cornea II hypersensitivity, corneal damage
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
what is a hypersensitive reaction (3)
an overreaction of the immune system to an antigen or allergen which would not normally trigger an immune response
The normally protective immune system responds abnormally, potentially harming the body
trigger can be an allergen (abnormal response to something outside the body) / autoimmune disease (abnormal response to something IN the body)
state the conditions that arise due to hypersensitive reactions (5)
marginal keratitis !!!
contact lens associated keratitis !!
AKC, VKC - see previous lectures for these !! atopic and vernal keratoconjunctivitis
Phlyctenulosis !
Ocular rosacea !!!
what is the aetiology of marginal keratitis (1)
•Toxic or hypersensivity reaction to bacterial exotoxins
what are the predisposing factors of marginal keratitis (2)
•Blepharitis (Staphylococcal)
•Current/recent upper respiratory tract infection, rosacea or Phlyctenulosis
what are the symptoms of marginal keratitis (3)
•Discomfort, irritation, FB sensation
•Lacrimation (production/shedding of tears - watery eye)
•Red eye
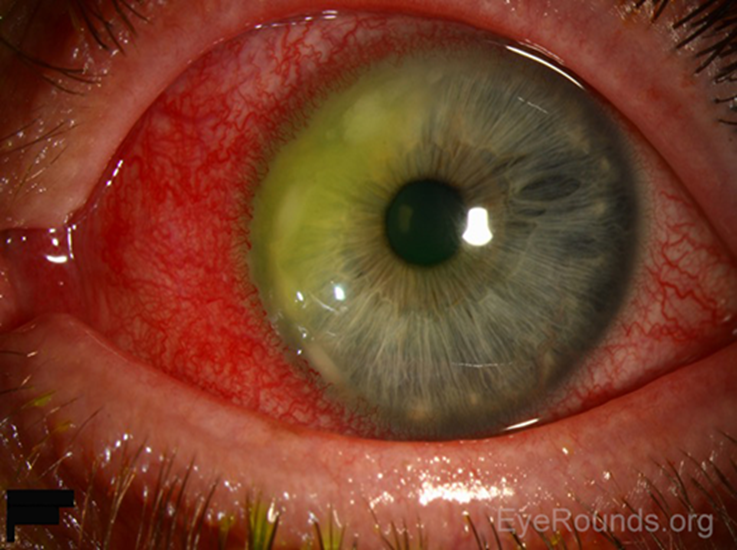
what are the signs of marginal keratitis (6)
•Shallow ulcer:
•Round, arcuate (curved pattern/shape) , single or multiple
•Usually parallel to the limbus but separated by a clear corneal zone
•+/- Stains with fluorescein
•Hyperemia and oedema of adjacent bulbar conjunctiva
•No anterior chamber involvement
what is the optometric management of marginal keratitis (6)
•Self-limiting - may scar / treatment to relieve symptoms & shorted the clinical course
•Treat underlying blepharitis
•Ocular lubricants - symptomatic relief
•Systemic analgesia (pain killers)
•Refer routinely if persistent or recurrent / refer same day if risk of infection
•Contact lens wearer - consider microbial keratitis (acanthaomeoba) or contact lens related
how is marginal keratitis managed by ophthalmologists (3)
•Microbiological cultures of lesion and lid margin
•Antibiotic treatment for blepharitis
•Topical steroid to calm inflammation
what is the aeitology of contact lens associated keratitis (1)
•Inflammatory (NOT infective) response to bacterial antigens (lens or lid margin) in hydrogel CL wearers
what are the predisposing factors of CL associated keratitis (2)
•Bacterial bioburden - eyelids, CL, CL cases, poor hand hygiene, increased risk in extended wear
•Smoking
