week 2- stomach, duodenum, cancer
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
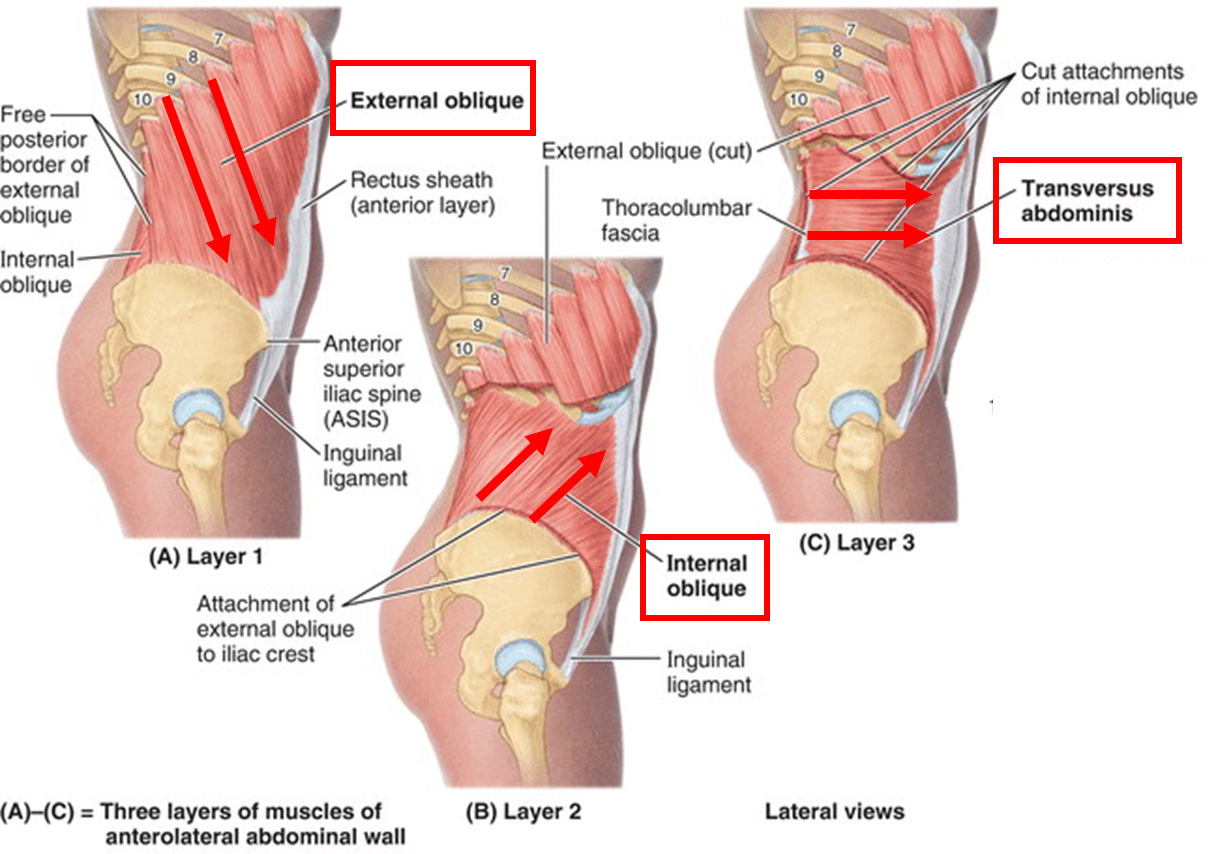
describe the anterolateral boundary of the abdominal wall
Anterior and lateral walls are musculofascial.
•Above umbilicus: Subcutaneous tissue is single sheet of connective tissue
•Below umbilicus: Two layers of connective tissue; Camper’s fascia (fatty layer) & Scarpa’s fascia (membranous deep layer)
Five muscles in the anterolateral group of muscles
outline the anterior muscles of the abdominal wall
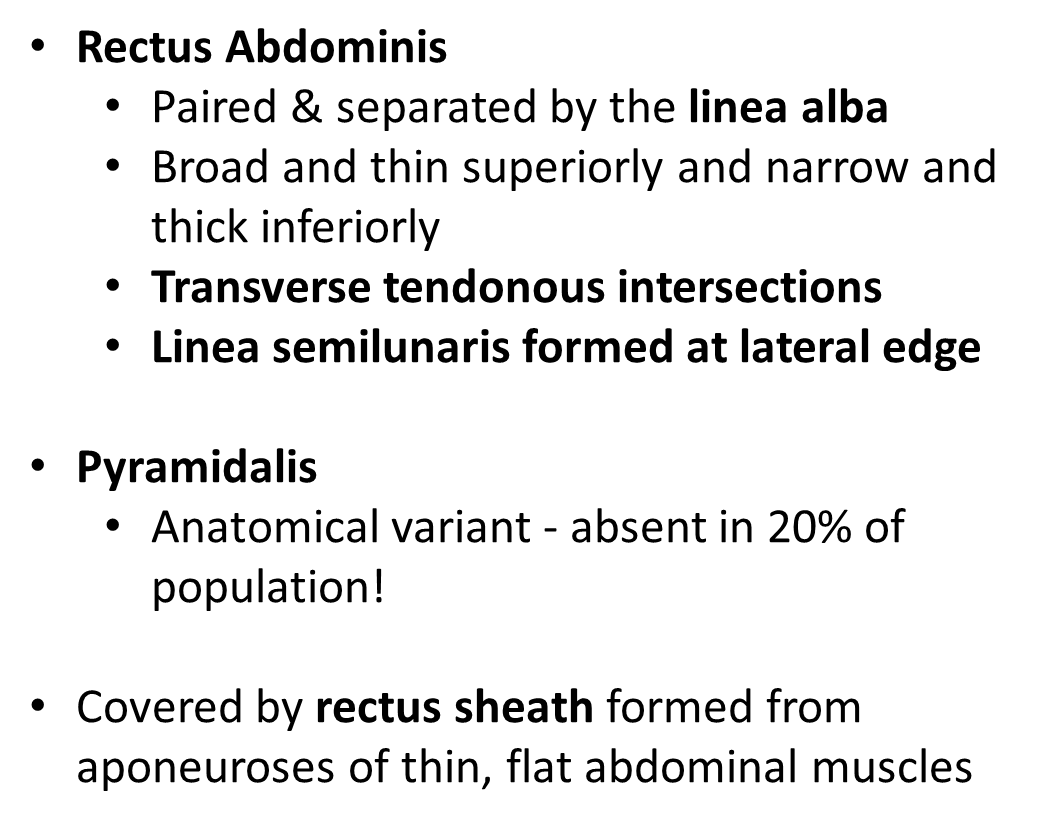
outline the lateral muscles of the abdominal wall
•External Oblique:
•Superficial
•Inferomedial direction
•Creates inguinal ligament
•Free edge posteriorly
•Internal Oblique:
•Intermediate
• Superomedial direction
•Transverse Abdominis
•Deep
•Transverse (horizontal) direction
•All aponeurotic anteriorly
•Form midline raphe - Linea alba
what structure is used to draw the inferior horizontal line in 9 regions?
the iliac tubercle
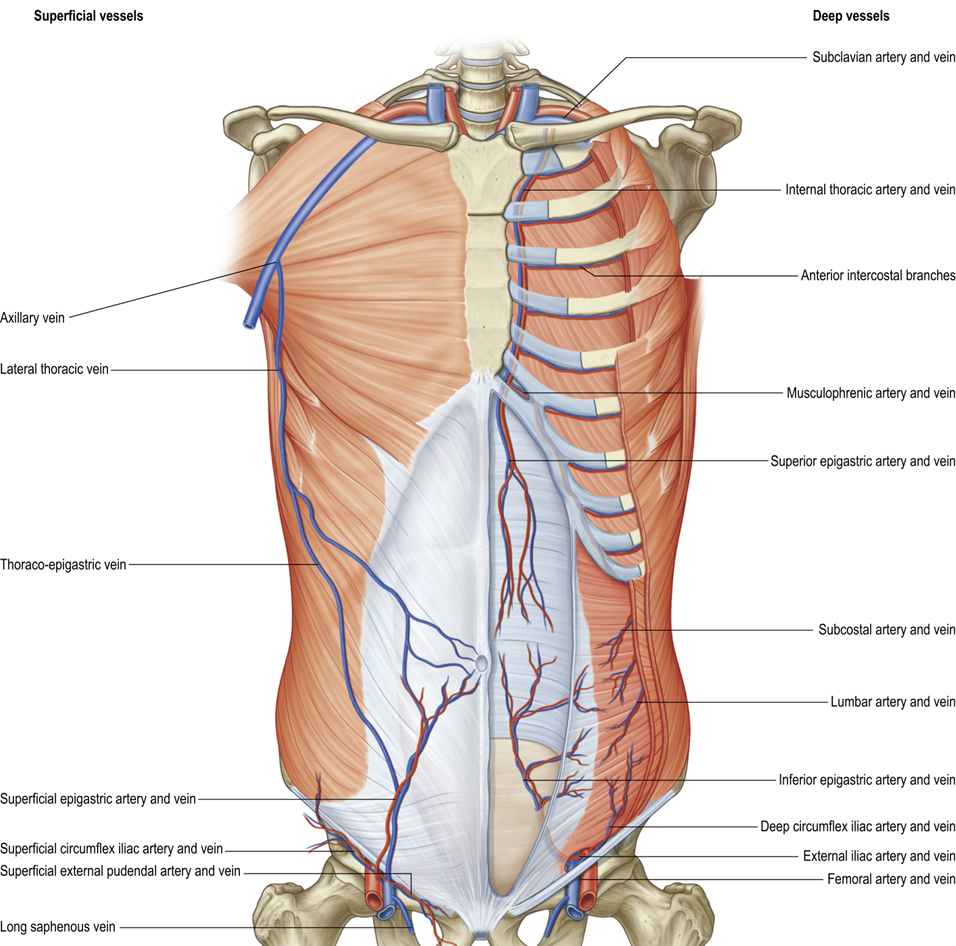
describe the vasculature of the anterolateral abdominal wall
Main vessels:
•Descending
Superior epigastric and musculophrenic arteries
(from internal thoracic)
•Ascending
Superficial epigastric and superficial deep circumflex iliac arteries (from femoral)
•Inferior epigastric and deep circumflex iliac arteries (from ext. iliac)
Laterally
•Intercostal and subcostal arteries
(from thoracic aorta)
•Lumbar arteries (from abdominal aorta)
outline the innervation of the anterolateral abdominal wall
Anterior rami of:
•T7 to T11 (intercostal nerves)
•T12 (subcostal nerve)
•L1 (iliohypogastric nerve and ilio–inguinal nerve)
what is found in the posterior abdominal wall?
