Post traumatic stress disorder
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
T or F: PTSD is the only disorder in the DSM where part of the etiology is the diagnostic criteria
TRUE!
Exposure to trauma = ethology + diagnostic criteria
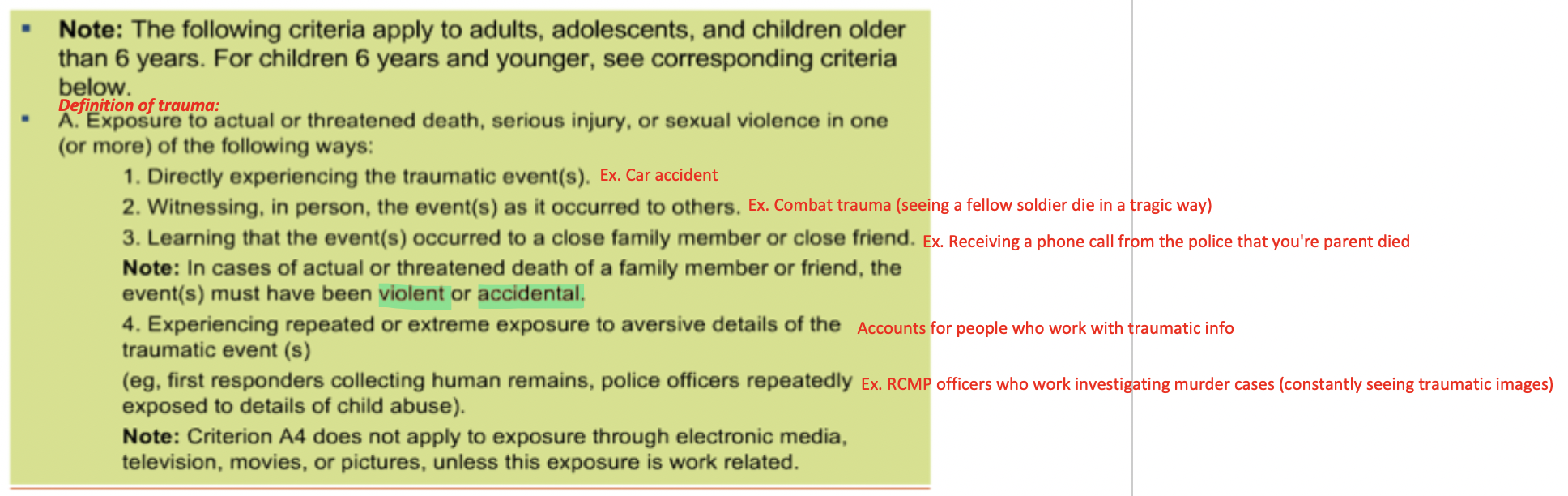
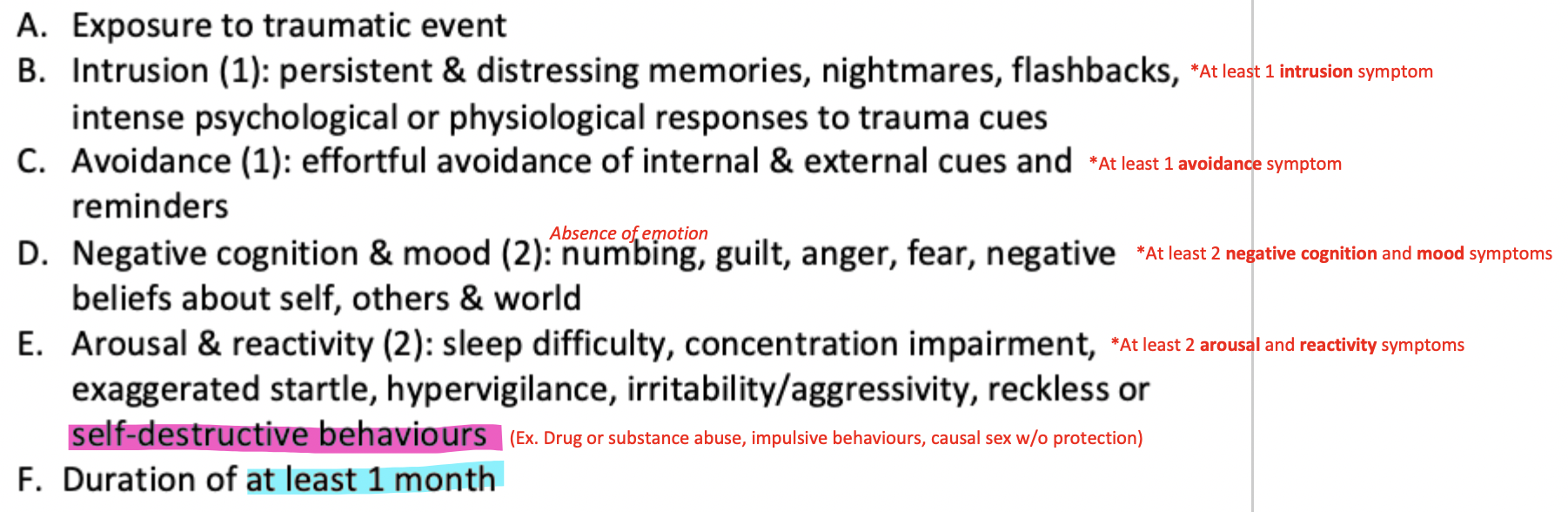
DSM 5 Criteria for PTSD
What is the difference between the duration between PTSD and acute stress disorder?
