Personality Disorders
1/56
Earn XP
Description and Tags
Exam 1 - sem 3
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
What is personality
Ingrained, enduring patterns of behavior
How one behaves toward
Self
Others
Environment
Personality
A unique way of thinking, feeling, and behaving that is influenced by experiences, environment (surroundings/life situations), and inherited characteristics
Personality traits
May be defined as characteristics with which an individual is born or develops early in life. They influence the way in which he or she perceives and relates to the environment and are quite stable over time
Personality disorder
Occur when these traits become rigid and inflexible and contribute to maladaptive patterns of behavior or impairment in functioning
Personality includes
Perceptions
Attitudes
Emotions
Personality disorders definition from DSM-5
An enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment
Developmental theories
Personality development occurs in response to a number of biological and psychological influences. These variables include (but are not limited to) heredity, temperament, experiential learning, and social interaction
Each suggests that personality development occurs in an orderly, stepwise fashion. These stages overlap to account for maturation rates being different individuals
Common characteristics of all personality disorders
Inflexibility/maladaptive response to stress
Failure to accept the consequences of behavior
Compulsiveness and lack of social restraint
Inability to emotionally connect in all relationships
Tendency to provoke interpersonal conflict
Lack of insight, poor boundaries
Involve reliance on maladaptive coping skill
Diagnosing personality disorder
Enduring pattern of inner experience and behavior that deviates markedly from expectations of cultures
Manifested by 2 or more of the following:
Thoughts: ways of looking at the world, thinking about self or others. interacting]
Emotions: appropriateness, intensity, range of emotional functioning
Interpersonal functioning: relationships, interpersonal skills
Impulse Control
Personality disorders: diagnostic clusters
Cluster A: odd-eccentric
Cluster B: dramatic-emotional
Cluster C: anxious-fearful
Cluster A: odd-eccentric
Paranoid Personality Disorder
Schizoid Personality Disorder
Schizotypal Personality Disorder
Paranoid Personality disorder
Suspicious; guarded
Hypervigiliant
Ready for any real or imagined threat
Insensitive to feelings of others
Feels that others are taking advantage of them
Trust no one
Constantly tests the honesty of others
Do not accept responsibility for their own behaviors
Envious and hostile toward others that are successful
Bears grudges
Paranoid Personality disorder facts
Prevalence: estimated at 1-4% of the population
Predisposing Factors:
Genetic/Hereditary: higher incidence among relatives of individuals diagnosed with schizophrenia, psychosis.
May have been subjected to parental antagonism and harrassment
Learned to perceive the world as “harsh and unkind”
Anticipating humiliation and betrayal by others, the paranoid person has learned to “attack first.”
Schizoid Personality disorder
Profound defect in the ability to form personal relationships and are often seen as eccentric, isolated or lonely
Neither desires or enjoys relationships including family
Chooses solitary activities
Lacks close friends or confidants except first degree relatives
Indifferent to praise or criticism
Emotional coldness, detachment, flat affect.
Appears shy, anxious, uneasy in the presence of others.
Takes pleasure in few, if any, activities
Schizoid Personality disorder facts
Prevalence: estimated at 3-5% of the population
Predisposing Factors:
Introversion is believed to be hereditary.
The development of this disorder is likely influenced by early interactional patterns that the person found to be cold and unsatisfying.
Childhoods are characterized as bleak, cold, and notably lacking empathy and nurturing
Schizotypal Personality disorder
Ideas of reference
Odd beliefs, magical thinking, superstitious, clairvoyance, bizarre fantasies
Suspicious and paranoid
Inappropriate affect
Behavior or appearance is odd, eccentric or peculiar
Lack of close friends
Excessive social anxiety even in familiar social settings.
Bizarre speech patterns
Described as “latent schizophrenics”
Behavior is odd and eccentric, but not decompensated to the level of schizophrenia.
Schizotypal Personality disorder facts
Prevalence: estimated at around 4% of the population
Predisposing Factors:
Genetic link suggests that this disorder is more common among first degree relatives with schizophrenia.
Anatomical deficits or neurochemical dysfunctions resulting in diminished activation, minimal pleasure-pain sensibilities, and impaired cognitive functions.
Early family dynamics characterized by indifference, impassivity, or formality, leading to a pattern of discomfort with personal affection and closeness.