•Lumbar vertebrae, pelvic girdle, ribs XI & XII
•Posterior abdominal muscles and fascia
what are the posterior muscles of the abdominal wall?
Quadratus Lumborium
•Thick muscular sheet
Psoas Major
(Psoas Minor) - Anatomical variation – not always present!
Iliacus (lines the iliac fossa)
•Combines with psoas major muscle - known as iliopsoas
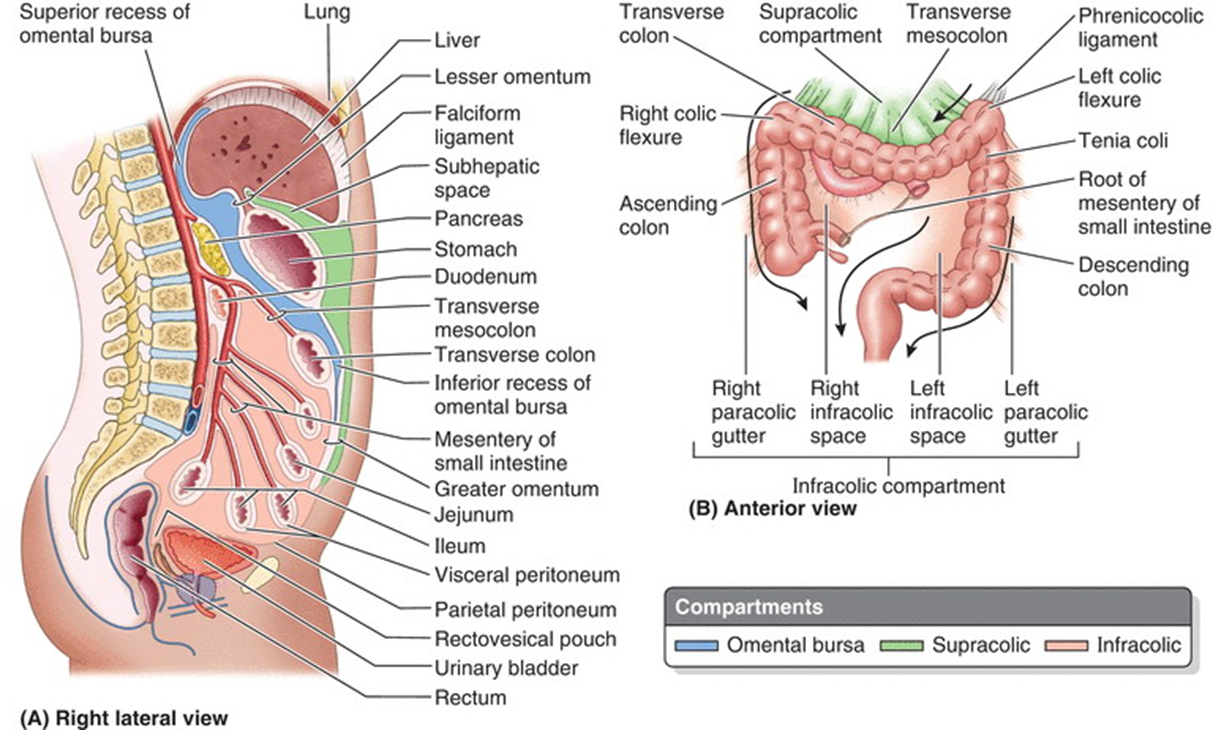
outline the peritoneum and its 3 parts
Continuous serous membrane that lines abdominopelvic cavity
•Parietal peritoneum - Lines abdominal walls
•Visceral peritoneum - Covers viscera
•Peritoneal cavity - Potential space, Peritoneal fluid
what are 2 things viscera can be in the peritoneum, and where does it come from embryologically?
Intraperitoneal:
•Suspended within the cavity, forms from the gut tube
•Eg stomach & spleen
Retroperitoneal:
•Outside cavity posteriorly, only anterior surface covered with parietal peritoneum, form from intermediate mesoderm
•Eg kidneys
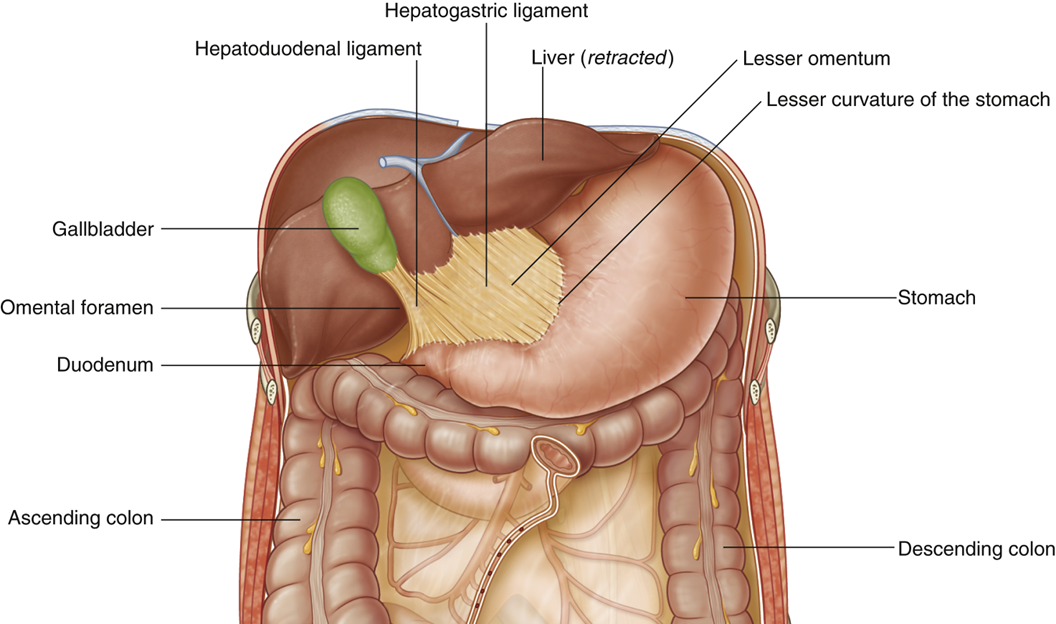
describe the peritoneal folds - greater and lesser Omenta
Omenta are peritoneal folds connecting abdominal organs
Greater omentum:
•Apron-like peritoneal fold that drapes over the intestines
•From greater curvature of stomach & duodenum to the transverse colon
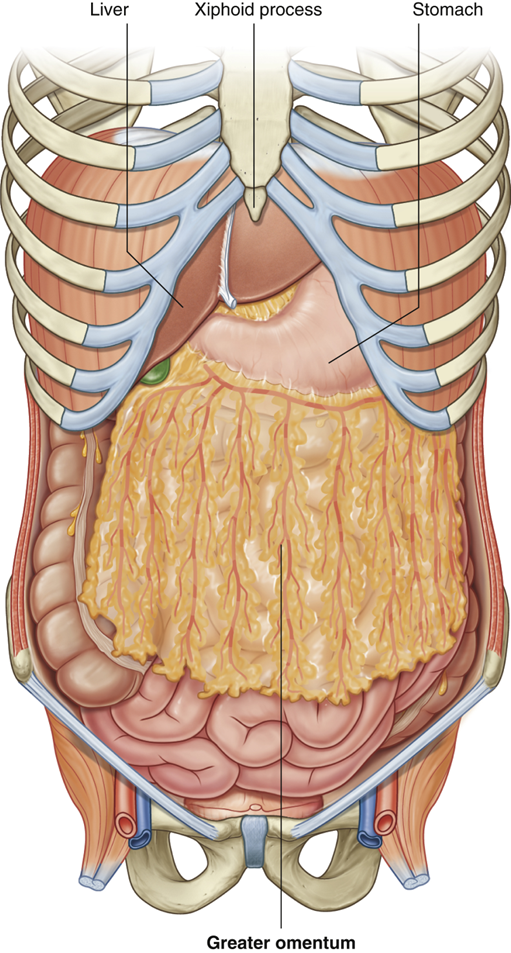
Lesser omentum:
•Peritoneal fold from lesser curvature of stomach & duodenum to inferior surface of liver
•Peritoneal ligaments: Hepatogastric ligament & Hepatoduodenal ligament
•Posterior to the free edge of the lesser omentum is the omental foramen; an opening between the greater and lesser sacs
what is the peritoneal fold - mesenteries?