what are the symptoms of CL associated keratitis (6)
may be asymptomatic
Moderately red
sl watery eye
mild FB sensation
mild photophobia
Symptoms improve soon after lens removed
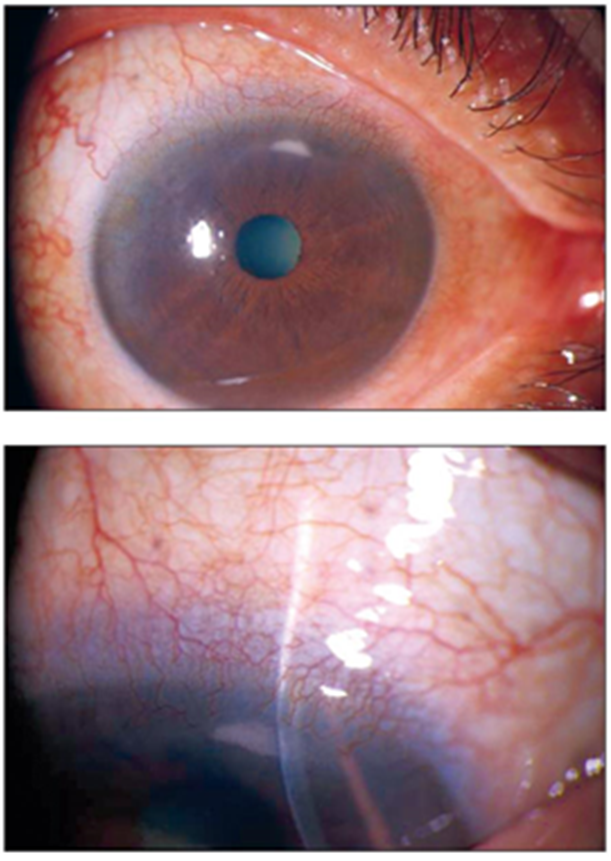
what are the signs of CL associated keratitis (5)
•Single or multiple peripheral anterior stromal infiltrates (<1 mm diam), round, usually stain
•Mild conjunctival hyperaemia
-mild epiphoria
•Quiet AC, no lid oedema
Usually unilateral
what is the optometric management of CL associated keratitis (5)
•Temporarily discontinue CL wear
•Tends to resolve quickly - 48 hours (2-3 weeks infiltrates)
•Refit with daily disposable CLs
•Address associated factors (hand hygiene, contact lens care, lid hygiene)
•Patient education - risk factors, prognosis
what is the aetiology of Phlyctenulosis (3)
•Rare in UK, common in Africa
•Type 4 hypersensitivity response
•Associated with systemic disorders (Behçet's disease, tuberculosis, HIV, rosacea)
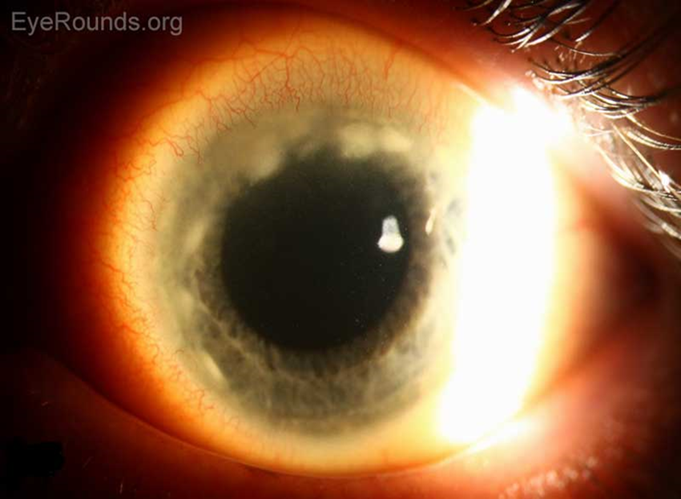
what are the signs of Phlyctenulosis (3)
•Phlycten (subepithelial nodules) located in conjunctiva or cornea
•Conjunctival phlycten - inflamed nodules - pink, reddish, near limbus, may be tender, surrounded by conjunctival hyperaemia
•Corneal phlycten - grey nodules associated with superficial neovascularisation

what is the treatment of Phlyctenulosis (1)
topical steroids
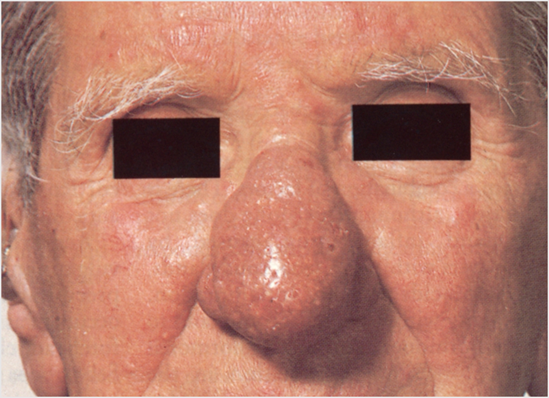
what is rosacea (3)
•Chronic skin disease (face)
•Redness and cutaneous telangiectasia (small, dilated blood vessels visible on the skin)
•Sebaceous hyperplasia - benign enlargement of sebaceous (oil) glands in the skin
what is the aetiology (2) and prevalence (3) of rosacea
•Unknown aetiology
•Immunological factors, skin surface microorganisms & reactive blood vessels are involved
•Common - Prevalence 10%
•40-60 year olds, M:F 1:2
•Ocular manifestations in 60%
what are the cutaneous (skin related) signs of rosacea (3)
•Facial flushing/chronic hyperaemia of the nose, forehead & upper cheeks
•Breakouts or papules
•Rhinophyma (bulbous nose) in severe cases

what are the symptoms of ocular rosacea (3)
•Discomfort, burning, itching, FB sensation
•Dry eye
•Photophobia, blurred vision
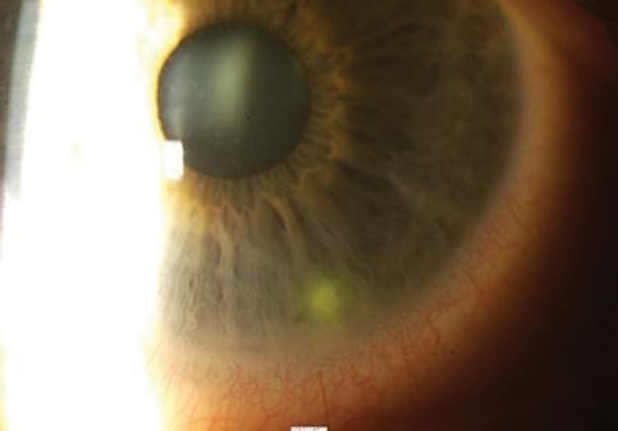
what are the signs of ocular rosacea (4:4)
•Hyperaemic thickened lids
•Telangiectasia (small, dilated blood vessels that are visible) of lid margins
•Chronic blepharitis (MGD)
•Recurrent chalazion/hordeolum
•Tear film instability

•Cornea (up to 30% of rosacea pts)
