I&I week 9 Inflammatory mediators and pharmacologic treatment
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
What are the two types of chemical mediators of inflammation?
Cellular derived
Plasma derived
What is cellular derived chemical mediators?
Pre-made mediators released from cells
What are plasma derived chemical mediators?
Soluble cascade system with activated subunits that have wide ranging inflammatory affects
What are the 4 types of cell-derived chemical mediators?
Lipid Mediators
Cytokines and chemokine
Vasoactive amine
lysosomal components within inflammatory cells
Lipid mediators lead to what type of pathway?
Arachidonic acid pathway
What is produced when the phospholipid bilayer is broken down by phospholipase A2?
Arachidonic Acid
What enzymes are used to breakdown Archidonic acid to produce Thromboxane and Protaglandins?
Cyclooxygenase 1 and 2
What are the products of Archidonic acid being broken down by Cyclooxygenase 1 and 2?
Thromboxane and prostaglandins
What enzyme is used to breakdown arachidonic acid into Leukotrienes?
Lipoxygenase
What is the product of arachidonic acid being broken down by Lipoxygenase?
Leukotrienes
What does does Thromboxanes express?
COX-1
What is COX-1?
Is expressed in healthy animals
Cytoprotection of mucosal cells and renal function but is increased during inflammation
What does Prostaglandins express?
COX-1
COX-2
What is COX-2?
Expressed during inflammation
Thromboxanes expressed during inflammation cause what?
Vasoconstriction
Platelet aggregation
Prostaglandins expressed during inflammation cause what?
Fever
Pain
Loss of function
Vascular response
Cellular Response
What does leukotrienes cause?
Smooth muscle contractions
vascular response
cellular response
mucous secretion
Leukotrines are seen in what two major immune responses?
Allergies and hypersensitivities
What are the therapeutic goals of lipid mediators?
Reduce inflammation
What are the therapeutic targets for lipid mediators?
Receptors
Iron channels
Pumps
Enzymes
What are the 4 types of enzyme inhibitors?
Phospholipase A2-inhibitors
COX-inhibitors
LOX inhibitors
Prostaglandine Receptor blockers
What drugs are used as a Phospholipase A2-inhibitor?
Glucocortiosteroid
What drugs are used as a COX-inhibitors?
Non-steroidal anti-inflammatory drugs
What are the three types of non-steroidal anti-inflammatory drugs?
COX-1 selective
COX-2 selective
COX-1/2 preferential
what is an example of a preferential or selective COX-1 inhibitor?
Acetyl salicylic acid
What are examples of non-specific cox inhibitors?
Carprfen
Flunixin meglumine
Phenylbutazone
Tolfenamic acid
What does it mean to be preferential to cox-2?
the drug prefers cox to at a 60/40 split meaning it will still bind to both but not at equal rates.
What type of binding does acetyl salicylic acid have?
irreversible binding
What are examples of preferential or moderately selective COX2 inhibitors?
Meloxican
Deracoxib
Etodolac
What are examples of highly selective COX-2 inhibitors?
Fibrocoxib
Robenacoxib
What is an example of Cox3 inhibitor?
Acetaminophen
What are the NSAID pharnacokinetics?
Weak acids
Reasonable Vd
Hepatic metabolism
Enterohepatic recirculation
What are the adverse effects of NSAIDS?
Stomach ulcerations
Kidney Damage
Hepatotoxixity
Slow bone healing
Buddy is a 9 year old, neutered lab retriever. His owners report that he has been slowing down on walks, has difficulty getting up from a lying position, and seems to being pain at times. What body system is likely involved?
Skeletal/muscle system
Buddy is a 9 year old, neutered lab retriever. His owners report that he has been slowing down on walks, has difficulty getting up from a lying position, and seems to being pain at times. What diagnostics do you want to run to figure out a diagnosis?
PE
X-rays
NSAID panel
Buddy’s owners are looking for ways to help manage his condition and improve his QOL. What is the therapeutic goal when treating buddy?
NSAIDS
pain management
Joint supplements
Buddy is diagnosed with osteoarthritis. What pathway within the arachidonic acid breakdown is primarilu associated with the clinical sign (pain, loss of function) seen in buddy?
Prostaglandins
The owners are looking for ways to help manage buddyes condition and improve his QOL. What is the most appropriate initial treatment recommendation for Buddy’s osteoarthritis?
Prescribe a non-steroidal anti-inflammatory drugs (NSAID)
Before beginning Buddy on a regimen of NAIDS it is recommended that a plasma biochem and urinalysis be preformed. What organ should be examined and why?