•Double layers of peritoneum that attaches viscera to the posterior abdominal wall
•It allows neurovascular structures to reach the viscera from the body wall
•Location determines name of mesentery
explain the Mesentery in development
In development, there is a ventral mesentery and a dorsal mesentery
•Ventral mesentery attached to proximal parts of the gut and dorsal mesentery attaches the entire length of the system
•Growth of the liver separates the ventral into the falciform ligament and the lesser omentum
Derivatives of the dorsal mesentery are:
•Mesogastrum-greater omentum in adults
•Mesoduodenum- disappears in adults
•Mesentery proper
•Mesocolon
explain the colic compartments
•The transverse mesocolon divides abdomen into supracolic and infracolic compartments
•Communication between them via the paracolic gutters
•Supracolic:
•Contains liver, spleen, stomach
•Infracolic compartments
•Contains small intestine, ascending and descending colon
•Divided left and right by mesentery of small intestine
explain the innervation of the peritoneum and its localisation of pain
•The innervation of the visceral and parietal peritoneum differs:
Parietal:
•Same spinal nerve that supplies the region of the abdominal wall that it lines
•Pain is well-localised
•Visceral:
•General visceral afferents of the autonomic nervous system
•Activation causes referred and poorly localised pain
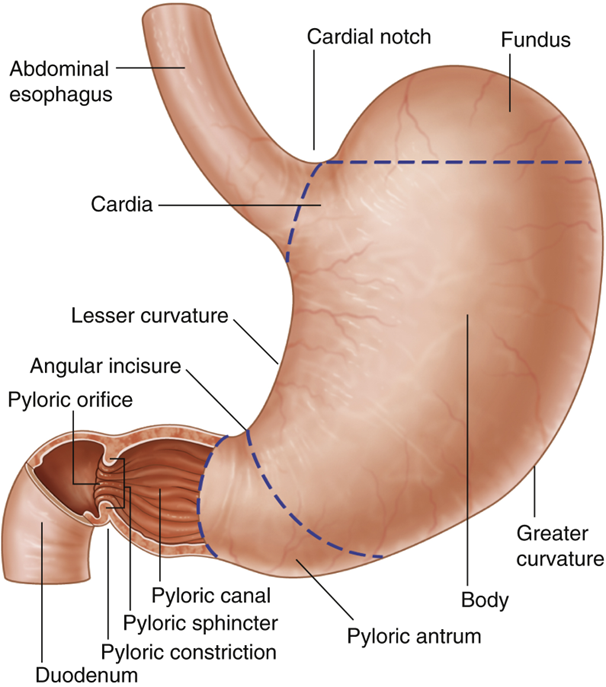
where does the peritoneal folds attach on the stomach?
attach to the stomach via its greater and lesser curvatures. The lesser omentum (or hepatogastric ligament) attaches to the stomach's lesser curvature and extends to the liver. The greater omentum (or gastrocolic ligament) hangs from the greater curvature and attaches to the transverse colon
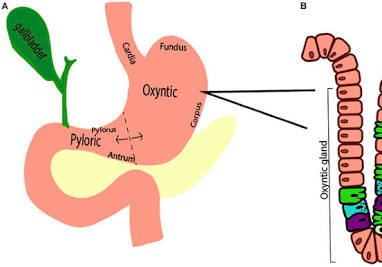
name the regions, sphincters and curvatures of the stomach
Regions of the stomach:
•Cardia
•Fundus
•Body
•Pyloric Part
Sphincters:
•Cardia
Pyloric
Curvatures of the stomach:
•Greater curvature
Lesser curvature
explain the blood supply of the stomach
•The left and right gastric arteries (lesser curvature)
•Left from celiac trunk
•Right from hepatic artery proper
•The left and right gastro-omental arteries (greater curvature)
•Left from splenic artery
•Right from gastroduodenal artery
•Fundus supplied by short gastric arteries
•Branching from splenic artery
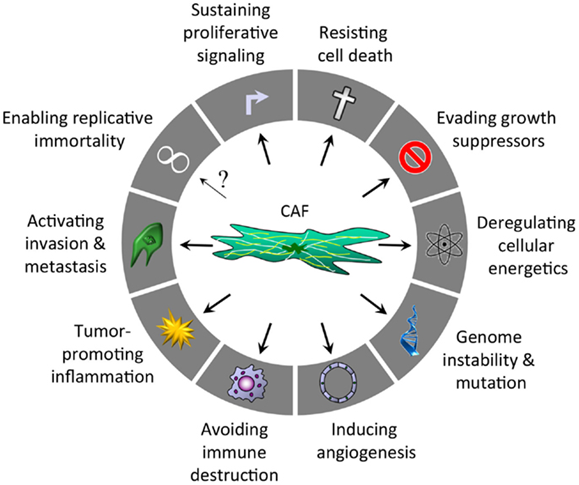
how do cancer-associated fibroblasts promote progression of cancer?
by regulating many hallmarks of cancer by secreting multiple cytokines and growth factors:
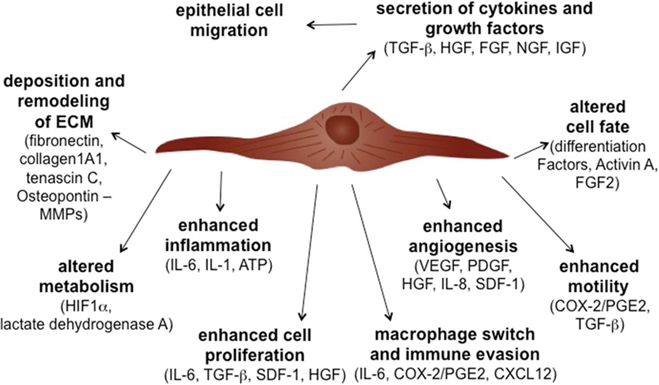
how do cancer-associated fibroblasts interact with tumour cells?
CAFs directly interact with tumour cells to pull them towards the vasculature and aid metastasis
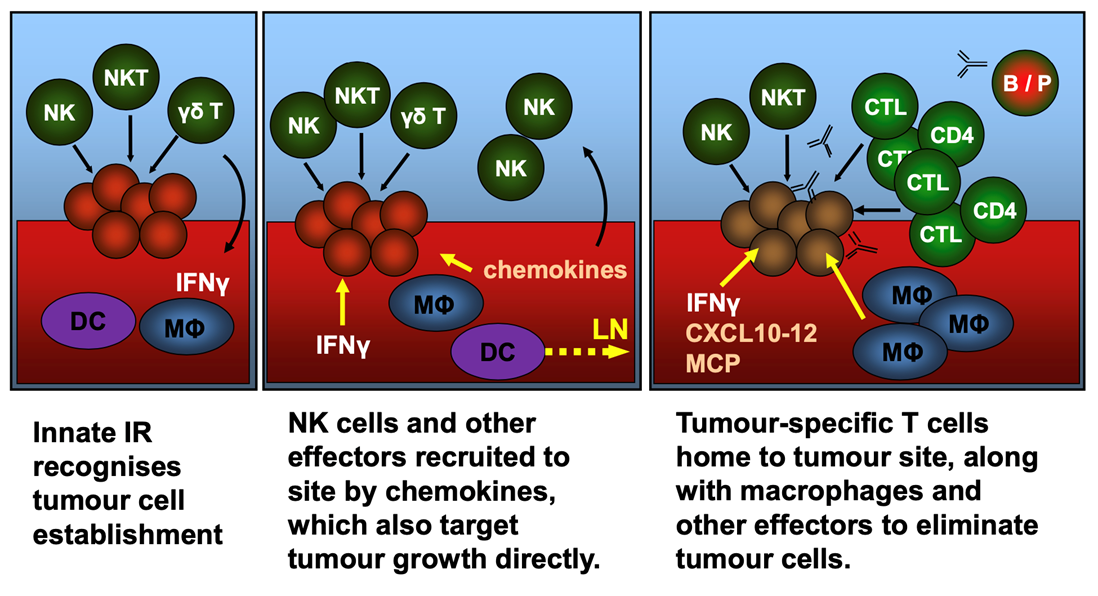
what cells are part of the immune infiltrate in the innate immune response and in the adaptive response?
INNATE: NK cells, dendritic cells, neutrophils, macrophages
ADAPTIVE: CD3+ T-lymphocytes
what are the initial stages of immune infiltrate response?
what are the 2 things immune cells can be?
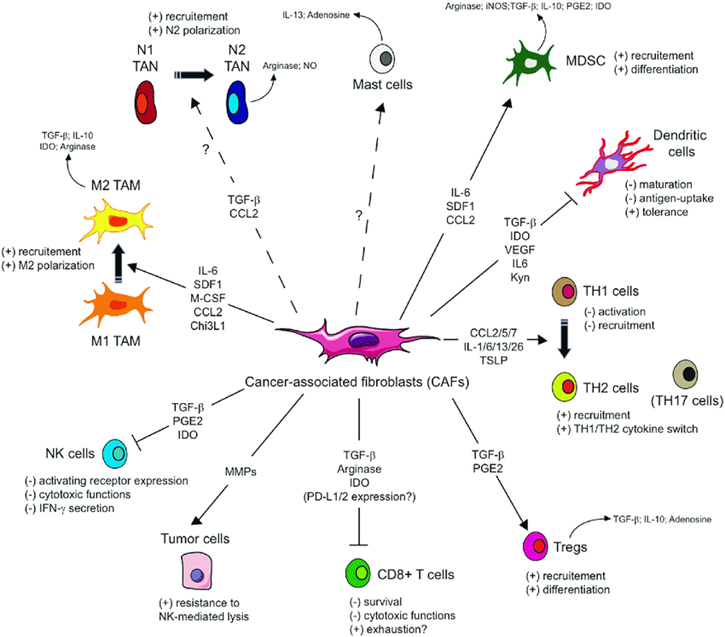
Immune cells can be both anti-tumorigenic and pro-tumorigenic depending on the factors secreted by the tumour cells
what is the role of immune cells regulated by?
by cancer-associated fibroblasts (CAFs)
what has been introduced in the last years to combat cancer?
Immunotherapy, it aims to enhance the patients own immune system to attack the tumour cells. Expensive. used for children with Leukaemia, not much else.
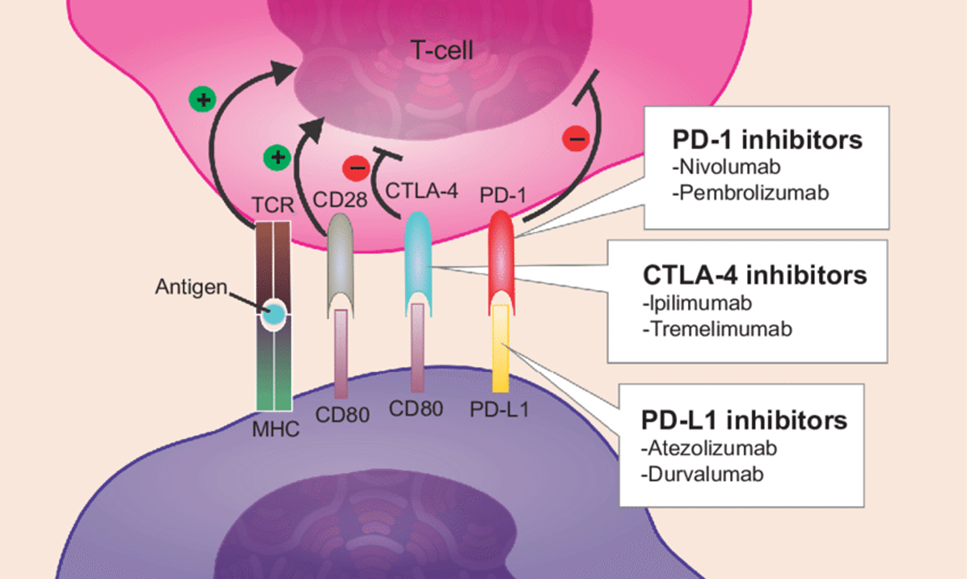
which type of immunotherapy commonly prescribed to cancer patients is the most successful to date, and what do they target?
checkpoint inhibitors such as ipilimumab and nivolumab
•These drugs target immune checkpoint proteins CTLA4 and PD-1/PD-L1
what is the main driver of vascular recruitment (angiogenesis) in the tumour microenvironment?