•Punctate corneal staining (lower 1/3rd)
•Corneal ulcers & thinning (can perforate)
•Ultimately peripheral neovascularisation and scarring

what is the optometric management of ocular rosacea (4)
•Advice on avoiding triggers (spicy foods, alcohol, heat, cosmetics, soap)
•Omega 3 fatty acid supplementation
•Management of blepharitis, chalazion etc.
Ocular lubricants
how is ocular rosacea managed by ophthalmologists (3)
•Oral antibiotics (tetracycline)
•Topical steroid for management of severe corneal disease (may accelerate stromal thinning)
•Systemic immunosuppression in very severe cases
what conditions are related to corneal damage/arise from corneal damage (5)
Photokeratitis !!
Exposure Keratitis !!
Neurotrophic Keratopathy !
Corneal abrasion/recurrent corneal erosion !!
Foreign Bodies !!
what is photokeratitis and its aetiology (4)
•Exposure to UVB or UVC
•Welding arc, sun (reflection snow, water), tanning lamps
•Radiation absorbed by corneal epithelium
•Delay of 6-12 hours
what are the symptoms of photokeratitis (2)
•Mild cases: irritation & FB sensation
•Severe cases: Pain, redness, photophobia, blepharospasm, lacrimation & blurring of vision
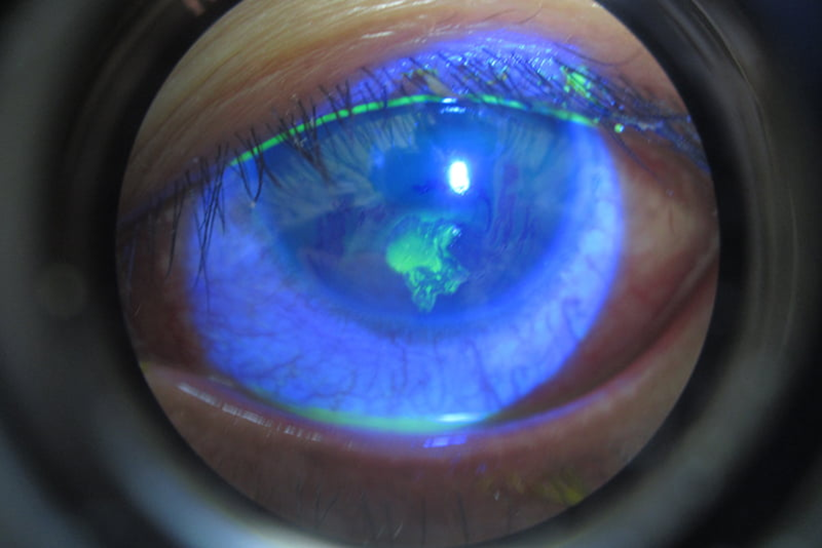
what are the signs of photokeratitis (7)
Bilateral
lid chemosis and redness
conjunctival hyperaemia
epiphoria
PEE - punctate epithelial erosions
blepharospasm
lacrimation, blurred vision
what is the management of photokeratitis (3)
•Reassurance - and eye protection in future
•Recovery in 24-48 hours
•Cold compress, rest with eyes closed
what is exposure keratitis (4) see lids lectures for details
incomplete closure of lids - cornea exposed
tears not spread evenly - drying out
leads to punctate epithelial staining - epithelial damage
uncomfy for patients
what is Neurotrophic Keratopathy (2)
•Impairment in corneal sensation
-and impairment of epithelial repair
predisposition and risk factors of Neurotrophic Keratopathy (3)
•Predisposition to inadvertent trauma and reduced healing
•Delayed clinical presentation
•HSK, HZO, CL wear, trauma to trigeminal nerve (irradiation, compression e.g. acoustic neuroma), diabetes, drugs (e.g. systemic beta-blockers)
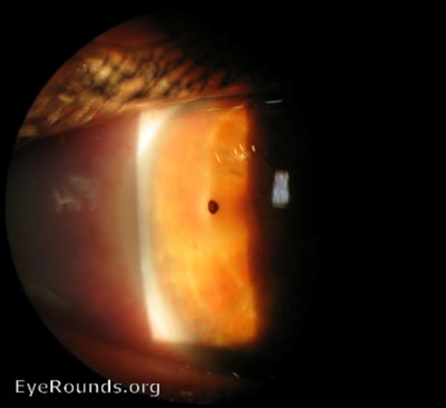
what is a corneal abrasion (3)
•Trauma to the eye surface
•H/o - history of - dust, sand, CL, fingernail, tree branch
•Usually recovers 3 days
what are the symptoms of a corneal abrasion (2)
•Painful, red, watery eye
•Photophobia, FB sensation