Nursing interventions: cluster A personality disorders
Respect personal space
Respect client’s preferences
Give feedback based on non-verbal cues
Provide client with daily schedules and inform client of changes
Help client identify adaptive diversionary activities
Use an objective, matter of fact approach
Use concrete, specific words rather than global abstractions
Cluster B: dramatic-emotional
Antisocial Personality Disorder
Borderline Personality Disorder
Histrionic Personality Disorder
Narcissistic Personality Disorder
Antisocial personality disorder
Socially irresponsible, exploitative, guiltless behavior
General disregard for the rights of others.
Failure to conform to social norms/laws; legal issues, arrests
Deceitful, lying, use of aliases, conning others
Charming, witty
Irritable and aggressive, physical fights
Reckless disregard for others
Irresponsible—failure to sustain work or honor financial obligations
Cannot maintain relationships
Seldom seen in clinical settings, or when they are it is to avoid legal consequences. More likely to be in jail, prison
*will make you like them and then kill you without caring
Antisocial personality disorder facts
Prevalence: 2-4 percent of the general population
Predisposing Factors:
Data from twin studies suggests high genetic vulnerability among first degree relatives
Studies have shown higher prevalence among childhood experiences with parents with alcoholism
Children with frequent temper tantrums that are undaunted by punishment
ADHD, Oppositional Defiant Disorder, and Conduct disorders increase risk of antisocial personality disorder as an adult
NANDA: antisocial personality disorder
Risk for other-directed violence
Defensive coping
Chronic low self-esteem
Impaired social interaction
Ineffective Health Maintenance
Nursing interventions: antisoical personailty disorder
Convey an accepting attitude toward patient
Use a concerned, matter-of-fact approach
Set, communicate and maintain consistent rules and regulations
DO NOT argue, bargain or rationalize
Confront inappropriate behaviors
DO NOT seek approval or coax; use choices and consequences
Be alert for flattery or verbal attacks.
Maintain low stimuli
Explore alternative ways to handle behaviors
Borderline personality disorder
Instability of affect, identity and relationships, frequent mood shifts
Unstable and intense relationships starting in early adulthood
“Splitting” behaviors: “All or nothing”, flatter or favor one staff person over another to get what they want
Manipulation
Impulsiveness: $$, sex, substances, driving, binge disorder
Fear of abandonment
Often uses self injury as a coping mechanism
Often related to dysfunction in childhood (i.e.: abuse)
Borderline personality disorder facts
Prevalence: 1-2 percent of the general population
Predisposing Factors:
Biochemical – serotonergic defect
Genetic- increased risk of development with depression in family background.
Family environments characterized by trauma, neglect, and/or separation, exposure to sexual or physical abuse, and serious parental psychopathology such as substance abuse and/or antisocial personality disorder.
Developmental: struggles with separation and autonomy
NANDA: borderline personality disorder
Risk for self-injury
attention seeking behavior; coping mechanisms
Complicated grieving (separation distress)
Impaired social interaction
struggle with having solid relationships; intense too quickly
Disturbed personal identity
Anxiety
Chronic low self-esteem
Nursing interventions: borderline personality disorder
Observe patient’s behaviors closely
Set limits, maintain consistency
Report in the morning to make sure everyone is on the same page
Convey an accepting attitude and develop trust
Rotate staff working with patient so they do not develop dependence on particular individuals
Histrionic personality disorder
Characterized by colorful, dramatic, and extroverted behavior in excitable and emotional people.
Uncomfortable in situations where he/she is not the center of attention
Interactions characterized by inappropriate sexual seduction
Rapidly shifting and shallow expressions of emotion
Style of speech is impressionistic and lacking in detail
Self dramatization, theatrically exaggerated expression of emotion
Considers relationships to be more intimate than they actually are
Is suggestible (easily influenced by others or circumstances)
Histrionic personality disorder facts
Prevalence: 2-3%of the general population
Predisposing Factors:
Studies suggest correlation with decreased serotonergic activity.
Heredity studies indicate increased prevalence amongst first-degree relatives.
Increased risk of development in those that show “an extreme variation of temperamental disposition.”
Psychosocially, the child may have learned that positive reinforcement was contingent on the ability to perform parentally approved and admired behaviors
Narcissistic personality disorder
Arrogant; grandiose views of self importance
Need for constant admiration
Sense of entitlement
Lack of empathy for others that strains most relationships
Sensitive to criticism
Envious of others and believes that others are envious of him/her
Takes advantage of others for self gain
“All about me”
Narcissistic personality disorder facts
Prevalence: 6% of the general population
Predisposing Factors:
Studies indicate higher prevalence among children who had their fears, failures, or dependency needs responded to with criticism, disdain, or neglect. They grow up with contempt for these behaviors in sources of comfort and support.