PTSD duration = at least 1 month
Acute stress disorder = 3 days to 1 month
What is more prevalent: PTSD or acute stress disorder?
Acute stress disorder
More common because symptoms drop off over a month (suggests that a lot of people are resilient to trauma)
What is the lifetime prevalence of trauma?
51.2% women
60.7% men
What is the lifetime prevalence of PTSD?
10.4% women
6.8% men
~42% in trans an non-binary folks
*Not everyone who experiences a traumatic event will develop PTSD
Lifetime prevalence of trauma vs. PTSD
The decrease in % of lifetime prevalence of trauma -> PTSD demonstrates how not everyone who experiences a traumatic event will develop PTSD
Ex. 51.2% women (trauma) -> 10.4% women (PTSD)
What is the epidemiology of PTSD in specific traumatized groups?
64% of BC residential school survivors
20.2% of sexual assault survivors
20% of 9/11 survivors
T or F: exposure of trauma is a necessary but not a sufficient cause of PTSD
TRUE!
Some people are more at risk of developing PTSD in the face of trauma compared to others
Pre-trauma
"Before the trauma"
Individual and environmental factors that already exist before the trauma exposure
Peri-trauma
"During the trauma"
The nature of the trauma itself, how the individual reacted/responded to the trauma, and what was happening in the environment during the trauma
Post-trauma
"After the trauma"
Individual and environmental factors that happen after the trauma
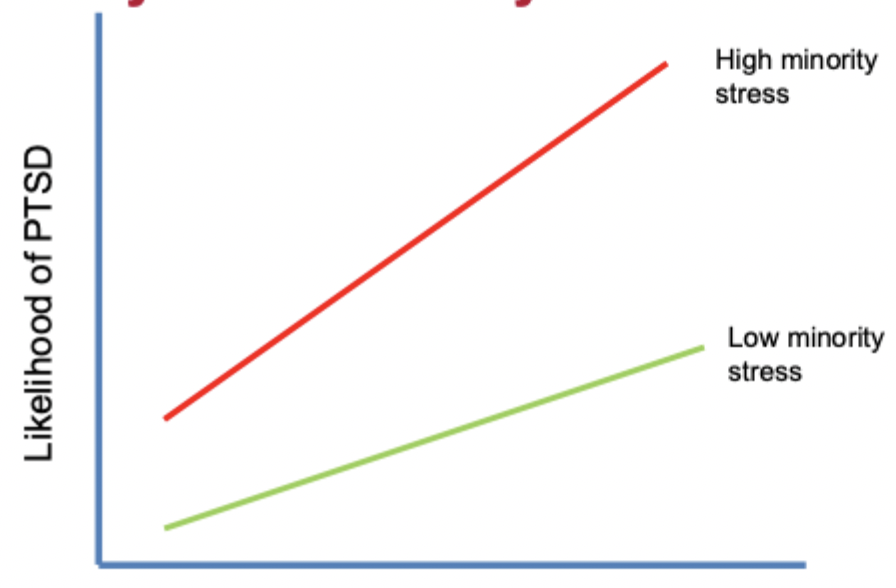
How does the minority stress theory explain PTSD?
Individuals with high minority stress have a greater likelihood of developing PTSD compared to those with low minority stres
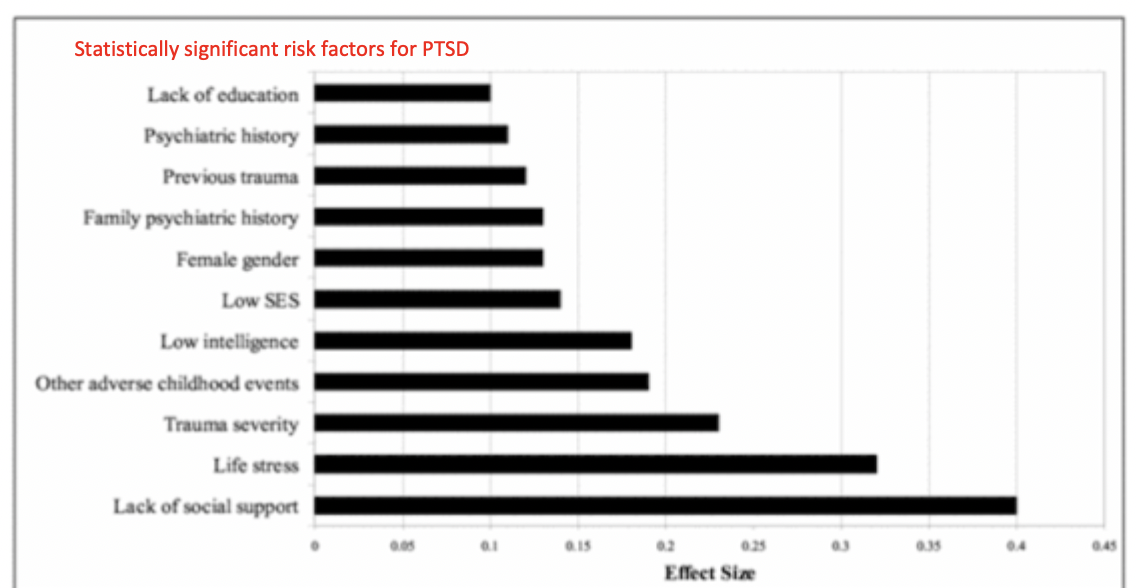
What are the major risk factors associated with PTSD? (Brewin et al., 2000)
Low levels of social support following trauma = BIGGEST risk factor for PTSD
Followed by life stress, trauma severity, other adverse child events, etc.