Liver- drugs metabolized in the lover and can cause hepatotoxicity
Kidneys- drugs can cause renal toxicity and damage to kidney due to lack of blood flow
What are alternatives can be used in the treatment of buddy?
Exercise
Weight loss
Use of prostaglandine receptor blockers
What is the mechanism of prostaglandine receptor blockers?
EP4 receptor is blocked
Why is EP4 receptor important when using prostaglandine blockers?
EP4 is the primary mediator for PG sensitization and sensory neurons and PG elicited inflammation
What is the routes of administration for Glucocorticouds?
IV
IM
Inhalation
Topical
Local
What are the Glucocorticoid Pharmacokinetics?
Large Vd
Liver metabolism
Inactive metabolites are eliminated via the kidneys
What drug needs to be converted to be given to cats and horses?
Prednisone
What are the three types of formulations of Glucocorticoid?
Succinate/phosphate
Acetate/Phenylpropionate/isonicotinate
Acetonide
What is an example of a succinate glucocorticoid?
Prednisolone sodium succinate
What is an example of an acetate glucocorticoid?
Prednisolone Acetate
What is an example of an phenylproprionate?
Dexmethasone phenylproprionate
What is an example of an acetonide?
Triamcinolone acetonide
What are the adverse effects of glucocorticoids?
Vomiting diarrhea
bodyweight gain or loss
polyuria and polydipsia
delayed wound healing
immunosuppression and predisposition to infection
Zorro, a 12-year-old Warmblood gelding, presents for an evaluation of chronic cough and exercise intolerance. The horse has a history of respiratory issues during the hay feeding months over the past few years. Physical examination reveals bilateral expiratory wheeze and flared nostrils at rest. What body system is likely involved?
Respiratory system
Zorro, a 12-year-old Warmblood gelding, presents for an evaluation of chronic cough and exercise intolerance. The horse has a history of respiratory issues during the hay feeding months over the past few years. Physical examination reveals bilateral expiratory wheeze and flared nostrils at rest. What diagnostics do you want to run to figure out a diagnosis?
PE, scope down nose, x-rays
Zorro, a 12-year-old Warmblood gelding, presents for an evaluation of chronic cough and exercise intolerance. The horse has a history of respiratory issues during the hay feeding months over the past few years. Physical examination reveals bilateral expiratory wheeze and flared nostrils at rest. It seems like the diagnosis is asthma. What type of hypersensitivity is associated with equine asthma?
Type 1
What pathways within the Archidonic acid breakdown is primarily associated with the clinical signs seen in zorro?
Prostaglandins and Leukotrienes
What is the therapeutic goal for zorro?
Block phospholipase A2 which will block both pathways so prostaglandins and leukotrienes cannot be produced.
What is the most appropriate treatment for Zorro?
Systemic glucocoticoids
Are adverse effects from glucocorticoids every seen in Horses?
Very rarely seen in horses with athsma
Which cytokine does fever, neutrophilia, and activation of phospholipase A2, stimulate acute phase proteins?
IL-1
What cytokine does shock, activation of neutrophils and endothelial cells, stimulate the production of other cytokines?
TNF-Alpha
What cytokine fosters a shift from acute to chronic inflammation, and activates macrophages and lymphocytes?
INF-gamma
What do IL-1, TNF-Alpha, and INF-gamma have in common?
Stimulate the immune system
What cytokine does immune system suppression?
IL-10
What chemokine attracts neutrophils?
IL-8
What chemokine attracts Eosinophils?
Eotaxin
What chemokine attracts Lymphocytes
CCL1
CCL2
CCL17
CCL22
What chemokine attracts monocytes?
MCP-1
CCL2
What is believed to increase the efficiency of leukocytes and iron sequestration, impair replication of microorganisms, and stimulate acute-phase inflammatory responses including resting?
Fever
What is a sign of inflammation but not necessarily infection?
Fever
High fevers occur during what kind of infections?
Acute
Low grade fevers occur during what kind of infection?
Chronic
What are the 3 types of vasoactive amines?
Histamine
Serotonin
Nitric oxide
Where is vasoactive amines produced?
WBC
Endothelial cells
Platelets
What does vasocative amines cause?
Vasodilation locally or systemically
Why are lysosomal components within inflammatory cells important?
Intracellular digestion and extracellular digestion of pathogens, dead cells, and debris
What are the types of inflammatory cells?
Neutrophils and Macrophages
What inflammatory cells phagocytosis?