Hypoxia with some help from CAFs
what does tumour vasculature influence?
the tumour microenvironment and immune infiltrate
how does having an inflammatory disease increase cancer risk?
alternating relapses of inflammation and periods of remission. damage and healing continuously. The release of proinflammatory mediators during IBD relapses leads to cancer development by promoting oxidative stress that favours DNA mutagenesis, antiapoptotic pathways and migration, angiogenesis and invasion
what sequence does tumorigenesis in patients with IBD follow?
the inflammation–dysplasia carcinoma sequence (B) instead of Vogelstein Model (A) described for sporadic CRC (colonrectal cancer). Most sporadic CRC develops from the benign precursor then to an early adenoma, and eventually progresses to invasive carcinoma
Colitis-associated CRC (CAC) develops in a chronically inflamed mucosa and follows the sequence of indefinite dysplasia to low-grade dysplasia to high-grade dysplasia to carcinoma
what is the role of liver in the systemic inflammatory response?
The liver, in particular hepatocytes are central to the elaboration of the systemic inflammatory response as they synthesize and release into the circulation a variety of acute phase proteins, such as C-reactive protein (CRP), which sustain the systemic inflammatory response
what measurements are seen to measure the systemic inflammatory response?
In patients with cancer as CRP [c-reactive protein] (and systemic inflammation) increases, albumin falls (nutritional marker) and this relationship is similar across many different tumour types including multiple GI cancers (gastroesophageal, colorectal, liver)
what does each score in the CRP (c- reactive protein) results mean?
Biochemical Measures | Score | Meaning |
CRP <10mg/ml and Albumin >35mg/ml | 0 | Normal |
CRP >10mg/ml and Albumin >35mg/ml | 1 | Systemically inflamed |
CRP >10mg/ml and Albumin <35 mg/ml | 2 | Systemically inflamed with nutritional deficit |
what can widely influence a cancer patient’s prognosis and survival in GI cancers?
The make up of the TME (tumour microenvironment) and amount and impact of systemic inflammation
what type of prognostic factor is vasculature?
•Increased vasculature is a poor prognostic factor as it promotes tumour progression and metastasis
what type of prognostic factor is increasing numbers of CAFs (Cancer-associated Fibroblasts)?
•In many cancers, increasing numbers of CAFs is a poor prognostic factor as measured by the tumour to stroma percentage
what type of prognostic factor is high levels of T-cells, what about macrophages and neutrophils specifically?
High levels of T-cells are a good prognostic factor.
However, the prognostic value of macrophages is dependent on their subtype and location within the microenvironment. Similarly, the prognostic value of neutrophils is dependent on their location within the microenvironment
what is Modified Glasgow Prognostic Score (mGPS)?
•mGPS predicts prognosis and survival in a variety of GI cancers
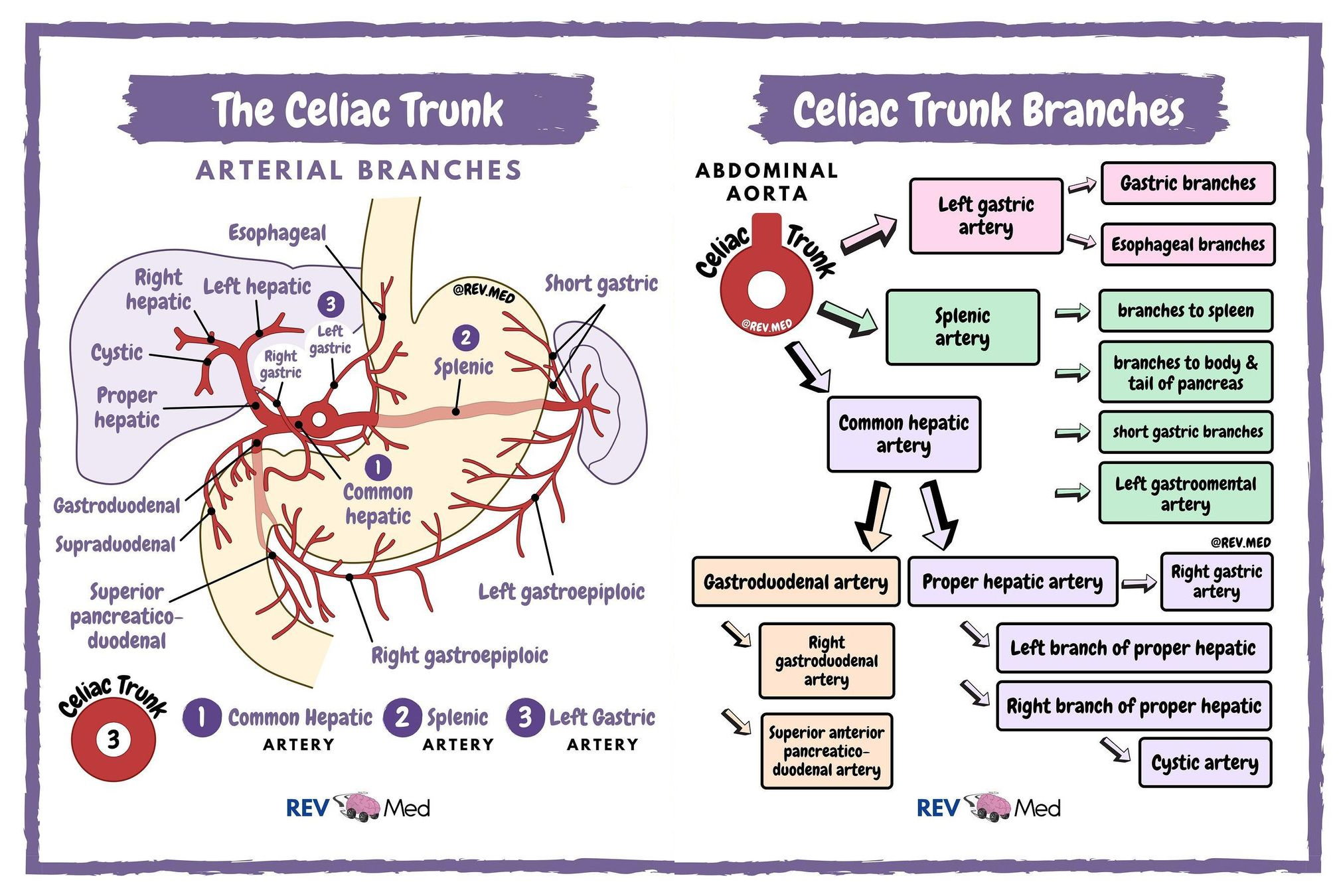
describe the arterial blood supply from the celiac trunk
•Celiac trunk is a large branch from anterior surface of the aorta, immediately below the aortic hiatus of the diaphragm
•It immediately divides into the left gastric, splenic, and common hepatic arteries
•It supplies foregut structures, which includes stomach, spleen, liver, gallbladder and part of duodenum
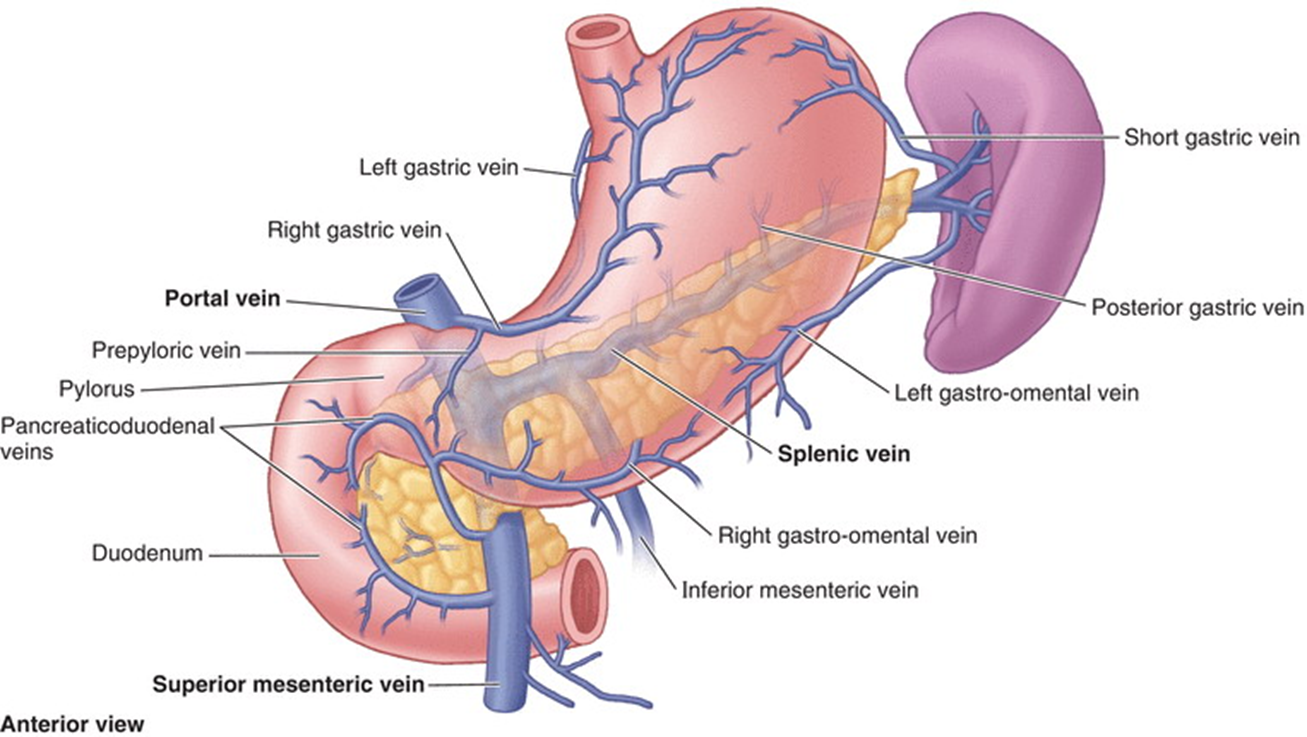
describe the venous drainage of the stomach
•The left and right gastric veins
•The left and right gastro-omental veins
•Short gastric veins
•A prepyloric vein ascends over pylorus and is used to identify this region of the stomach in a living patient
what causes upper GI inflammation?