what are the signs of a corneal abrasion (1)
•Epithelial defect which stains with fluorescein - Hyper fluorescence indicates a deeper (stromal) wound

what is the management of a corneal abrasion (6)
•Rule out foreign body
•Antibiotic ointment
•Cease contact lens wear
•Systemic analgesia (paracetamol/Ibuprofen), cycloplegic for pain relief
•DO NOT patch
•NB: Complete epithelial basement membrane repair takes around 3 months
what is the aetioogy of recurrent corneal epithelial erosion (3)
•Recurrent epithelial breakdown - due to poor adhesion of epithelium to the basement membrane
•Follows an episode of superficial trauma
•Epithelial dystrophies - inherited — remember to check for this
what are the symptoms of Recurrent corneal epithelial erosion (3)
•Sudden onset, unilateral sharp pain, on eye opening (waking or during the night)
•Lacrimation and photophobia
•May recur over weeks, months or years
what are the signs of Recurrent corneal epithelial erosion (1)
•Epithelial erosion, stains with fluorescein - ‘loose’ edges - ‘slipped rug’ appearance
what is the optometric management of Recurrent corneal epithelial erosion (3)
•Ocular lubricants ++
•Ointment at night time for at least 3/12 after last episode
•Refer routinely if persistent or large defect
what are the secondary care options for recurrent corneal epithelial erosion (3)
Lubricants, cycloplegia, antibioticointment
Bandage contact lens - do NOT pad
Debridement (medical removement) of loose epithelium - excimer laser photo-therapeutic keratectomy, alcohol debridement, diamond burr superficial keratectomy
what are foreign bodies/cause (1)
Wind blown, high velocity, DIY/gardening
what are the symptoms of foreign bodies (3)
Unilateral
FB sensation/pain
red, watery and blurry
what are the signs of foreign bodies (3)
•Foreign body adherent to the ocular surface
•Rust ring - Oedema and infiltrate around a rust ting indicates a long standing metallic FB
•Linear corneal scratches (always evert the lids - check both eyes, conjunctiva and cornea)

what is the management of foreign bodies (6)
•Careful history (cause and prognosis) - History may indicate penetrating trauma (e.g. high velocity particles) - check the fundus
-Assess the depth of the FB (slit lamp optical section)
•Superficial FB - flush out with saline, normally no referral
•Deeper FB - remove with needle/burr or Alger brush (trained)
•Same day referral to eye clinic
-Consider an antibiotic ointment post removal to reduce the risk of infection