Studies also indicate increased prevalence among first degree relatives. Narcissism may also develop from an environment in which parents attempt to live their lives vicariously through their child, expecting their child to achieve what they were not able to
Nursing interventions: Cluster B personality disorders
Acknowledge manipulative behaviors
Maintain realistic, consistent, firm limits with enforceable consequences
Give a rationale for limits and consequences
Maintain consistency among staff members
Confront client each time manipulation occurs:
Example: both staff confront client when manipulative behavior (ie: splitting) occurs
Cluster C: anxious/fearful
Avoidant Personality Disorder
Dependent Personality Disorder
Obsessive-Compulsive Personality Disorder
Avoidant personality disorder
Avoids social activities r/t fear of criticism, disapproval or rejection
Unwilling to get involved with people unless they are sure to be liked
Shows restraint in intimate relationships due to fear of ridicule
Preoccupied with being criticized or rejected in social situations
Views self as inept, unappealing or inferior
Anxious in social situations
Avoidant personality disorder facts
Prevalence: 2% of the general population
Predisposing Factors:
No clear cause noted but psychosocial studies have shown increased prevalence with parental rejection and censure, which is often reinforced by peers. These children are often reared in families in which they are belittled, abandoned, and criticized such that any natural optimism is extinguished and replaced with feelings of low self-worth and social alienation
Dependent personality disorder
Extreme dependency in a close relationship with an urgent search to find a replacement when one relationship ends.
Difficulty making every-day decisions or taking care of self
Need excessive amounts of advice and reassurance from others
Difficulty initiating projects d/t lack of self confidence
Goes to excessive lengths to obtain reassurance from others
Unrealistically preoccupied with fears of being left alone
Dependent personality disorder facts
Prevalence: 2-4% of the general population
Predisposing Factors:
Psychosocially, dependency is fostered in infancy when stimulation and nurturance are experienced exclusively from one source. The infant becomes attached to one source to the exclusion of all others. If this exclusive attachment continues as the child grows, the dependency is nurtured
Nursing interventions: dependent personality disorder
Evaluate client’s ability for self-care
Avoid doing things that the client is capable of doing
Help client identify assets and liabilities
Emphasize strengths and potential
Encourage client to take responsibility for own opinions
Point out when client negates own feelings or opinions
Encourage client to make choices
Obsessive compulsive personality disorder
Pre-occupied with orderliness, perfectionism, control, lists, rules
Perfectionism that interferes with task completion
Excessively devoted to work and productivity
Over conscientious and inflexible
Unable to discard worn out or worthless projects
Reluctant to delegate tasks or work with others
Obessive compulsive personality disorder facts
Prevalence: Relatively common and more prevalent in men than women.
Predisposing Factors:
The parenting style in which the individual tends to be “over controlled.” Parents expect their children to live up their imposed standards of conduct and condemn them if they do not. Praise for positive behaviors are bestowed on the child with much less frequency than punishment. Children learn and grow the understanding of what “not” to do in order to avoid punishment
Usually in first borns
OCD vs. OCPD
OCD: client recognizes OCD behaviors and wants to be rid of them
Recurrent and persistent thoughts, urges or images and attempts to suppress them
Obsessions or compulsions are time consuming
This is when you will wash your hands 5 times before leaving the house even if it means being late for an appointment
OCPD: Many times the client sees the symptoms as positive and a part of their success.
Preoccupied with details, lists, rules, organization
Shows perfectionism
Excessively devoted to work and productivity
Nursing implications for personality disorders
Identify behavioral patterns or maladaptive symptoms
Acknowledge that patient will rely on maladaptive coping skills
NANDA for personality disorders
Ineffective Coping
Ineffective Role Performance
Risk for Other-Directed Violence
Risk for Self-Injury
Risk for Self-Mutilation
Social Isolation
Self-Esteem Disturbance
Nursing process for personality disorder
SAFETY!!! --number one priority
Consistency
Limit Setting
Boundary Setting
Appropriate self-disclosure
Ongoing staff support and supervision
Pharmacology for personality disorder
No new medications
The medications will be used to treat symptoms and other related psychiatric conditions:
Antidepressants and anxiety agents for depression/anxiety
Mood stabilizers and antipsychotics for aggression/mood stabilization
How do you treat personality disorders
Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy(DBT) are “Gold Standard” treatments
Teach positive coping skills/strategies
Other psychotherapy (individual), group therapy and case management
Behavioral therapy
Changing behavior is the key to treating problems
Behavior is learned and has consequences.