Neutrophils and Macrophages
What inflammatory cells cause degranulation?
Neutrophils, Eosinophils, Mast cells, and Basophils
What groups of lysosomal components are most likely to contribute to liquefactive necrosis?
Enzymes
Reactive oxygen species
What enzymes have lysosomal components?
Proteases
Esterases
Nucleases
Collagenases
Histamineases
What are enzymes with a lysosomal components function?
Non-specific break down of cellular structures
What are antimicrobial peptides that have lysosomal components?
Defensin (neutrophils)
Major basic protein (eosinophils)
What are characteristics of antimicrobial peptides that have lysosomal components?
Specifically target pathogens
Many mechanisms of killing still not known
What are ROS cells that have lysosomal components?
Free-radicals
What cells produce free-radicals?
Inflammatory cells
Endothelial cells
What is a characteristic of ROS?
High concentration they are damaging to pathogens and host cells
Dr. Fonseca’s experimenting in the lab with a new workout powder. He wants to increase blood flow to his pecs. Which mediator would be least useful to drop in his orange juice?
Thromboxane
The complement system is comprised of activated proteins that do what?
Attack pathogens directly
Enhance vascular and cellular inflammatory responses
What complement proteins are anaphylatoxins?
C3a and C5a
What do anaphylatoxins cause?
Vascular and cellular response
