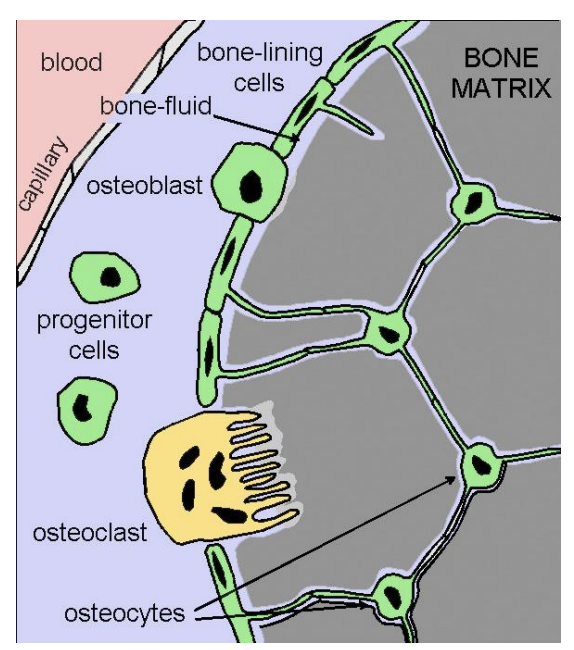
PTH and bone: what is in this bone fluid
high in calcium
from ECF on the other side
PTH and bone: other feature of osteoblasts and cytes
have membrane-bound PTH receptors
PTH and bone: Osteoclasts
separate lineage of cells found within bone
Giant, multinucleated
PTH and bone: Osteoclasts what do they do
release proteolytic enzymes and acids
help to digest an dissolve bone
→ helps in bone remodelling
PTH and bone: what does bone remodelling involve
bone reabsoprtion by the osteoclasts
deposition by osteroblasts
→ about 10% of adult bone is turned over each year
PTH and bone: PTH effects on bone
controversial: osterocytic osteolysis→ describes the erosion of nearby, easily-accessible bone crystals by osteocytes
taking advantage of their large SA
Calcium released
transferred into the ECF
mobilization is rapid→ minutes→ hours
ten min: osteoblasts are inhibited from laying down more bone
ostesoblasts produce a paracrine signal
stimulates the osteoclasts to erode bone
releasing more Ca into the ECF
Effect develops over days or weeks
the signal ALSO stimulates progenitor cells to differentiate into more osteroclasts
PTH increases bone erosion BUT PTH can be injected to treat osteroporosis?!
Because the type of injection of hormone
Injected=> BIG SPIKE
decreases bone erosion
Parathyroid hormone and the kidney: three effects of PTH on the kidney, acting on different parts/functions
Distal convoluted tubule
Proximal tubule
Active vit D3
Note: there is always Ca2+ reabsoprtion in the PCT and LoH
the PTH just tweaks the control
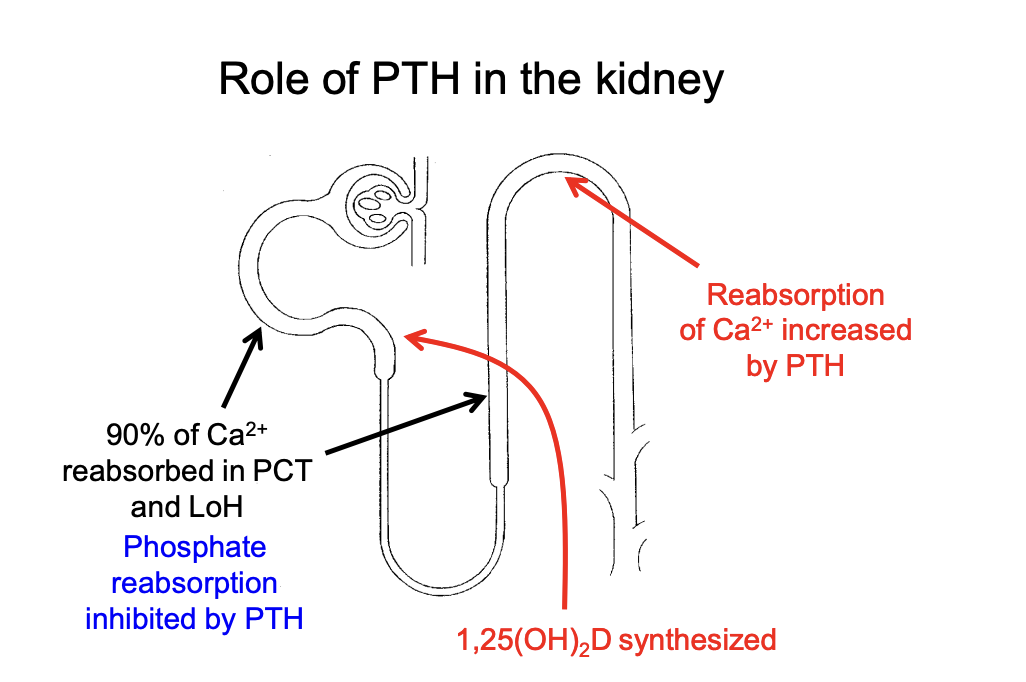
PTH effects levels of what in the kidney?