Teaches ways clients ways to decrease anxiety or avoidant behavior and gives client’s opportunities to practice techniques.
Includes relaxation training and modeling
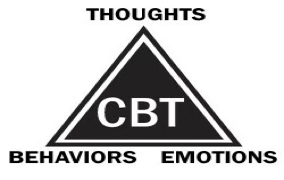
Cognitive behavioral therapy (CBT)
Aaron Beck – Based on personality theory that asserts how one thinks largely determines how one feels and behaves
Short-term, goal-oriented psychotherapy treatment that takes a hands-on, practical approach to problem-solving.
Changes people’s attitudes and behavior by focusing on the thoughts, images, beliefs and attitudes that are held
GOAL – Modify negative thoughts that lead to dysfunctional emotions and actions. Recognize dysfunctional cognitions, how the cognitions contribute to one's feelings, and change one’s behavior
Automatic thoughts: thoughts a client has
Schemata – Unique assumptions about ourselves, others and the world around us
Cognitive distortions
Automatic thoughts that are often irritation and lead to false assumptions and misinterpretations
Unhelpful thinking styles
All or nothing thinking
Mental filter
Jumping to conclusions
Emotional reasoning
Labelling
Over generalizing
Disqualifying the positive
Magnification (catastrophising) & minimization
Should/Must
Personalization
CBT example
SCENERIO – Billy has been in counseling for depression. His therapist’s secretary called and cancelled this week’s appointment and rescheduled.
Client’s automatic thought– “My therapist is disgusted with me and wants to avoid me.”
Emotion – Sadness, rejection, and hopelessness.
Behavior-Decides to call off work and return to bed.
Reframing – There is no evidence to believe that I disgust my therapist. Why would they have rescheduled if he really didn’t want to see me?
Therapeutic tools used in cognitive therapy
Priority restructuring: assisting clients to identify what requires priority.
Journal keeping: clients can write down stressful thoughts to process
Assertiveness training: teaches client to express feelings and solve problems in a nonaggressive manner.
Monitoring thoughts: helps client to be aware of negative thinking.
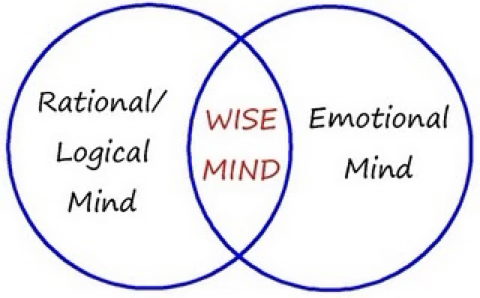
Dialectical Behavior Therapy (DBT)
A form of CBT
Developed by Marsha Linehan, PhD. In the 1980’s
Primarily used for personality disorders (Borderline) that include self-injurious and suicidal behaviors. (Ineffective coping skills)
Based on the belief that the primary problem for this client is emotional dysregulation.
More effective treatment for personality disorders than medication.
Gradual behavior changes
Provides acceptance and validation for clients
MODES OF TREATMENT (Is a year long therapy)
Group skills training (weekly for up to 1 year)
Individual psychotherapy
Telephone contact
Therapist consultation/team meeting
4 modules (skills) of DBT
Mindfulness
Interpersonal Effectiveness
Distress Tolerance
Emotion Regulation
5 functions of DBT
To enhance behavioral capabilities
To improve motivation to change
To ensure that new capabilities generalize to the natural environment
To structure the treatment environment such that the client and therapist capabilities are supported and effective behaviors are reinforced
To enhance therapist capabilities and motivation to treat clients effectively
Ways to help cope with that emotional toll…
Talk to colleagues about feelings of frustration
Clear and frequent communication with all members of the treatment team will minimize manipulation by the client
Do not take anything personally!
Set realistic goals and remember that changes in clients with personality disorders takes time. Be patient!
Caring for personality disorder clients: an emotional toll on nurses
Understand your own reactivity
Self-awareness
Countertransference: the nurse’s behavioral and emotional response to the patient. (ie: may become angry with an antagonistic client or feel flattered when showered with attention from the client)
Labels of Stigma
Supervision