Behavioral Health Nursing Lecture 1
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
31 Terms
Health
state of well-being, able to cope with normal stressors, able to reach potential
Illness
–psychiatric disorders that have a definable diagnosis and are culturally defined.
- Different amongst cultures
•Factors to consider: developmental, biological/genetics, or physiological

Mental health and illness continuum
–Well-being to Emotional problems to Mental Health problems
• Well-being: no major disruption in daily life from everyday stressors
•
•Emotional problems/concerns: mild to moderate distress and impairment in functioning
•
•Mental illness: marked distress and moderate impairment in functioning
Mental health risks
-Genetics
-Biological/physiological
-Prenatal exposures
-Social/economic factors: Stress
-Environmental factors
•Culture
•Laws
•State of Healthcare

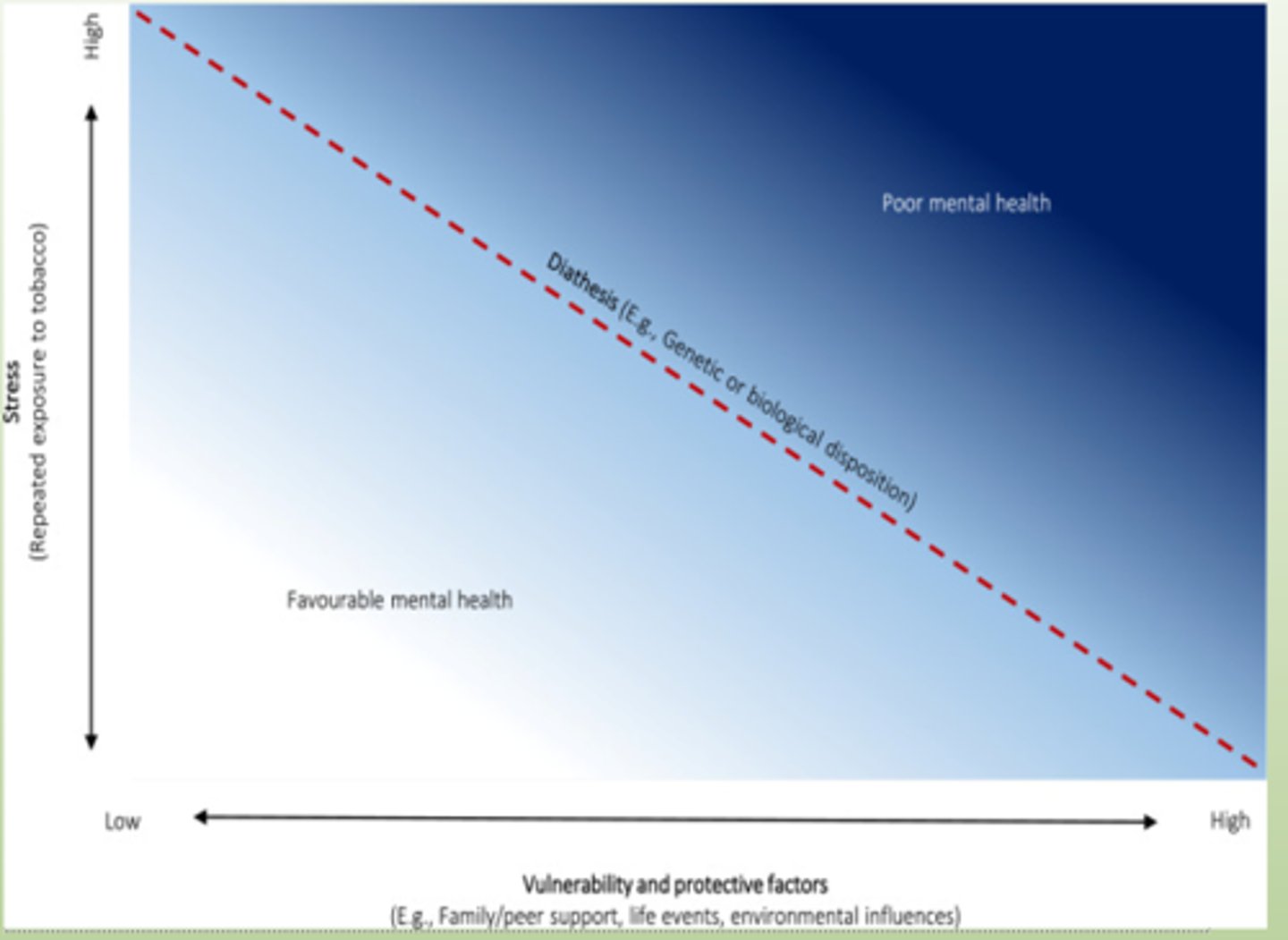
Nature vs Nurture
–Mental illness is not purely one or the other
Mix of nature and Nurture
High stress and low family support causes poor mental health
–Diathesis stress model
•Diathesis=biological predisposition
•Stress=environmental stress or trauma
Mental health affects
–Thinking (Delusions)- Disorientated thoughts
–Mood (Depression or other mood disorders)
–Self/Personality (Personality disorders)
–Experience (Disassociation)- disconnecting from reality
–Relational functioning (Impairment in relationships)
–Behavior
Mental health Trends
–Patients are more acutely ill
•High turnover of patients due to insurance coverage/lack there of
–Lack of mental health professionals
•Lack of outpatient care: people wait until they can’t anymore and end up in the ER
–Cultural diversity
•culturally competent: Take culture into consideration when providing care
•History of the Mental Health System
•Asylums: States responsibility to house the “insane.”
–1950s: Thorazine introduced: medication
–1960s: No Medicare or Medicaid coverage for psychiatric care
–1999: Olmstead decision = institutionalization violates rights
–Current: Continuum of care with both outpatient and inpatient options
mental health system
•Primary care:
–This is where many first seek treatment
–Often, mental health issues manifest as physical symptoms (stomachache etc.)
•Specialty care:
–Psychiatrists, PMHNPs, PAs, Psychologists, Social Work, Many others
•Patient center care home:
–Primary, mental health, acute/chronic, and preventative care all rolled into one!
•Community mental health centers:
–Free to low-cost care; includes many services
–Patients switched from institutions to CMH
mental health system
•Psychiatric home care:
–For homebound patients, Social Work and Nursing are involved
•Assertive community treatment:
–Intense case management
–Patients with severe illness, unable or unwilling to participate in other forms of treatment
•Intensive outpatient program/partial hospitalization program:
–Step down from inpatient
–PHP is more hours; they are “partially hospitalized. 5 days a week for 6 hours generally
–IOP is less usually 3-5 times a week for 3 hours
•Emergency care:
–Triage and stabilization
Mental Health System
•Crisis stabilization unit/observation:
–Short-term stay, 1-3 days
•General/Private Hospitals:
–Many have inpatient units, the average stay is generally 5-7 days
•State Hospitals:
–Severely ill patients are served here
–Extended stay
–May be forensic related (crime)
Flow for a patient with major depression may go like this
–Primary care: Generalized complaints, screened for depression PHQ9, is positive and admits to active suicidal ideation (may or may not be petitioned)
–ED: Sent to emergency for SI, triaged by a nurse, emergency physician petitions and certifies the patient
–Inpatient unit: Initial cert is good for 72 hours. Patients are seen by a Psychiatrist within that timeframe, generally in the first 24 hours. The patient is on the unit for 5-7 days on average, is stabilized, and discharged
–Outpatient: Could be PHP or standard outpatient treatment and follow-up
A petition form often is what sets this process in motion:
–State of Michigan Petition Form
–Remember, anyone can petition! If they think someone is suicidal
-Only physicians can certify!
Difference between a mental health unit and a standard medical unit?
–Made up of a multi-disciplinary team: social workers, activity therapists, physicians, psychiatric techs, and nurses
–Milieu: refers to the overall environment, physical and social/emotional
–Safety: heavily emphasized, staff receive additional training on de-escalation, physical design is unique to mental health (look for this on the units)
Differences in culture can cause barriers
–Language
• Phrases may mean something different to you vs. the patient.