Promotes Ca2+ reabsorption
Inhibits Phosphate reabsorption
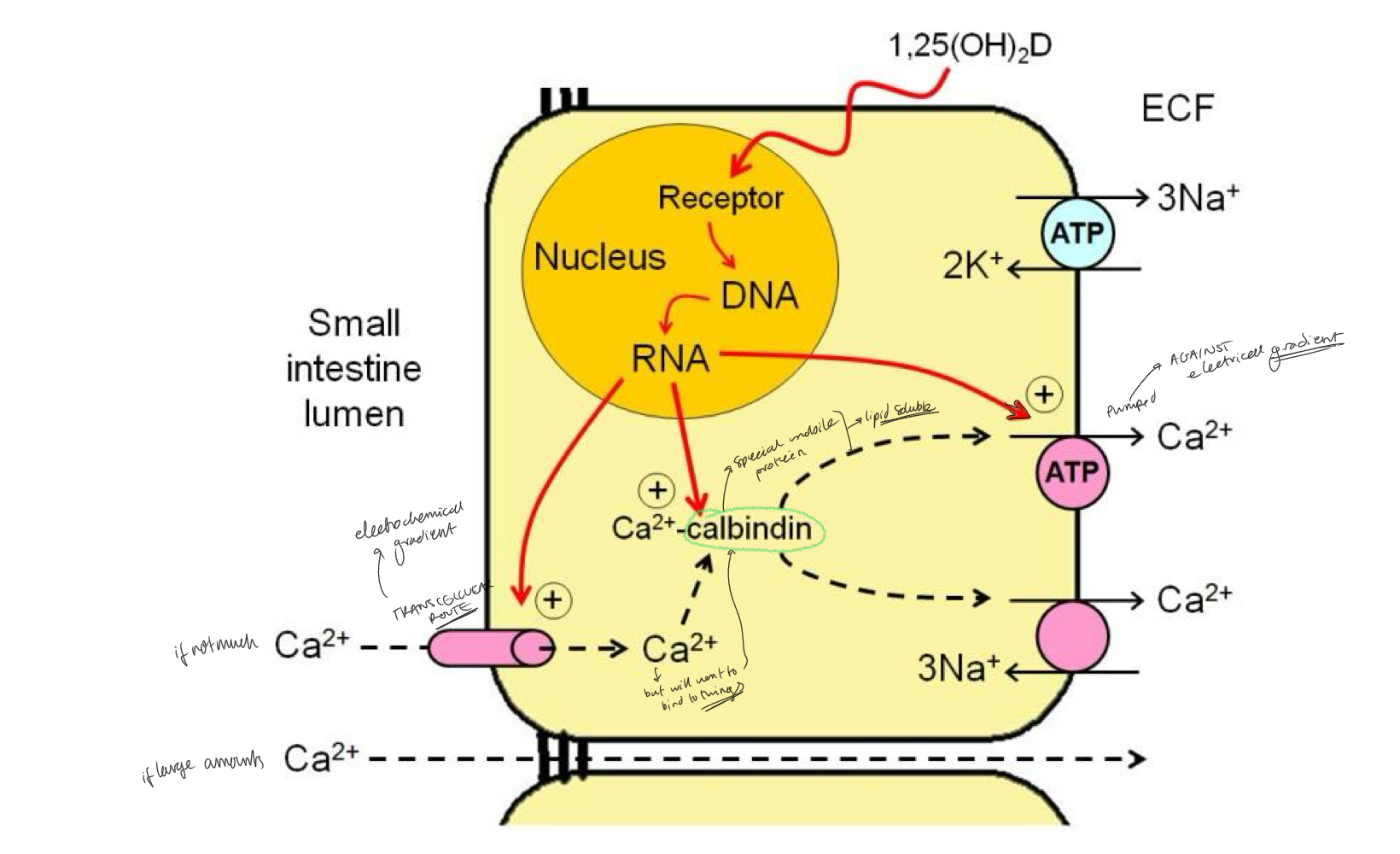
Parathyroid hormone and the kidney: three effects of PTH on the kidney: effect 1
PTH increases active reabsorption of Ca by the distal convoluted tubule of the kidney
The trancellular calcium transport mechanisms resemble those in the gut
effects of PTH are very fast acting within minutes
allow rapid adjustments to blood calcium levels
Parathyroid hormone and the kidney: three effects of PTH on the kidney: effect 2
PTH powerfully inhibit reabsoprtion of inorganic phosphate Pi ions in the proximal tuule
Helps to lower extracellular phosphate levels
inhibits Pi reabsorption so can dump the Pi AFTER is has been eroded by the bone→ OVERALL selects for Ca2+ in this bone erosion
