Carbohydrate metabolism
1/69
Earn XP
Description and Tags
FNN200
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
Carbohydrate oxidation
Chemical energy in nutrients stored and released through metabolic reactions
cellular oxidation of 1mol glucose releases net DeltaG of 280 kcal/mol
ATP
converted to adp results in deltaG of -12kcal/mol
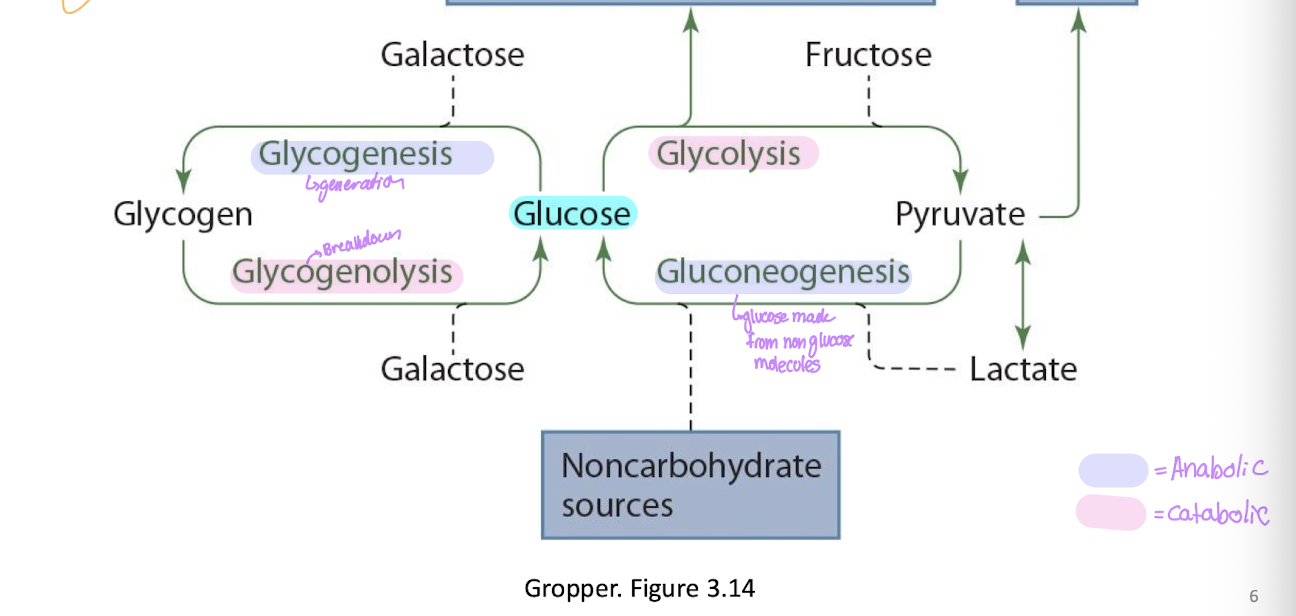
Different pathways of carb metabolism
Glucose → glycolysis + fructose → pyruvate →
TCA cycle
Lactate
+ non carbs → Gluconeogenesis
Glucose + galactose → Glycogenesis → glycogen → glycogenolysis +galactose →glucose
Covalent modification
activates/inactivates enzymes
removal/addition of phosphate to or from enzyme
phosphorylaze b to a in glycogenolysis
Reversibility of enzymes
most reactions are reversible with the same enzyme
unidirectional may be able to make the same thing but it would require a new enzyme for that
may be because of energy requierments
concentration gradients etc
Compartmentalization
enzyme within a cell and is only active within that cell
brings enzymes into close proximity
controls metabolic pathways
krebs
Induction in enzymes
changes in concentration of inductible enzymes
increased activity
often occurs through the action of hormones
Allosteric regulation - main enzyme regulator
may be positive or negative
can either allow or prevent the binding of a substrate to an active site
Common ones
ATP (-), ADP (+), AMP (+)
reaction metabolites (substrates or products)
other substances
3 key regulatory steps and enzymes
step 1: HK and GK
hexokinase (muscle/adipose) and glucokinase (liver and pancreas)
Step 3: PFK
Phosphofructokinase
committed step
Step 10: PK
Pyruvate kinase
1st phase of glycolysis
Glucose is acted on by either HK or GK depending on where in the body
HK in muscle and adipose
GK in liver and pancreas
The glucose is phosphorylated in a process which uses an ATP
this is non reversible and traps the glucose in the cel
allosteric regulation to inhibit the kinase to stop taking in when it is full
Converted into Glucose-6-phosphate
Fructose-6-kinase is then acted on by PFK to create fructose-1,6-bisphosphate
this is the committed step of glycolysis
GK vs HK
GK (Glucokinase is found in liver and pancreas)
this has a higher Km because there must be a higher regulation of blood glucose
HK - hexokinase is in the muscle and adipose tissue
lower Km because it does not need to have the same level fo regulation and they want more glucose in them
PFK-1
Phosphofructokinase
converts fructose -6-phosphate into Fructose-1,6-bisphosphate
Committed step of glycolysis
irreversible so it tells the cell that it is going to do glycolysis
Allosteric regulation
negative: atp, Citrate
Positive: AMP, fructose-2,6 bisphosphate/PFK-2
Kinase
catalyzes transfer of phosphate group
Hexokinase
located in muscle, brain and adipose itssue
allosteric inhibition by glucose 6- phosphate (product)
Low Km function at max velocity at fasting blood glucose
not induced by insulin at normal individuals
not induced by insulin in insulin resistant individuals
Glucokinase
liver and pancreas
not inhibited by product (glucose-6-phosphate)