•Actual language difference
–Stigma
–Misdiagnosis
•Most tools are based off Western world view
–Concepts of distress
•The way a culture understands illness
•Idioms: Sick as a dog etc.
•Explanations: demonic possession
Syndromes: Ghost sickness etc
Cultural Considerations
–Care should be congruent with the patient’s culture
–Need to ask the patient how they describe their illness
–Avoid stereotyping; even if you know about a culture, every patient is different.
–When it doubt ask, it is ok
Legal and Ethical Aspects
•Autonomy
–Right to make own decision
•Beneficence
–Act of doing good or benefiting others
•Nonmaleficence
–Do no harm
•Justice
–Duty to provide care equally
•Fidelity
–Loyalty
•Veracity
–Telling the truth
ethical dilemma
–occurs when two or more concepts are opposed
–Ex. Patient is threatening to harm themselves
•Beneficence dictates I stop them
•Autonomy states to let them make their own decision
Voluntary admission
Patient understands the need for treatment and seeks it out
involuntary admission
–Patient does not understand the need and is forced
–Involves a petition and certification
–Some criteria need to be met either
»They are a threat to themselves or others
»Or unable to care for self
»If these are not met, the patient should not be admitted against their will, this could be false imprisonment

Within the state of Michigan, a patient in a mental health unit cannot leave without
–an order
–holds true for both involuntary and voluntary
Patient's rights
•Right to treatment
•Right to refuse treatment
–If there is a court order, the patient must receive psychiatric meds.
–They can still refuse other medical treatment
•Right to informed consent
–Need to make sure patient has both capacity and competency
–Capacity: Ability to make informed decision
–Competency: legal term, the patient has the mental clarity to make decisions
–Guardians: some patients are not competent and therefore have a guardian to make decisions
–Right to confidentiality
seclusion and restraints
•If the patient is verbally threatening use a verbal response
•If the patient is physical then use a physical response
•Seclusion: confinement of a patient to a single room
•Restraint: Limiting a patient’s ability to move
–Physical
–Chemical: Sedation med
•An order is needed for these, a nurse can start one, but the physician needs to sign off and see the patient within the hour
-Restraints for adults
•Once seen within 1 hour by a physician, the restraint order is good for 4 hours, can be renewed for up to 24 hours
–Patient will be reassessed by a physician 24 hours after restraint
–Once restraints are discontinued, a new order is needed if the patient needs to be restrained again
-Duty to warn
•If the patient is a threat to another person, the healthcare team has a LEGAL responsibility to warn the potential victim
In this case, the right to confidentiality is overruled
Torts
•Intentional
–Assault- threat i.e. pretending to hit a patient
–Battery- actual physical harm
–False imprisonment
•Unintentional
–Negligence-Failure to perform ordinary care
–Malpractice- professional negligence, 5 elements are needed
»Duty to perform
»Breach of duty
»Cause in fact- the cause
»Proximate cause- was it foreseeable
»Damages
As a nurse, you have a duty to report negligence, irresponsibility, and impairment
if a colleague is impaired or irresponsible, talk with them if you feel comfortable; if you don't move up the chain of command
•Its for patient safety; that should be your focus
The Quality and Safety Education in Nursing (QSEN)
focused on
•Safety
•Provide patient-centered care
•Work in interdisciplinary teams
•Employ evidence-based practice
•Apply quality improvement
•Use informatics
Assessment
–Need to establish a rapport
–Obtain chief complaint
–Baseline physical assessment and vitals (includes skin assessment!)
–Assessing for risk to self or others
–MSE (mental status exam)
–Psychosocial assessment
–Establish mutual goals
–Create a plan of care
–Document findings
Take age into consideration
•Children- Can show regression (reverting to previous behaviors common in younger ages, thumb sucking, etc.)
–Caregivers can give you insight into behaviors
–Observing during play gives you great insight! (True for adults too!)
•Adolescents- very concerned with confidentiality, may not want you to share information with parents, need to be upfront and honest with them; some information may be shared
•Older adults- Some may have physical or mental deficits but remember everyone is different which is why we assess
Number one priority in a mental health unit
Safety