Parathyroid hormone and the kidney: three effects of PTH on the kidney: effect 3
PTH stimulates syntehsis of active vit D3 derivative calcitriol (1,25(OH)2D)
has an important role in the intestinal absorption of calcium
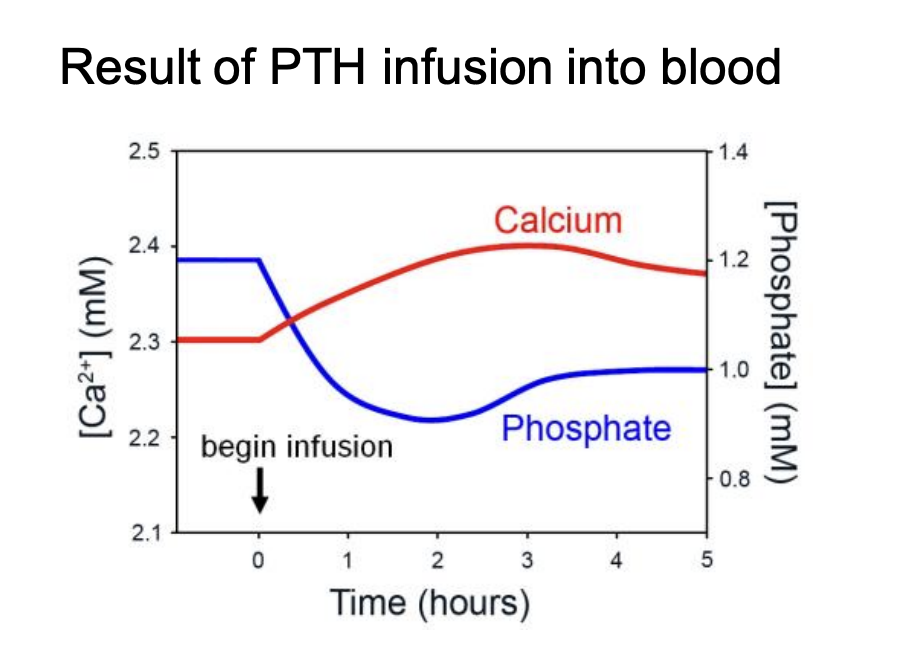
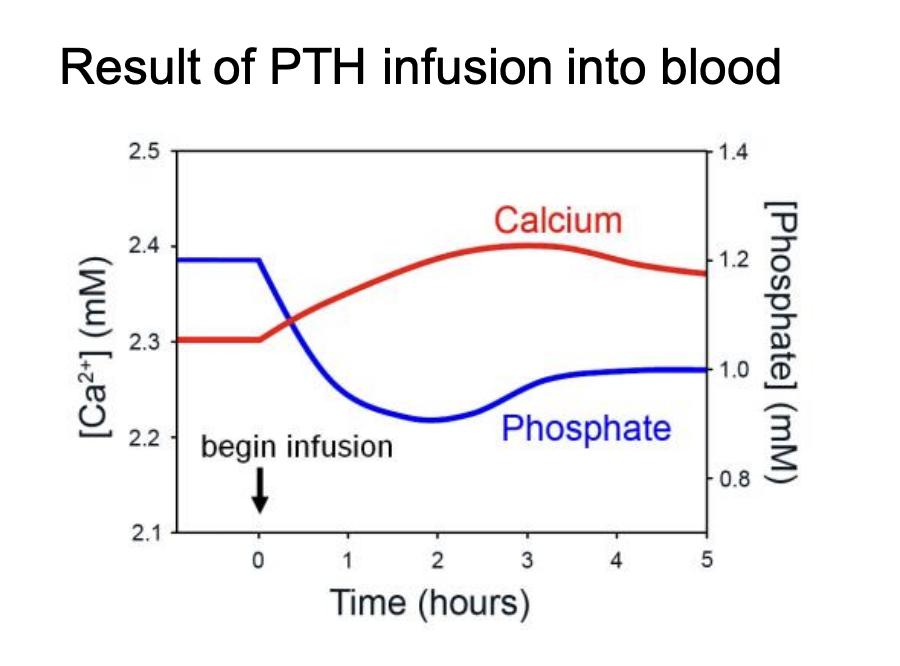
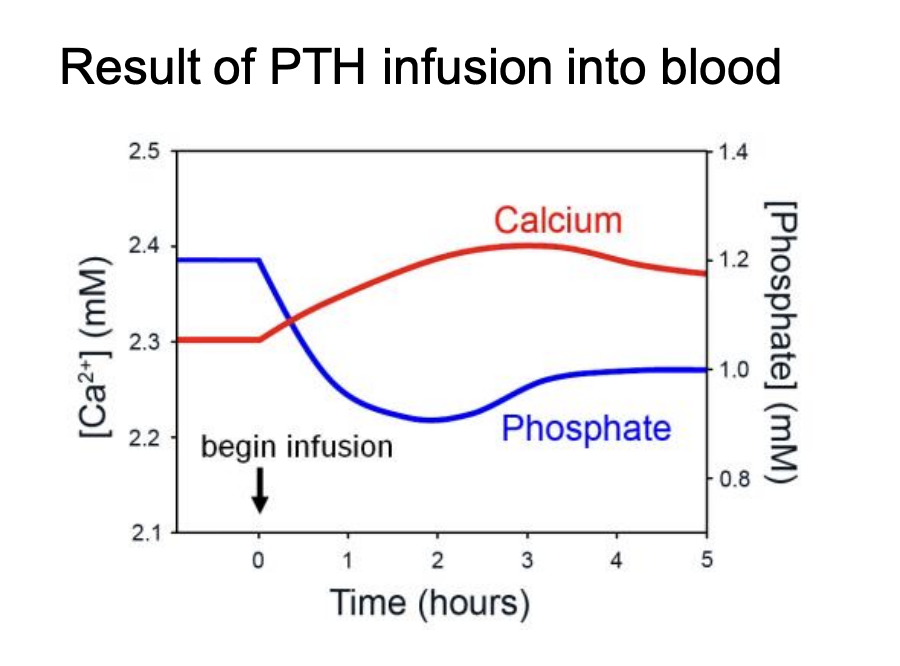
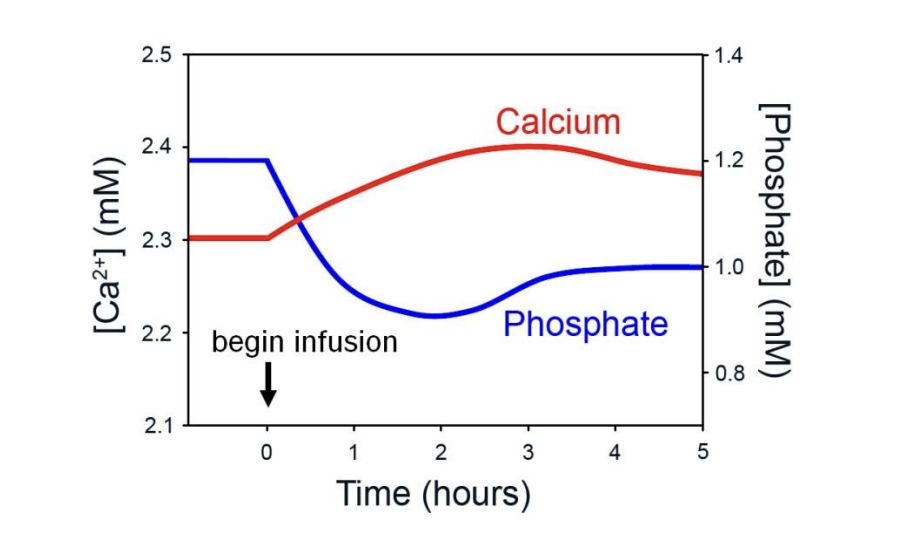
OVERALL: in the presence of PTH
calcium is released from bone
plasma levels rise
Phosphate levels:
although phosphate absorption from gut and bone is increased
this effect is overwhelmed by the increased loss of phosphate
in the urine
ALSO: drop in phosphate→ MORE free Ca because it is no longer bound to phosphate
→ OVERALL: net phosphate is lost
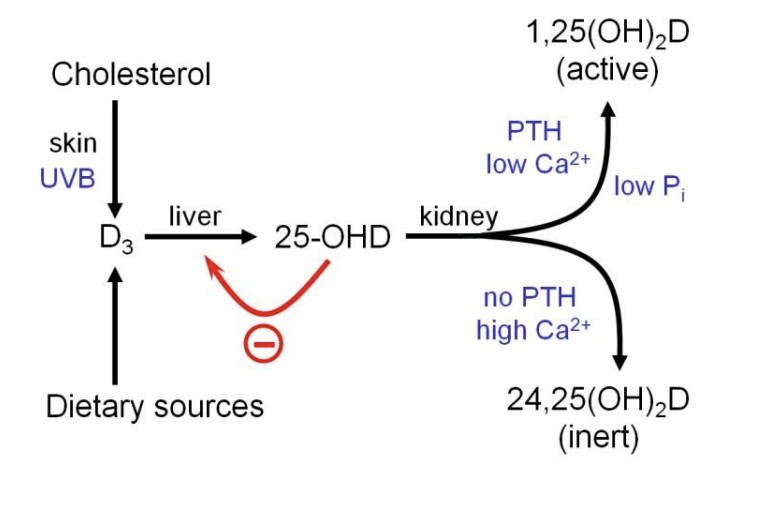
Vitamin D3 and derivatives: Vitamin D3 (Cholecalciferol) how made/obtained