High Km: functions at max only when glucose levels are high like followign a high carb meal
Induced by insulin in normal inidviduals
not induced by insulin in insulin-resistant individuasl
PFK1 vs PFK2
PFK 1 is responsible for the conversion of Fructose-6-phosphate into fructose-1,6-bisphosphate
positive regulation from fructose -2,6-bisphosphate
PFK2 is respobsible for conversion of Fructose-2,6-bisphosphate into fructose-6-phosphate
this is positively regulated by Glucagon
PFK 2 is also responsible for the active change of Fructose-6-phosphate into fructose -2,6-bisphosphate
this is positively regulated by insulin
Energy yield of glycolysis
2NADH + 4 ATP
then some are used so the ent is actually
2 ATP and 2 NADH
one is used by HK or GK and the other by PFK
2nd phase of glycolysis
NAD+ is converted to NADH (x2)
ADP converted to ATP (x2)
Phosphoenolypyruvate (x2) is acted on by pyruvate kinase (PK)
creates pyruvate (x2)
also makes ATP (x2)
Pyruvate kinase (PK)
irrevertible
allosteric regulators
negative: ATP
Positive: AMP and fructose-1,6-bisphosphate
Hormonal regulators
negative: glucagon cause it wants body making glucose
Positive= insulin cause it wanst glucose in so it wants glycolysis to occur
Fate of pyruvate in anaerobic
skeletal muscles during exercise
tissues with no mitochondria or vascularization
rbcs, cornea, lens of eye
Lactate dehydrogenase acts to turin it into 2 lactate and then it will become lactic acid and leave the cell
the acid will return to the liver where it will be converted to pyruvate
Fate of pyruvate aerobic
2x pyruvate will enter the mitochondria and go through the krebs cycle with 2 acetyl-CoA
Fructose and metabolism
always committed to glycolysis because it enters the cycle after PFK
all will be oxidized and may be stored in fat more
Acted on by fructokinase
uses ATP
creates Fructose-1-phosphate
then will become Fructose-1,6-bisphosphate
Galactose in glycolysis
Galactokinase
Uses atp
creates galactose-1-phosphate
becomes glucose-1-phosphate
glycogen synthase can make it into glycogen which is where most galactose is stored
Some will go to become Glucose-6-phosphate to go through glycolysis
depends on the energy state of the cell
Glycogenesis
Glucokinase is used to convert glucose → glucose-6-phosphate
then glycogen synthase is used to create glycogen
Glucose-6-phosphate
removes P
absent in muscle
liver glycogen contributes to blood glucose in times of need
muscle only produces glucose for the tissue
Occurs in the liver
Gluconeogenesis
stimualted by glucagon and epinephrine
occurs in the liver
phosphorylase glycogen, makes glucose-1phosphate whthen phosphotase makes glucose to go to blood glucose
Major sites of glycogen storage
liver (7% weight)
Muscle (1% weight)
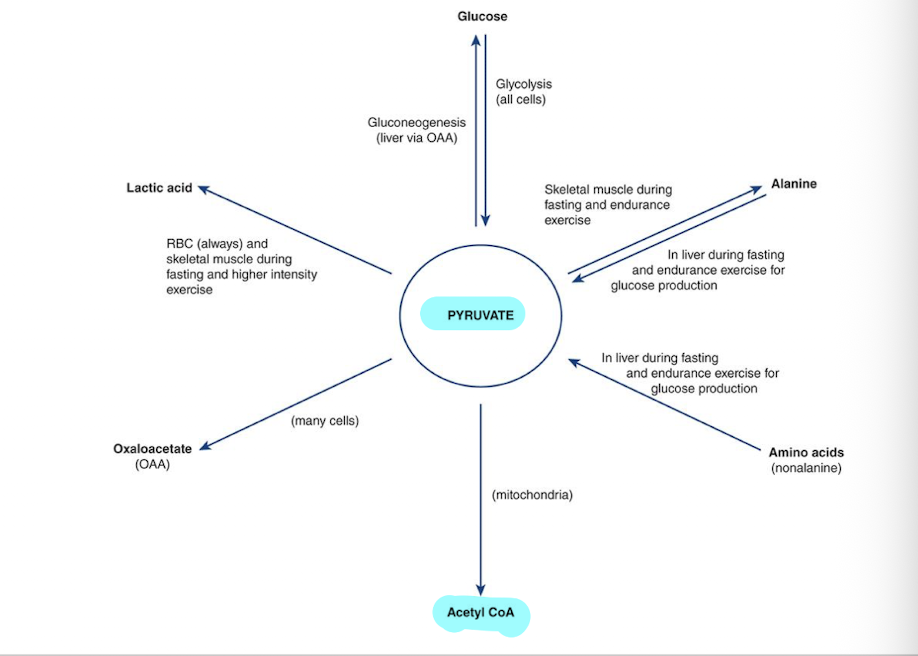
Different sites pyruvate can go to
acetyl CoA
Oxaloacetate
lactic acid
glucose (comes from glycolysis but can go through gluconeogenesis)
alanine (muscles)
amino acids can become pyruvate
Krebs cycle/TCA Cycle
Step 1 Involves:
Oxaloacetate + Acetyl CoA
undergoes citrate synthase
creates citrate
Energy Yield per pyruvate (x2)
3 NADH
1 FADH2
1 ATP
2 CO2
TOTAL =
6NADH
2 FADH
2 ATP
4 CO2
Krebs regulators
ADP = positive