What complement proteins are opsonization?
C3b
What is the function of opsonization?
Enhanced phagocytosis by neutrophils and macrophages
A 5 year old gelding presents with a recurring fever, lethargy and back pain. Cerebrospinal tap is pictured. Pure culture of streptococcus is isolated from the fluid. Laboratory studies show C3 levels are at 25% normal with normal levels of C2.C5.C7. What would this patient be at increased risk for developing bacterial meningitis?
Reduced activity of the alternative and common pathway.
decreased MAC attack
Decreased anaphylatoxins
decreased opsonins
A 5 year old gelding presents with a recurring fever, lethargy and back pain. Cerebrospinal tap is pictured. Pure culture of streptococcus is isolated from the fluid. Laboratory studies show C3 levels are at 25% normal with normal levels of C2.C5.C7. What if the defect was in C1 levels?
Loss of classical pathway
What is the Fibrinolytic system?
Activated at the same time as the clotting cascade to degrade fibrin and blood clots
Plasmin also cleaves C3 of the complement system
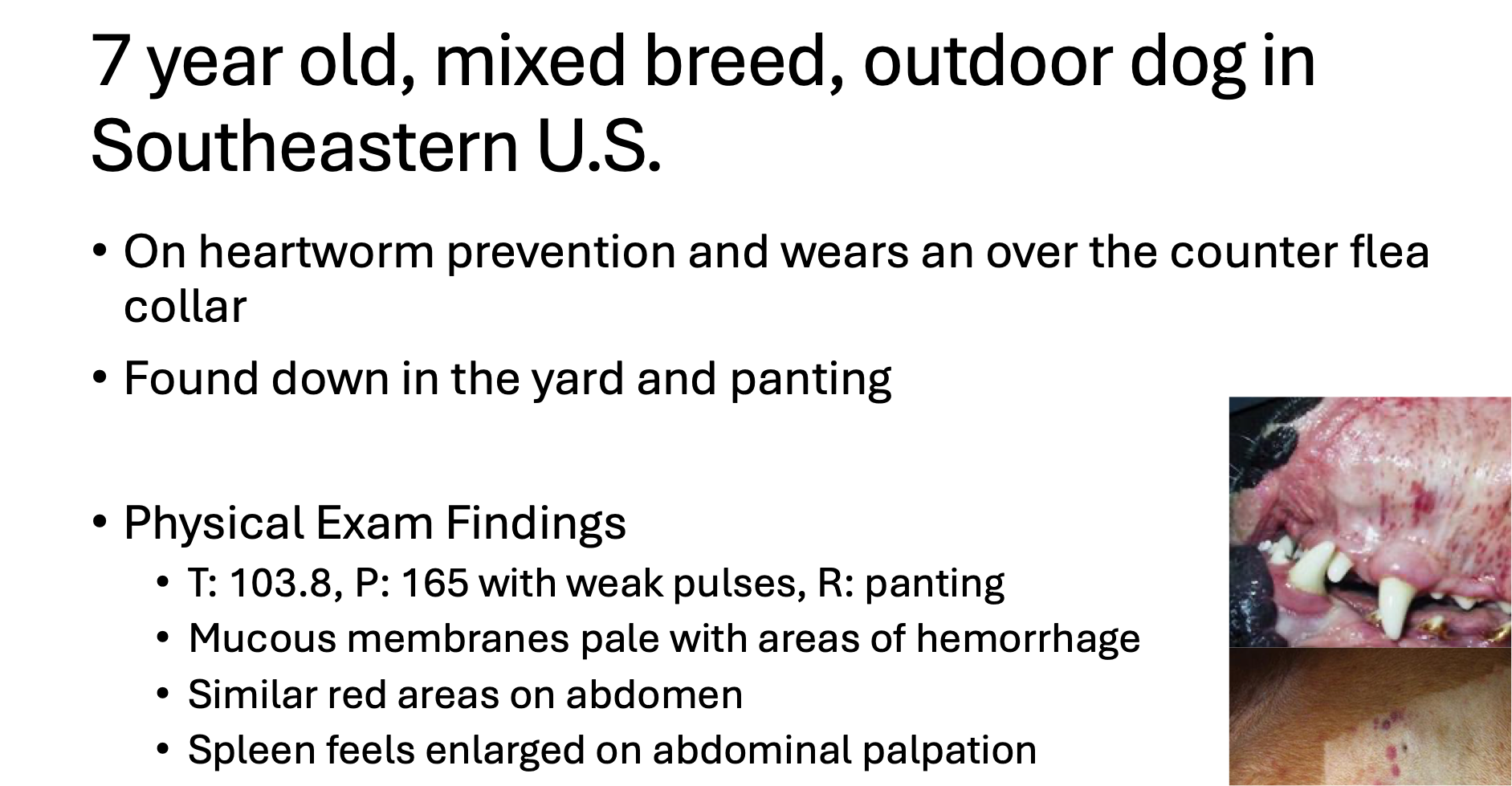
What body system are you worries about in this dog?
Cardiovascular
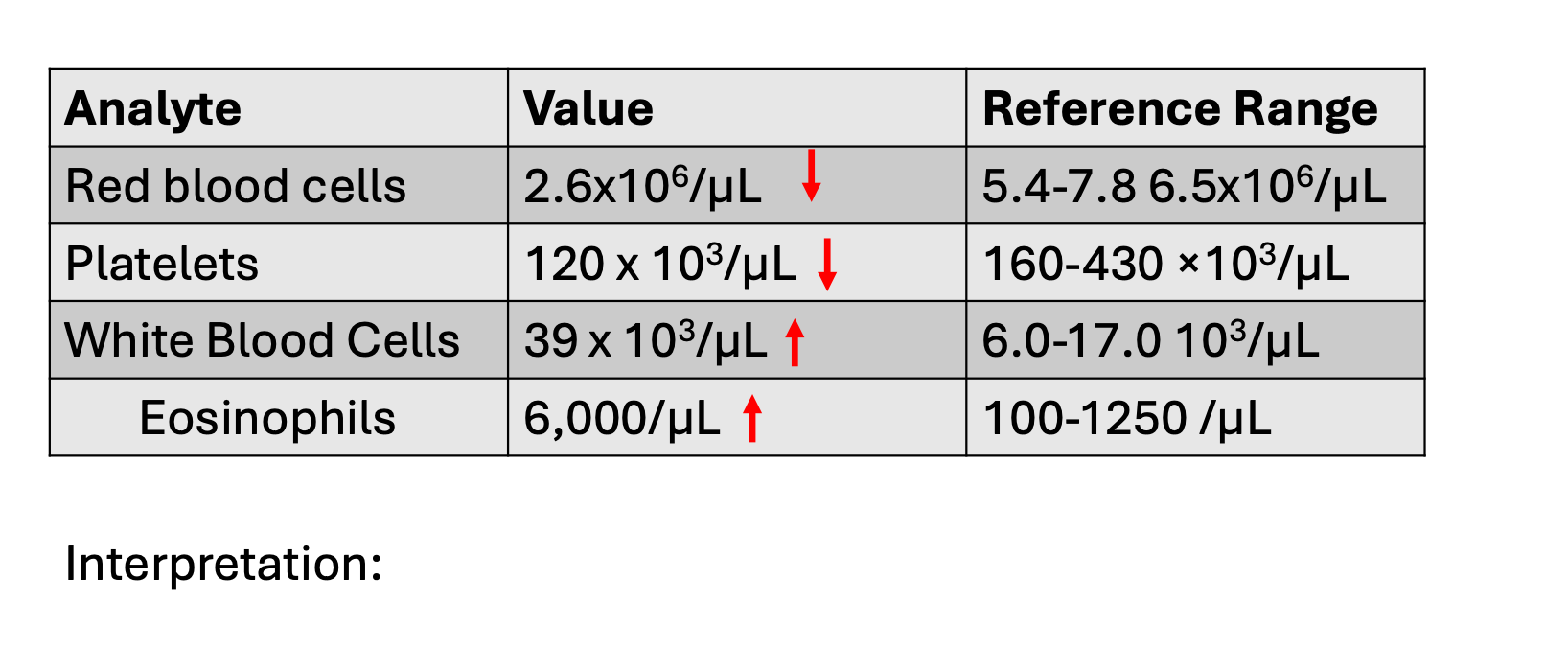
Interpret this CBC
Low red blood cell (anemia)
Low platelets (thrombocytopenia)
High White blood cells (Leukocytosis-eosinophilia)
What are characteristics of Babesia canis?