in specialised skin cells→ keratinocytes
from cholesterol
In one step of synthesis: Secosteroid requires exposure to UVB light
Obtained in diet
dairy products and fish liver oils
Vegans→ supplement of the equivalent vit D2→ made of fungal sterol ergosterol
the strucutrue of Vit D3 is close to cholesterol
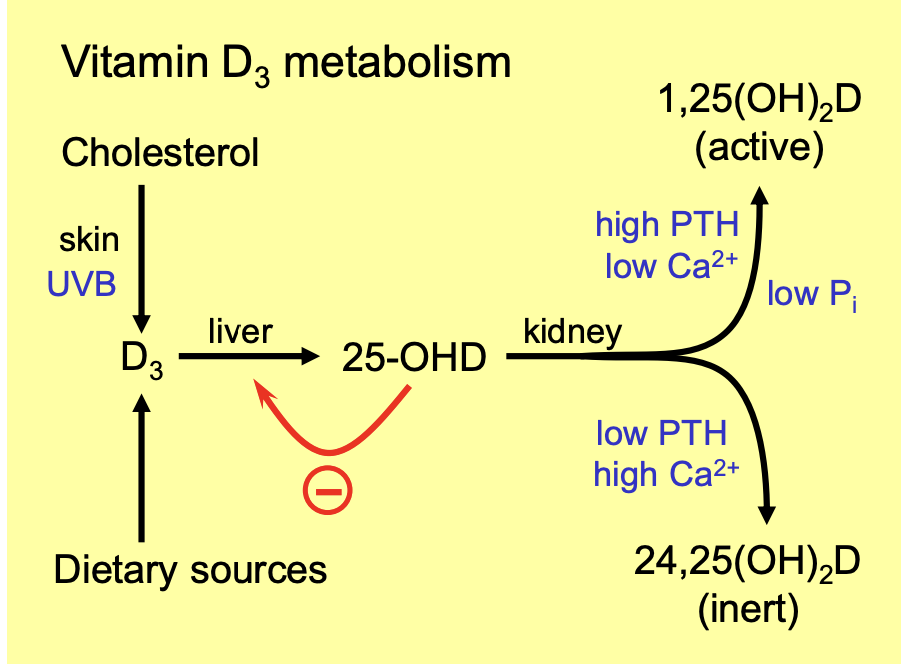
Vitamin D3 and derivatives: where/how stored (in what form)
Stores in liver
used to maintain a constant level of 25-hydroxycholecalciferol (25-OHD) in plasma
after enzymatic conversion subject to feedback control
Proximal tubules of the kidney
taken up under the influence of PTH
decreased clacium leveles/decreased pohsphate levels→ converted to biologically ACTIVE form calcitriol (1,25 dihydroxycholecalciferol; 1,25(OH)2D)
Otherwise→ converted into inert 24,25(OH)2D