NAD = positive
ATP = negative
NADH = Negative
Electron transport chain
this is aerobic oxidation
O2 is the final electron accepter
each thing fuels the next
NADH gives up hydrogen to FADH
The final step is a ATP synthase which allows H+ back through creating the change from ADP to ATP
PRODUCTS
1 NADH produces 3 ATP
1 FADH Produces 2 ATP
Total ATP calculations
one carb gets 36-38 atp + heat
10 NADH x 3 ATP = 30 ATP
2FADH x 2 ATP = 4 ATP
+ 4 ATP from glycolysis + TCA cycle
Total becomes 38 ATP/ mol of glucose
sometimes they are lost in the transport of NADH into mitochondria so sometimes there is 36
Concersion of cellular energy into kCal
1 mol of carb → 36/38 ATP (40% of potential energy) + heat (60% of potential energy)
1 mol of glucose is equivilent to 180gm
ATP = 7.3kcal/mol
38 ATP = 280kcal (38×7.3)
280 kcal/180gm = 1.55 kcal/gm (40% of potential enery)
remaining 60% is released as heat
TOTAL POTENTIAL ENERGY PER GRAM
1.55 × 100)/40 = 3.89 kcal/g
roung up to 4kcal/g
Lipogenesis
creates triglycerides when there is excessive carb intake
when the cells have enough energy there will not be the krebs cycle and therefore fatty acid syntehsis will occur instead
it will also activate carb response elment binding protein
Phosphorylase
Phosphorylase B must become phosphorylase a in order to convertn glycogen into glucose -1-phosphate which is required to increase blood glucose
works with glucose -6-phosphotase
Phosphorylase induction and covalent modification
hormonal
epi and glucagon increase the conversion b-a (activates)
insuling increases a-b (inactive)
Metabolic regulators
p is the required substrate for phosphorylase
Ca++ increases the activity of phosphorylase kinase
AMP and IMP can increase the activity of phosphorylase b independent of the conversion to a
Protein phosphotase is what inactivates (a→b)
Importance of blood glucose regulation
energy source
RBC exclusively use glucose
brain and neurons need fuel nonstop and they prefer carbs
no fuel can be stored
ketones are alternative fuels which require only small amounts of glucose
Hyperglycaemia
blood vessel damage, glycation (proteins which should not have glucose but do), tissue damage
Hypoglycaemia
potentially irreversible brain damage, confusion dizziness, seizures, loss of consciousness
TCA cycle glucose
glucose is essential for energy to be obtained from all macronutrients
pyruvate → acetyl CoA → citrate and oxaloacetate
Oxaloacetate
first step of TCA cycle
Oxaloacetate + Acetyl CoA → citrate
Cannot occur without a constant supply of oxaloacetate
also a part of gluconeogenesis
Can be made from pyruvate independent of TCA cycle as well
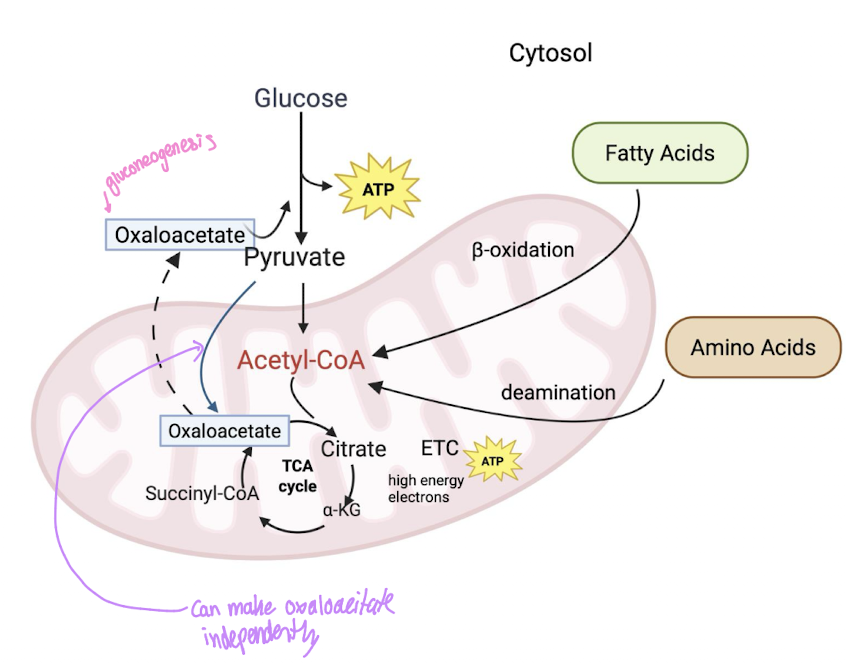
Pyruvate creation of Oxaloacetate
can be done independent
uses a different enzyme
ensures that the TCA cycle can continue to operate
Gluconeogenesis
mainly occurs in liver
Lactate: Cori Cycle
lactic acid in blood
liver → pyruvate
Glycerol
triglycerides
Free Fatty Acids do not make glucose
Glycerol does make a small amount of lgucose
Glucogenic amino acids
there contribute to pyruvate or oxaloacetate production
Low dietary CHO
Glucogenic amino acids will make oxaloacetate and pyruvate