Imbalance in mucosal protection
environmental ( smoking, chemicals, drugs, viruses, bacteria)
Hormonal secretion
Genetic
Host Immunity
outline what happens in upper GI inflammation on the cellular level
•Cell damage and turn over
•Inflammation and irritation
list symptoms of upper GI inflammation manifestation
abdominal pain
weight loss
diarrhoea
dysphagia
fatigue
vomiting blood
anaemia
vomiting
nausea
funny taste
ulceration
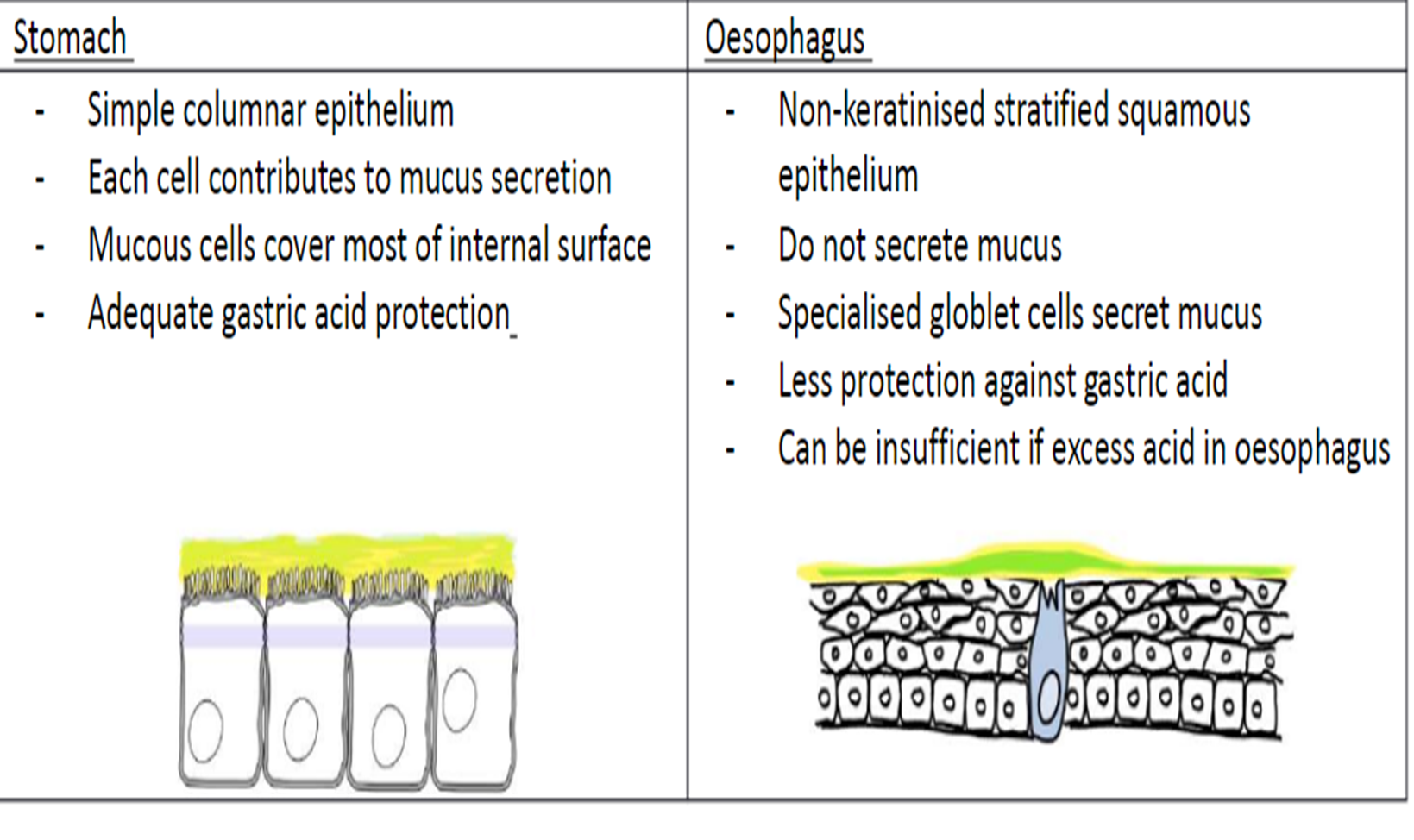
describe and differentiate the epithelium of the stomach and of the oesophagus
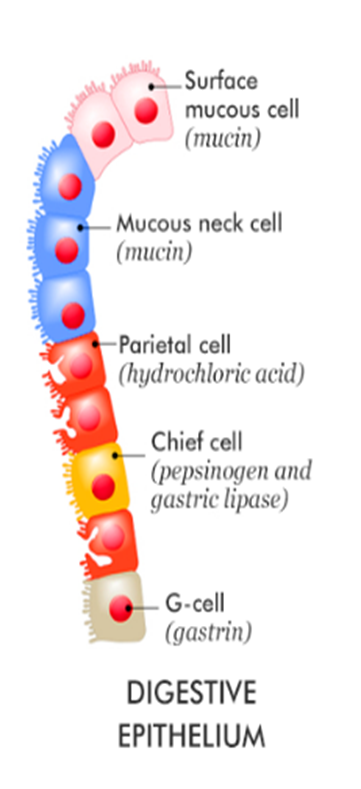
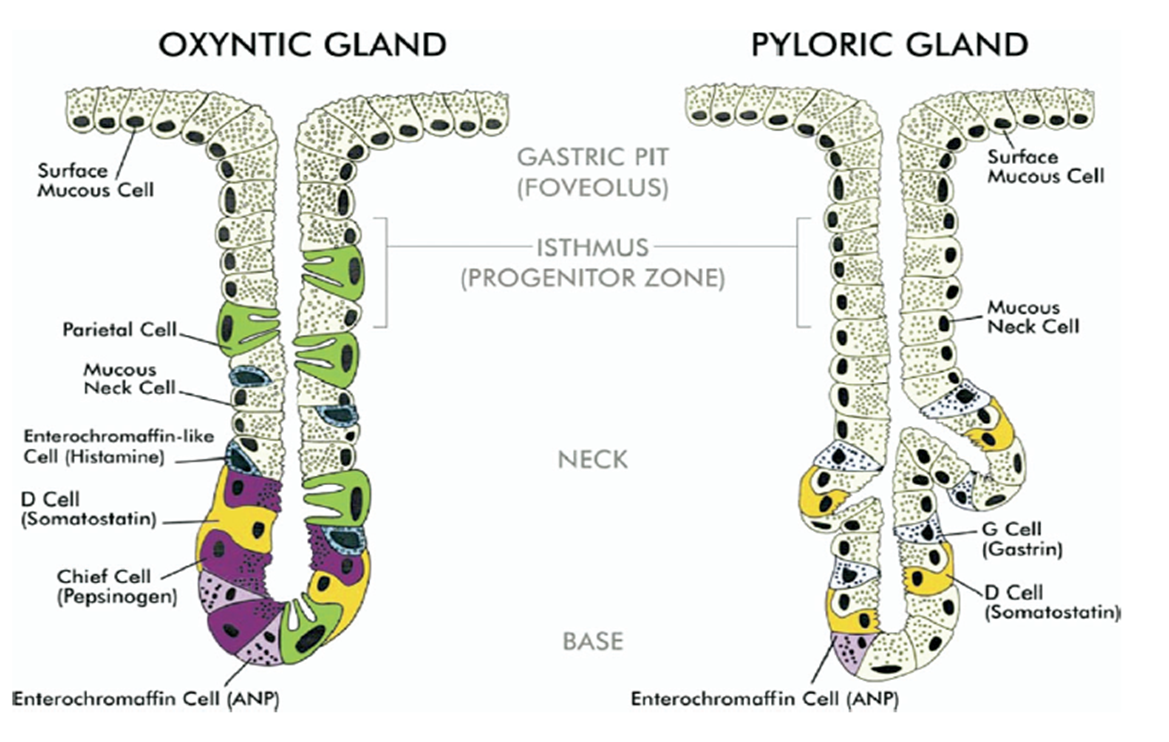
name the secretory glands of the stomach and their secretory products
Cells of Gastric Glands | Secretory products |
Surface Mucus cells | Mucin in an alkaline fluid |
Mucus neck cells | Mucin in an acidic fluid |
Parietal cells | HCL and Intrinsic factor |
Chief cells | Pepsinogen and lipase |
G Cells (enteroendocrine) | Gastrin |
D Cells (pyloric region) | Somatostatin |
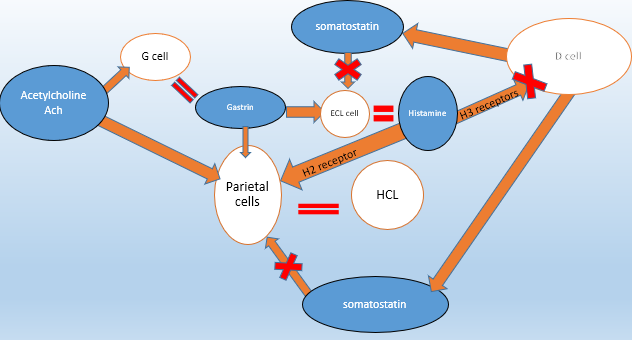
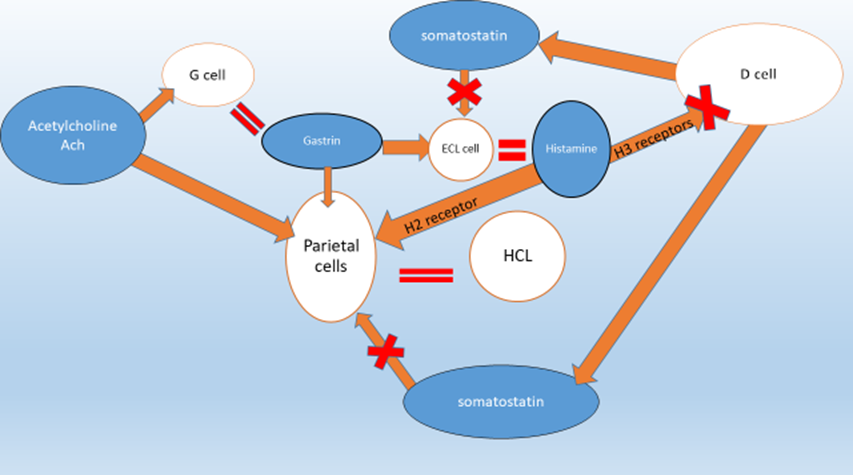
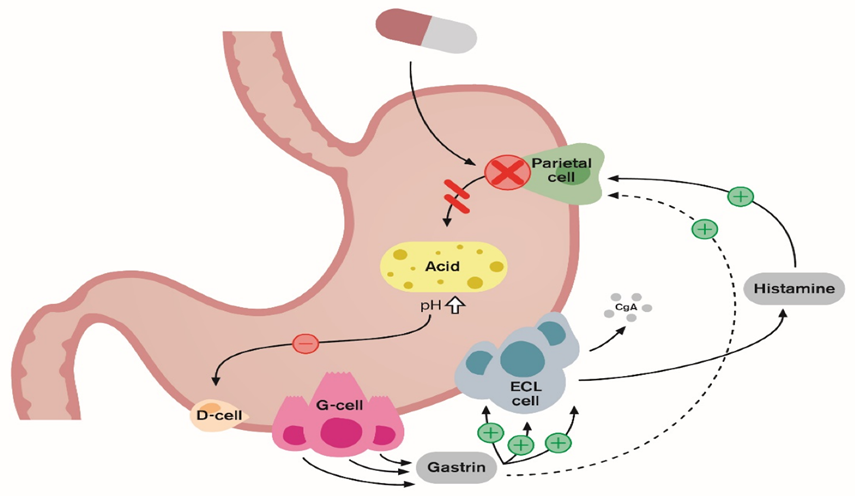
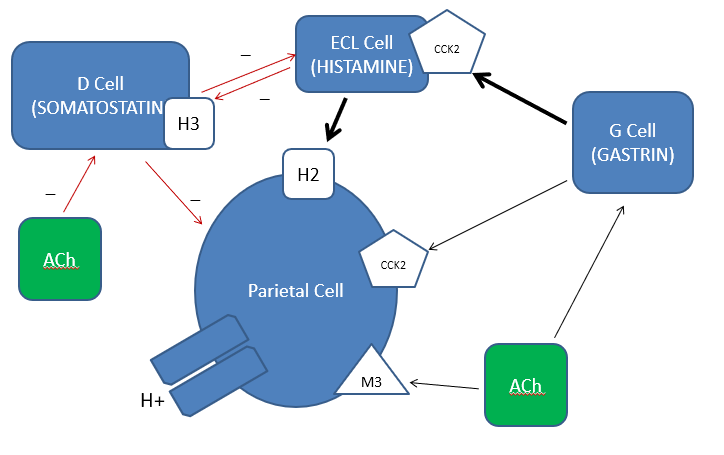
explain the stimulatory pathway
•Gastrin stimulates Enterochromaffin like cell (ECL) to produce histamine
•Gastrin stimulates parietal cell to produce acid
• Ach stimulates G cell to produce Gastrin
• Ach stimulates parietal cell to produce acid
• Somatostatin inhibits ECL cell histamine secretion
• Histamine stimulates acid secretion by acting on parietal cells via H2 receptor
• Histamine stimulates acid secretion by acting on D cell via H3 receptor to inhibit somatostatin production
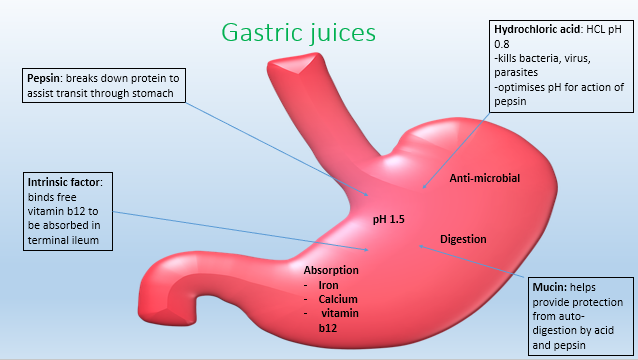
name and explain the roles of the different gastric juices
list some common upper GI inflammatory conditions
GORD: Gastro-oesophageal reflux disease
Gastritis
Ulcers-Oesophageal, Gastric and duodenal
Eosinophilic Oesophagitis
explain GORD: Gastro-oesophageal reflux disease, and the causing factors
Reflux of acidic acid contents
Incompetent lower oesophageal sphincter
The cells: non-keratinised Squamous epithelial cells
DO NOT secrete mucus
Less protection against acid
C/o
Burning, radiation behind sternum
Bending, lying, jumping
Waterbrash; regurgitation acid contents to back of throat
Spicy food, carbonated drinks, alcohol, smoking
Obesity, pregnancy, structural abnormality– increased pressure
Dysphagia ( acid related strictures)
explain Eosinophilic Oesophagitis and its risk factors
- Chronic, allergic inflammatory
-Eosinophils
-Inflammation
- Narrowing
- Food bolus obstruction
Risk factors
-Asthma, allergy, environment-dust, dander, pollen