25-OHD→ is the main form in plasma bound to proteins
Vitamin D3 and derivatives: Roles of calcitriol are mediated by
ts nuclear receptor
Functions of calcitriol
Increase Ca absorption from gut
promotes erosion of bone
INcreases Ca and phosphate reabsorption from kidney
Vitamin D3 and derivatives: calcitriol most important effect
Increase calcium absorption from gastrointestinal tract:
in the Duodenal epitheial cells→
calcitriol upregulates expression of an apical calcium channel→ calbindin protein
ferries calcium across the cell
basolateral Ca2+-ATPase pumps it out into extracellular fluid
Phosphate absorption from the gut is also increased
Vitamin D3 and derivatives: calcitriol minor roles…
promote bone erosion
increasing both Ca and phosphate reabsorption from the kidney
In what ways are vitamin D3 less like a ‘true’ vitamin and more like a steroid hormone?
kinda both
Vitamin→ its is REQUIRED for normal physiologyical process and cannot be made
Steroid hormone→ chemmical messenger from cholesterol, travel in the blood and works on intracellular receptors and affects gene expression
Vitamin D deficiency: Rickets
in children dietary lack of vitamin D3 is the commonest cause of rickets:
plasma calcium do not drop substantially because of PTH secretion
which erodes the bones to maintain plasma levels
but the weakened bones become distorted
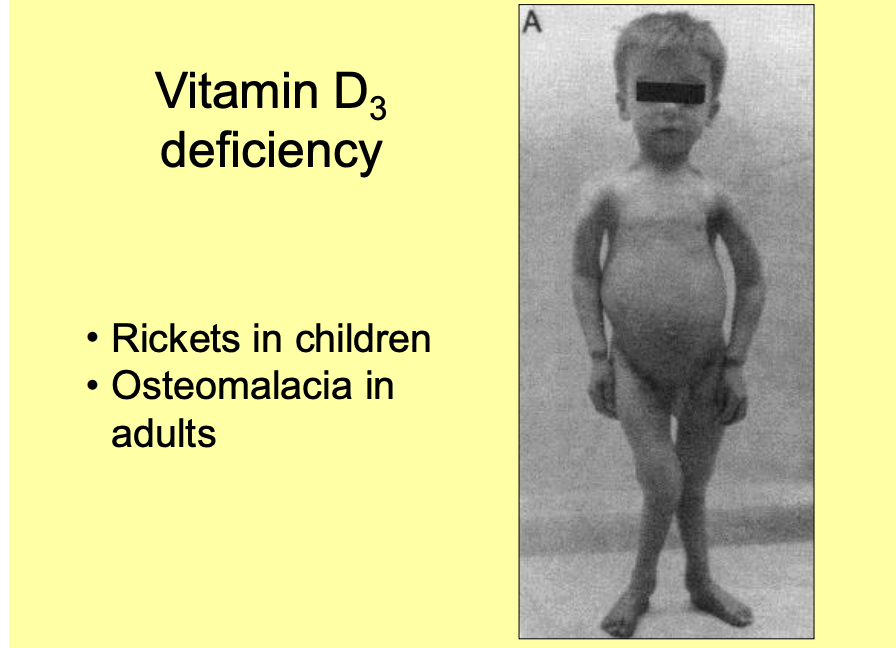
Vitamin D deficiency: Adult version of rickets
after grwoth-plates fuse
osteromalacia
Factors affecting Vit D3 availability
Latitude, air pollution, clothing, sunblock
Vegan diets
Women vs men??→ Women are paler?→ need more Ca for pregnancy?