Protozoa spread by brown dog tick
infects and completes life cycle in RBC
Can cause hemolytic anemia
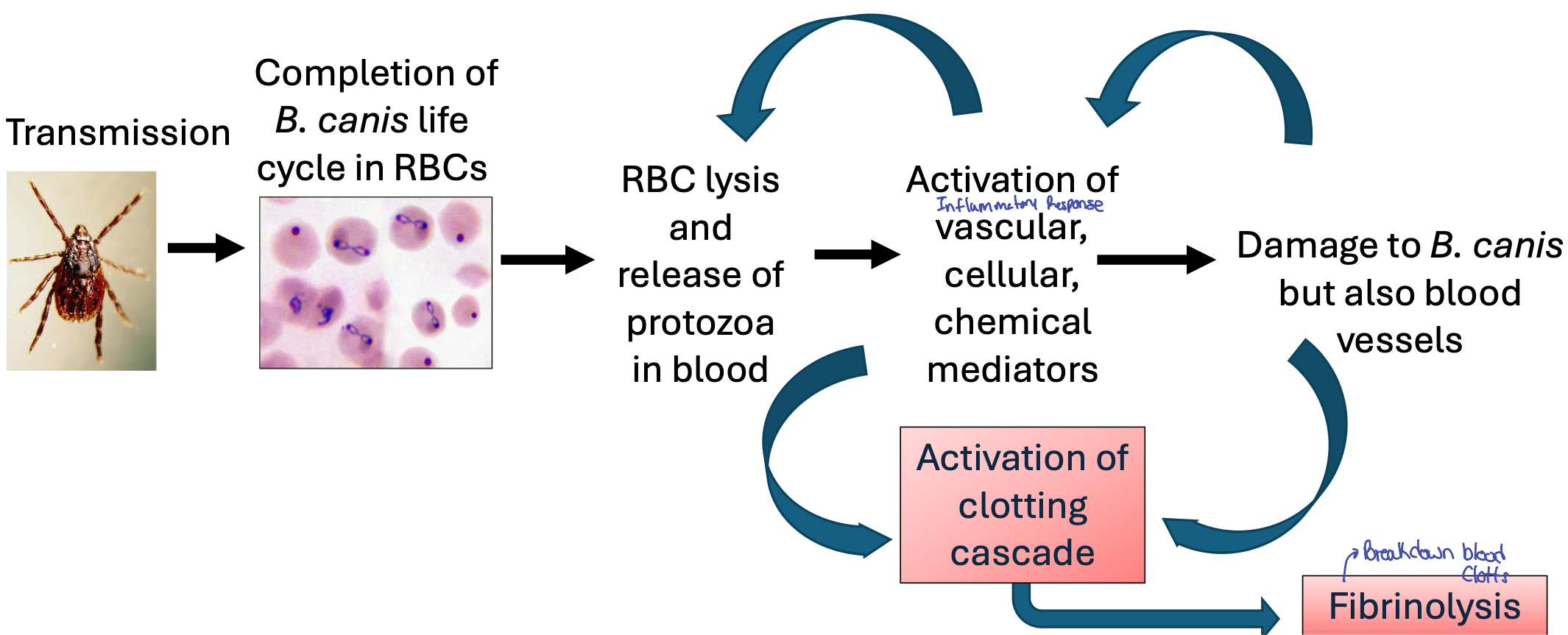
What does this pathway explain?
How an infection can cause a clotting disorder
What is disseminated intravascular coagulation?
Causes widespread consumption of clotting factors, only so many factors in storage.
Cause massive bleeding that cannot be stopped without major intervention