Ketogenic and fatty acids will not
Ketone formation - absence of glucose
Produced in liver
can be used for energy
brain can adapt to use them
low oxaloacetate so itll use acetyl-CoA
this is in fatty acids
Ketosis
accumulation of ketones in the blood
excreted via kidney in urine
require increased water intake to prevent
Mild → elevated levels
headaches, dry mouth, lack of appetite
Severe → blood acidity, coma and death
Allulose
fructose epimer
one carbon has a different orientation which changes how the body will respond to it
10% of the calories as regular sugar
occurs naturally in wheat, figs, raisins, maple syrup an dmolasses
absorbed similar to fructose (GLUT5) but is not recognisedd by fructokinase
GLUT5 into the endothelial cel and GLUT2 out
Fructokinase
responsible for the changing of fructose into fructose-1-phosphate
but does not recognize allulose so allulose is not going to be committed to glycolysis
Allulose
reduced glucose release from CHO
stimulated in vetro by bellisimo
Possible that it inhibits the a-amylases and therfore results in a lower spike in glucose when consumed with rice
Blood glucose - Hormonal regulation
B-cells
insulin
moves glucose into muscles, liver and into fat cells
immediately after a meal to bring down the blood glucose levels
anabolic to build glycogen stores
a-cells
glucagon
moves glucose from glycogen stores and gluconeogenesis back into the blood stream
occurs several hours after a meal so that blood glucose stays normal
Catabolic process
Stress and growth hormones
Raise blood glucose
Epi and norepi
thyroid hormones
glucocorticoids
growth hormones
Diabetes
most common disease associated with CHO metabolism
characterized by high blood glucose levels
inability of body to produce enough insulin or respond to insulin or both
Types of diabetes
gestational
during pregnancy
if untreated it can pass to baby with high birth reight → delivery complications
risk of obesity and type 2 diabetes in life
Type 1 (10%)
auto immune disease that destroys the pancreas
treated with insulin injections
the body is unable to produce insulin
Type 2 (90%)
cells have a decreased sensitivity to insulin
decreased insulin production (B-cell dysfunction) or response to insulin (insulin resistance)
Normal blood glucose levels
fasting : 4.5-5.5mmol/L
Fed: up to 7.8 mmol/L
Diabetes
Diagnosis: Fasting blood glucose >7.0mmol/L
Glycosuria: 10mm/L
glucose in urine cause it was so high in the blood
Pre-diabetes
impared glucose tolerance or glucose intolerance
Fasting glucose levels
Normal: <6
Prediabetes: 6.1-6.9
Diabetes: >7
2 hours post eating glucose levels
Normal <7.8
prediabetes 7.8-11
diabetes >11
Type 2 diabetes
Step 1: Increased insulin secretion but it is still conpensating
there is a decreased sensitivity to insulin which is why more is being produced
Blood glucose is normal but hyperinsulinemia
Step 2: Prediabetes
increased insulin secretion but only partial compensation
Blood glucose is increased and stil hyperinsulinemia
Step 3: Beta-cell exhaustion
increased blood glucose and either hyper or hyopinsulinemia
there may be increased or decrease in the insulin secretion depending on insulin functions
Diabetes risk factors