Steatorrhoea→fatty faeces→ lose D3 with as fat soluuble→ decrease Ca2+too coz not enough fat
What is calcitonin
32 amino acid polypeptide hormone
secreted by the C-cells (clear cells) of the thyroid
Primary stimulus of calcitonin secretion
increased plasma [Ca} levels acting directly on the C-cells
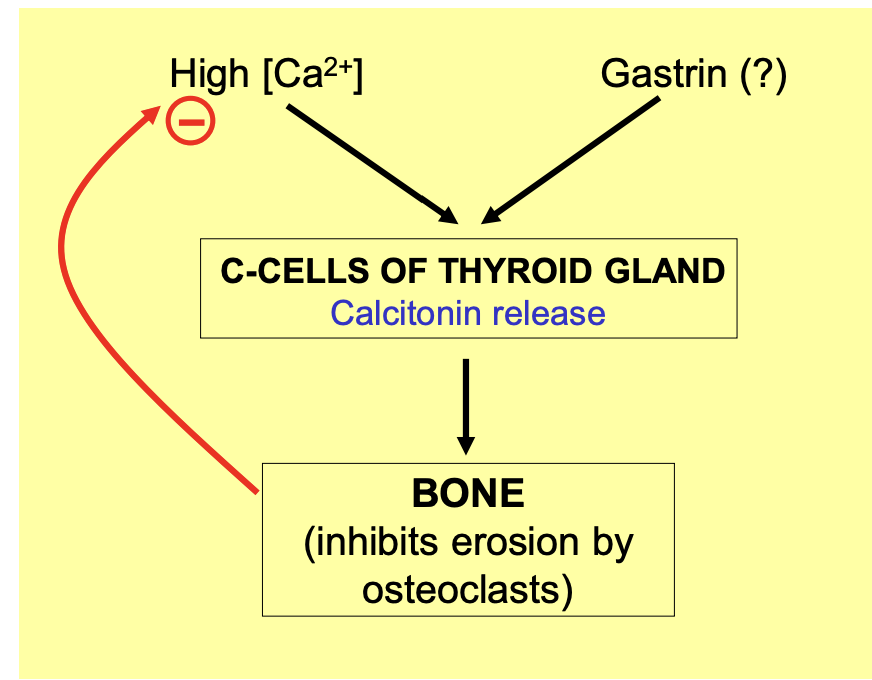
Effect of calcitonin
reduces plasma [Ca]
by rapidly inhibiting the erosion of bone by osteoclasts
shifting the balance in favour of deposition
![<ol><li><p>reduces plasma [Ca] </p></li><li><p>by rapidly inhibiting the erosion of bone by<strong> osteoclasts</strong></p></li><li><p>shifting the balance in favour of deposition</p></li></ol><p></p>](https://knowt-user-attachments.s3.amazonaws.com/834a98b2-99c1-4e08-9e25-2599273de376.png)
Gastrin→ what does it do
causes increased calcitonin secretion
might help as an anticipatory response to the calcium
that will be absorbed as part of the meal
but this is controversial as the concentrations needed are not physioligcally possible
It has been suggests that calcitonin helps to…
Stabilise Ca2+ homeostasis when turnover between plasma and bone is unusually high
e.g during growth or lactation
To protect against excessive bone erosion
However…
some argue that calcitonin has no important physiological effcts in humans
→ may be a vistigial hormones→ when the thyroid is removed→ still get normal calcitonin
How else can humans deal with hypercalcaemia? Why is calcitonin more important in marine fish?
Caclitonin is used more or less depending on the environment of the organism
→ e.g marine fish
importnat to stop hyper Ca due to the gills being exposed to water
which will be high in Calcium
so therefore it is importantn in controlling the Ca2+ levels
Phosphate homesostais: phosphate importance
essential as part of the inorganic structure of bone
As part of many organic molecules
Phosphate homesostais: phosphate in the plasma
present mainly in the forms HPO42- and H2PO4-
Phosphate homeostasis and calcium
phosphate homesostasis is closely linked with that of calcium
You have enough information from these notes for you to work out the body’s response to low phosphate levels. Draw out a flow diagram to illustrate the processes involved. Consider the effects on calcium levels too!
put this here lol
Exam questions
Compare the roles of parathyroid hormone, vitamin D and calcitonin in the regulation of blood calcium levels (NST 1B 1994)
What mechanisms contribute to the stability of the plasma concentration of free calcium ions? (NST 1B 1996)
Explain why parathyroid hormone, but not calcitonin, is essential for life (NST 1B 2000)