explain Gastritis and duodenitis and the causing factors
•Inflammation lining of stomach or duodenum
“Dyspepsia”
Imbalance in mucosal protection factors
-Stress, alcohol, drugs, H.pylori, bile
describe the basic of drug treatments
Antacids
•Calcium carbonate
“neutralise”
Raise gastric pH
Reduce pepsin activity
• Alignate/antacid
-Raft barrier
-Raise gastric pH
•H2 antagonists
The “tidines”
Cimitidine
Famotidine
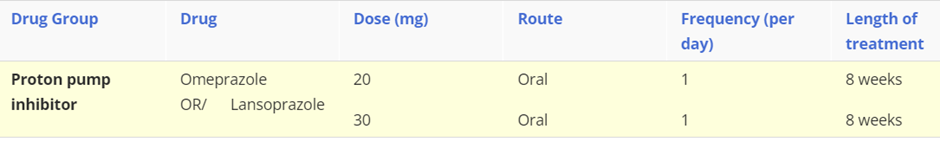
• Proton pump inhibitors
-The Prazoles : Omeprazole, Lansoprazole
•Proton pump (H+/K+-ATPase) is the FINAL step in the secretion of acid in the gastric lumen from parietal cells.
-Bind irreversibly to the proton pump (H+/K+ antiporter) in parietal cell to INHIBIT acid secretion
By BLOCKING the secretion of H+ ions from the cell into the lumen
Most effective suppressors of acid secretion
outline the cause of cancer in the upper GI
Hormones and bacteria are involved in the digestive process
Imbalance in mucosal protection
environmental ( smoking, chemicals, drugs, viruses, bacteria)
Hormonal secretion
Genetic
Imbalance in mucosal protection
•Cell damage and turn over
•Inflammation and irritation
=CANCER
explain the metastatic process of cancer
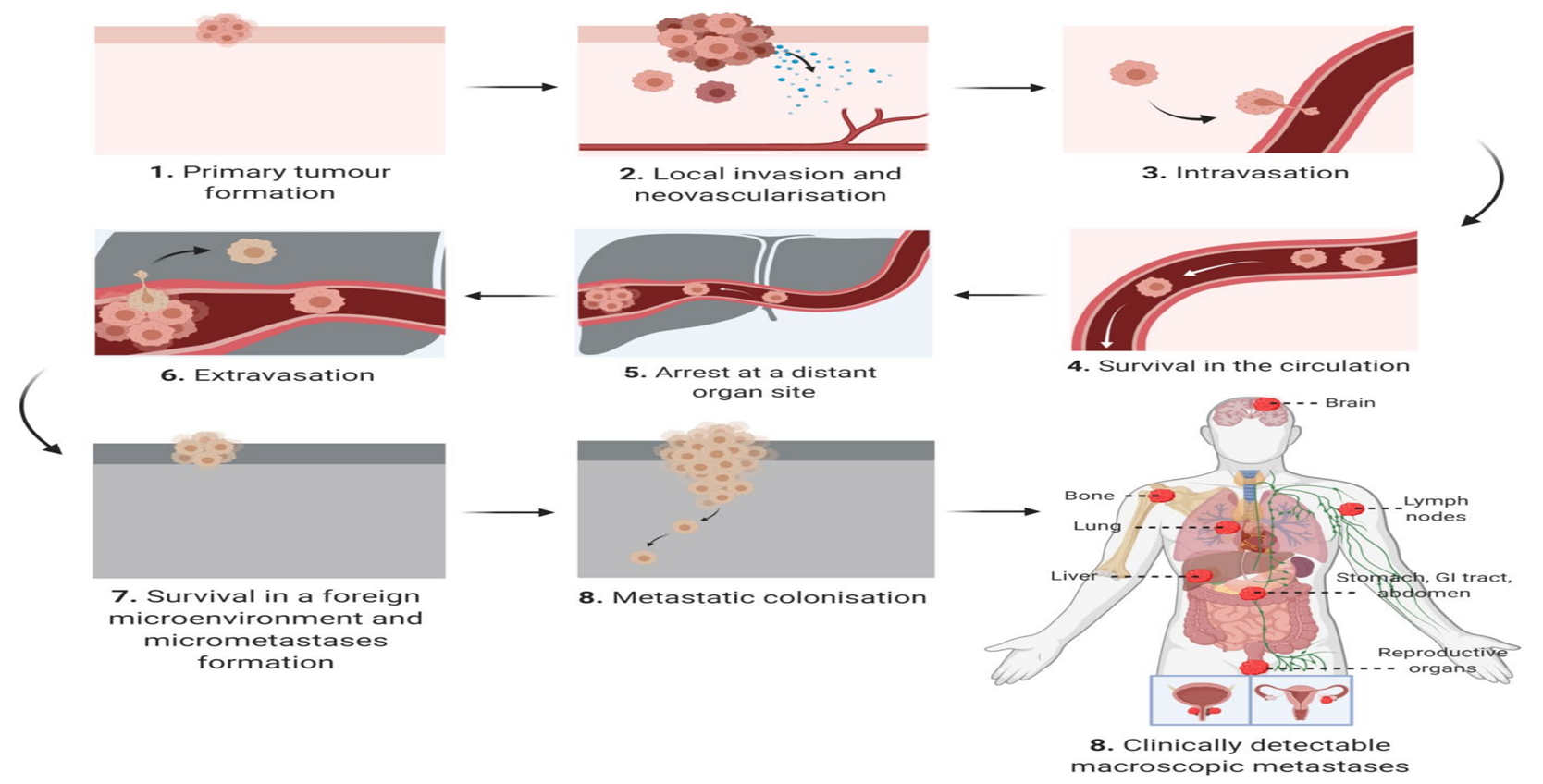
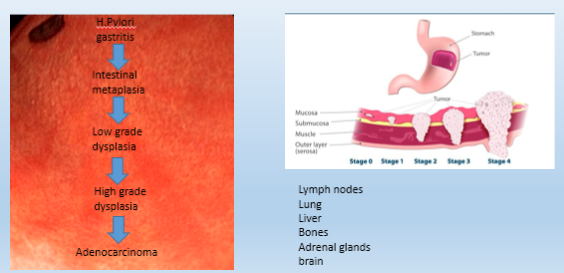
Describe the Gastric and Oesophageal pre-cancerous cascade
Chronic inflammation
- sustained tissue damage
-Damage induced cell proliferation
-Tissue repair
Metaplasia: cell change from one type to another
Dysplasia: cell proliferation leading to atypical cell production
=
Cancer
describe the Oesophageal pre-malignant change in Barret’s Oesophagus and the management pathway
Barret's Oesophagus
Metaplasia
-Abnormal cell change in epithelium
-Stratified squamous to simple columnar
- Goblet cells
management:
Acid damage (management)
Suppress (medication)
Surveillance (regular)
explain the treatment of gastric cancer
H.Pylori
- eradicate
Intestinal metaplasia “transformation”
- Cellular change- small bowel---goblet cells
- Surveillance
Atrophic gastritis
-Chronic inflammation
-loss of gastric gland cells
-replaced by intestinal type epithelium-----fibrous tissue
- Surveillance
outline the oesophageal cancer cascade, grade and metastasis
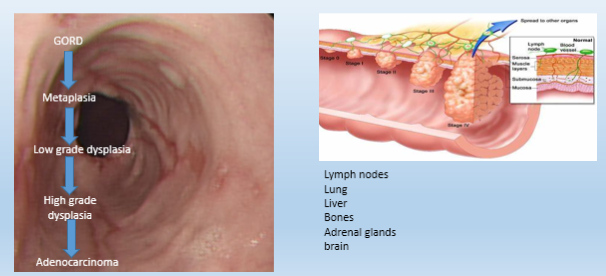
name the 3 gastric cancers and their risk factors
Adenocarcinoma
Signet ring cell
Lymphoma
- H.pylori ( maltoma)
RISK FACTORS:
H.Pylori
Smoking
Being overweight or obese
A diet high in smoked, pickled, or salty foods
Stomach surgery for an ulcer
Epstein-Barr virus infection
Genes
Working in coal, metal, timber, or rubber industries
Exposure to asbestos