obesity, age, lifestyle, genetics, ancestory, very complex
Diabetes treatments
weight loss
exercise
diet
medication
Grains and starches examples of 3 categories
Low GI (55 or less)
carrots - cooked
green peas
Winter squash
Medium GI (56-69)
corn
parsnip
pumpkin
High GI (70+)
corn starch
gnocci
rice crackers
Fruits in the 3 categories
Low GI (55 or less)
apple
apricots
berries
Medium GI (56-69)
ripe bananas
cherries
grapes
High GI (70+)
overripe banannas
breadfruit
Dairy in the 3 categories
Low GI (55 or less)
almond milk
cottage cheese
cows milk
Medium GI (56-69)
oat milk
processed cheese
High GI (70+)
rice milk
Proteins in the three categories
Low GI (55 or less)
Black beans
chickpeas
hummus
Medium GI (56-69)
Lentil soup
split pea soup
High GI (70+)
broad beans
Differences in the CFG plate and the Diabetes canada plate
diabetes has starchy veg grouped in with the whole grain portion
it includes more plant protein sources
uses more greens
Genetic screening of newborns for errors in metabolism
protein metabolism disorders
fatty acid oxidation disorders
carbohydrate metabolism
Galactosemia
all newborns screened
Deficiency of Galactokinase or Galactose-1-phosphate urdiyltransferase (GALT)
converts galactose-1-phosphate to glucose-1-phosphate
Galactose accumulates in blood and tissues
failure to thrive, liver damage, sepsis, death
Treatment
galactose restricted diet for life
GALT
enzyme responsible for the conversion of Galactose-1-phosphate into glucose -1-phosphate
mcardle disease
type 5 glycogen storage disease
onset in childhood in skeletal muscles
deficiency in muscle glycogen phosphorylase: cant break down glycogen to release glucose so glycogen accumulates
Results in
fatigue, exercise intolerance
muscle weakness, soreness, cramps
higher in protein (low carb, keto may help-
can prevent glycogen breakdown
Goal is to prevent hypoglycemia or muscle symptoms
GLP-1 agonists
mimic the natural affects of GLP
inhibit motility in the intesting so that your body tell sthe brain that you are full
Wegovy
increases satiety
Type 2 diabetes targets are
Semaglutide
Ozempic - not actually approved by weightloss
cardiosystem
increasing insulin synthesis ans ecretion
B-cell proliferation - cannot get levels back to normal but might be able to get some function back
decrease glucagon synthesis and secretion
Increase glucose uptake by fats
incake lipolysis
increase uptake in muscles and more synthesis of glycogen
lower gluconeogenesis
Exercise training impacts glucose metabolic pathways
higher GLUT4 density and signaling in muscle
translocation to take in glucose and increase uptake
insulin and muscle contraction
exercise and can take in more glucose form blood
increased glycogen synthase activity
glycogen storage → glucose -1-phosphate to glycogen
better in insulin signaling
more translocation
Increased number and size of mitochondria
more fat for fuel → spares glucose
all burn in Kreb
lower overall fat through increased fat consumption
Carb Loading
Goal → to maximise muscle and liver glycogen stores prior to prolonged endurance and exercise
phase 1 → deplete the glycogen from muscles
phase 2 → CHO load to increase the glycogen storage