what are the components of gastric juice?
•Hydrochloric acid
•Pepsin
•Mucin
•Intrinsic factor
what is the difference between Oxyntic and Pyloric glands?
Oxyntic glands, located in the stomach's fundus and body, secrete hydrochloric acid (HCl) and intrinsic factor from parietal cells, while pyloric glands are in the antrum and secrete the hormone gastrin from G cells to stimulate acid production. The main difference is that oxyntic glands are the primary site of gastric acid secretion, whereas pyloric glands regulate this process by producing gastrin
explain the 3 gastric stimulants and 1 gastric inhibitor of gastric secretion
•Acetylcholine (neuronal – parasympathetic) [acts on muscarinic receptors, on parietal cells]
CEPHALIC PHASE
•Histamine (ECL cell – paracrine) [paracrine messenger in the gastric mucosa, stimulates parietal cells to secrete acid]
•Gastrin (G cell – endocrine) [in the pyloric antrum, stimulates both parietal cells and ECL cells, promoting acid secretion and gastric mucosal proliferation]
IN RESPONSE TO HIGH pH – GASTRIC PHASE
•Somatostatin (D cell – endocrine)
Inhibits gastric acid secretion by acting on somatostatin receptors on parietal cells and inhibiting the release of other stimulatory molecules like gastrin.
IN RESPONSE TO LOW pH – INTESTINAL PHASE
explain the process of gastric secretion
•Gastrin stimulates ECL cell to produce histamine
•Gastrin stimulates parietal cell to produce acid
•ACh stimulates G cell to produce gastrin
•ACh stimulates parietal cell to produce acid
•Somatostatin inhibits parietal cell acid secretion
•Somatostatin inhibits ECL cell histamine secretion
•Histamine stimulates acid secretion by acting on parietal cell via H2 receptor
•Histamine stimulates acid secretion by acting on D cell via H3 receptor to inhibit somatostatin production
Describe Hydrochloric acid concentration and pH, and its functions
Hydrochloric acid : 160 mmol/l pH 0.8
Digestion (converts pepsinogen to pepsin)
Absorption of iron, Vitamin B12, calcium
Antimicrobial
outline the gastric cascade, stage and metastasis
what is Melena?
rapid transit of partly digested blood
why do peptic ulcers occur?
when the protective mucus lining of the stomach or small intestine is damaged, allowing stomach acid to eat away at the underlying tissue. This imbalance between damaging factors (like stomach acid and digestive enzymes) and protective mechanisms is most often caused by H. pylori bacteria or long-term use of NSAIDs.
what’s the Stomach’s Defence Against Gastric Acid?
prostaglandin rich mucus layer
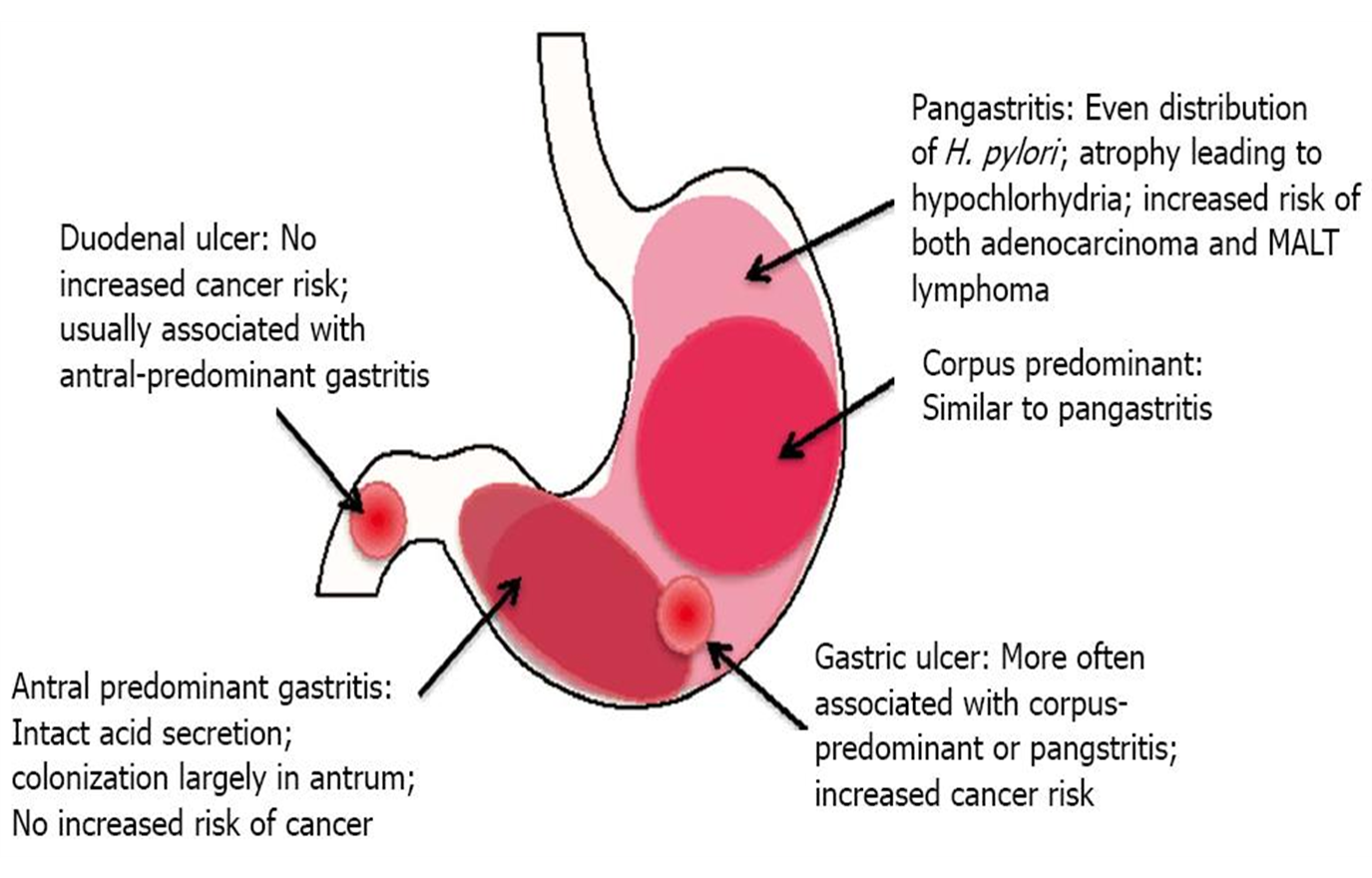
which diseases cause Peptic ulcers?
•Too much attack:
-Zollinger Ellison Syndrome= Gastrin producing tumour
-Helicobacter pylori antral gastritis
•Weakened defence:
- Non steroidal anti-inflammatory drugs
- “Stress” ulceration
- Helicobacter pylori corpus/pan gastritis
what are complications of Peptic ulcer Disease?
air in the diaphragm
anaemia (pale conjuctiva)
what type of bacteria is Helicobacter Pylori?
gram negative bacillus
what is the risk for having an ulcer in different parts of the stomach?
how can H. pylori survive in the stomach’s acidic environment?
H. pylori neutralizes its immediate acidic environment in the stomach by producing the enzyme urease, which converts urea into ammonia and carbon dioxide.
How is Helicobacter pylori detected?
•Blood test : serology for antibody
•Stool test for Helicobacter antigen in faeces
•Tests of urease activity
Urea breath test
Rapid Urease Test from endoscopic biopsy
•Histological biopsy
how do we reduce gastric acid secretion? (to treat H. Pylori)
H2 Receptor antagonists:
•Cimetidine (Tagamet)
•Ranitidine (Zantac)
•Famotidine (Pepcid)
Competitively and reversibly inhibit H2 receptor on parietal cell
Proton Pump Inhibitors:
•Omeprazole (and Esomeprazole)
•Lansoprazole
•Pantoprazole
•Rabeprazole
what are the surgical procedures that are rarely used and performed only in select cases of severe, persistent peptic ulcer disease?
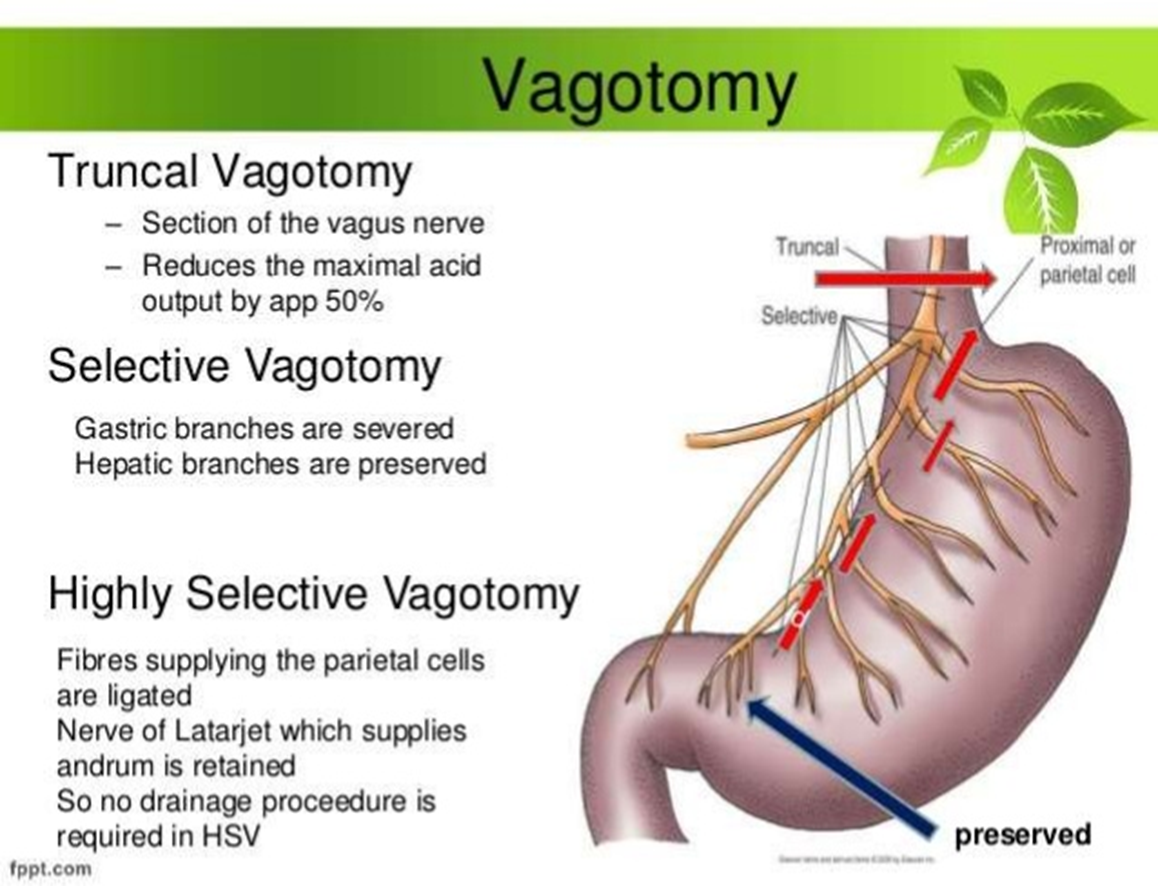
Vagotomy with Antrectomy: surgical procedure involving cutting the vagus nerve (vagotomy) and removing the stomach's antrum (antrectomy)
what is Proton Pump Inhibitors (PPI) mechanism of action?
Oral ingestion
Absorbed via small intestine
Uptake only when ATPase making acid
Short plasma t ½ (30-60 minutes)
MOST effective on an empty stomach
what are potential mechanism of PPI (protein pump inhibitors) adverse effects?
(1) Reduction in Gastric Acid Output
- Reduced nutrient absorption (vitamin B12, iron, calcium)
- Reduced gastric antimicrobial function (Community Acquired Pneumonia, Enteric infections=illness that enters the body through the GI)
(2) Increase in serum gastrin Levels (Neoplasia, Osteoporosis-Risk higher with shorter duration of therapy, Rebound acid hypersecretion-return or worsening of acid-related symptoms after stopping PPIs)
(3) Idiosyncratic (rare, unpredictable reaction in an individual that isn't a typical side effect) (Lymphocytic colitis- too high lymphocytes level in colon, Interstitial Nephritis- kidney inflammation in the spaces between kidney tubules, Hypomagnesaemia- abnormally low levels of magnesium in the blood)
(4) Interaction with metabolism of other drugs
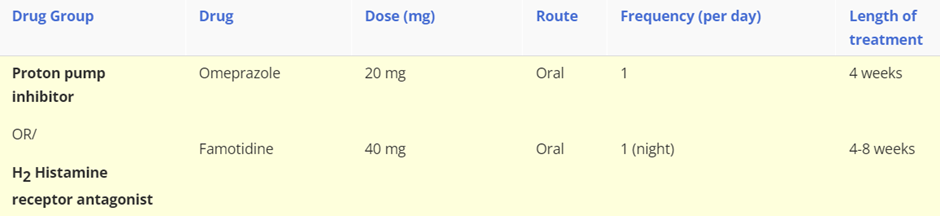
describe peptic ulcer disease: including what they are, symptoms, the 2 main causes, treatment for the drug induced cause (drug group, drug name, length of treatment, route)
Peptic ulcer disease
Peptic ulcer disease includes gastric or duodenal ulceration, which is a breach in the epithelium of the gastric or duodenal mucosa.
Symptoms: The main symptom of peptic ulcer disease is upper abdominal pain but other less common symptoms include nausea, indigestion, heartburn, loss of appetite, weight loss and a bloated feeling.
Causes: The most common causes of peptic ulcer disease are Non-steroidal anti-inflammatory (NSAIDs) drug use and Helicobacter pylori (H. pylori) infection. Smoking, alcohol consumption, and stress may also contribute to the development of peptic ulcer disease.
Treatment:
NSAID drug use peptic ulcer disease
Proton pump inhibitor OR histamine H2 antagonists
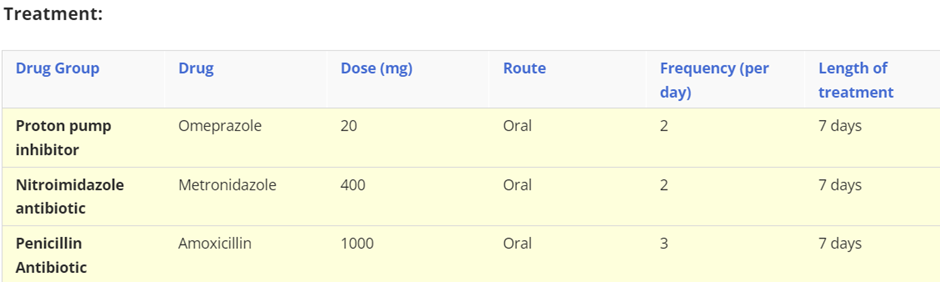
describe Helicobacter pylori infection, including description, associated diseases, symptoms, cause and treatment (drugs groups, drug name, length of treatment, route)
Helicobacter pylori infection
Helicobacter pylori (H. pylori) infection is one of the most common causes of peptic ulcer disease, with 95% of duodenal and 70–80% of gastric ulcers associated with it. The use of NSAIDs may have an additive effect if there is co-existent H. pylori infection, further increasing the risk of peptic ulceration and bleeding. H. pylori is also associated with acute and chronic gastritis, gastric cancer, and gastric mucosa associated lymphoid tissue (MALT) lymphoma.
Symptoms: Severe indigestion that does not respond to over the counter or other medications, as well as nausea, bloating. Rare symptoms include stomach and duodenal ulcers, unintentional weight loss, vomiting blood, melaena (black, sticky poo).
Causes: many people have it, but it does not cause any problems and therefore, do not require any treatment. Coming into contact with the bodily fluids/faeces of a person that has it will however cause effects on the other people.
describe Gastro-oesophageal reflux disease (GORD), the 2 classifications, causes, symptoms and treatment (drug group, drug name, length of treatment, route)
Gastro-oesophageal reflux disease (GORD) is usually a chronic condition where there is reflux of gastric contents (particularly acid, bile, and pepsin) back into the oesophagus. GORD can be classified as:
non-erosive when a person has symptoms of GORD but the endoscopy is normal
erosive oesophagitis when oesophageal inflammation and mucosal erosions are seen at endoscopy.
Symptoms: GORD causes symptoms of heartburn and acid regurgitation. Less common symptoms such as chest pain, hoarseness, cough, wheezing, asthma and dental erosions can also occur if acid reflux reaches the oropharynx and/or respiratory tract.
Causes: Consumption of trigger and fatty foods, pregnancy, hiatus hernia, family history of GORD, increased intra-gastric pressure from straining and coughing, stress, anxiety, obesity, drug side-effects, smoking and alcohol consumption.
Treatment: Proton pump inhibitor or H2 antagonist