What are examples of negative appraisals of trauma?
Nowhere is safe
The next disaster will strike soon
I attract disaster
I am a victom
Ill never get over this
I deserve the bad things that happen to me
Nobody is there for me
I am dead inside
What Is the nature of trauma memory (memory paradox)?
Intentional recall is very power
Trouble intentionally recalling complete memory of trauma
Memory is poorly integrated into autobiographical memory base (no clear context in time, place, or other memories)
*Difficulty recalling the trauma because they literally cannot (it's not just that recall is emotional)
Vivid unintentional recall
Involuntary and intrusive memories (flashbacks)
Flashbacks experienced as if in the present
Flashbacks experienced despite more recently learned contradictory info
Flashbacks triggered by wide range of stimuli (fear generalization)
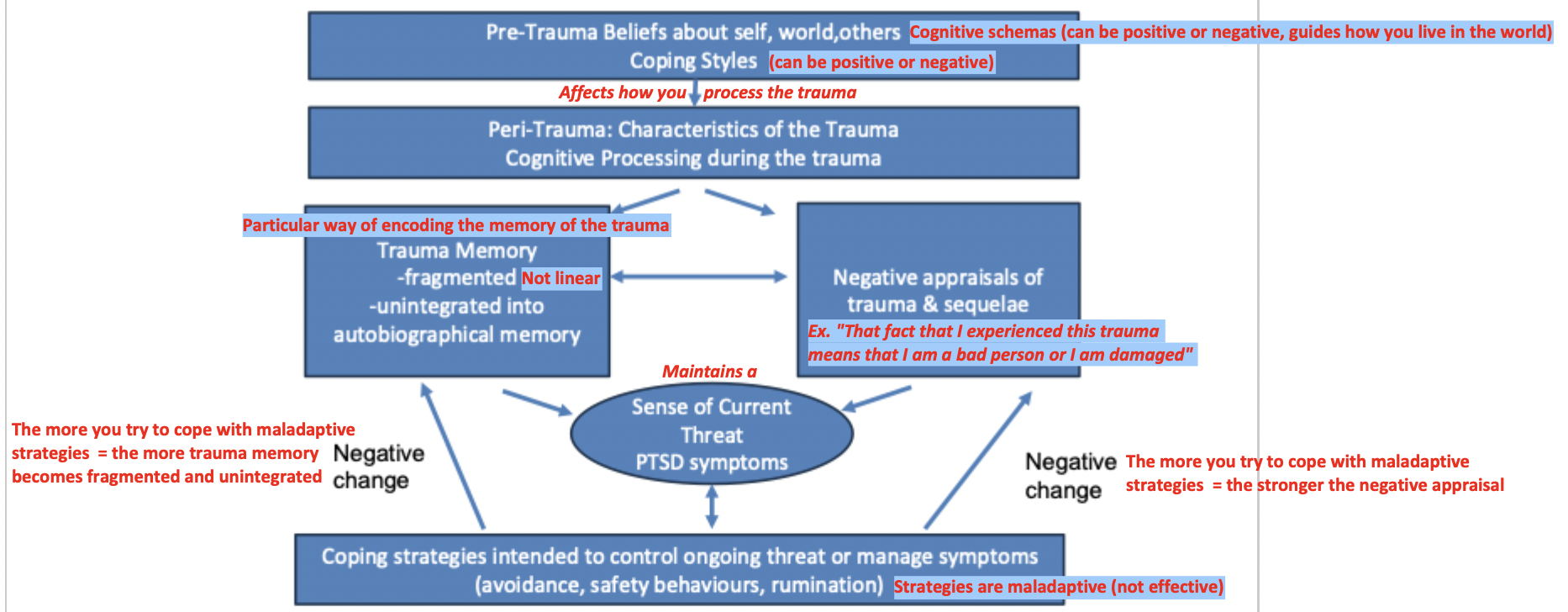
Cognitive behavioural model of PTSD
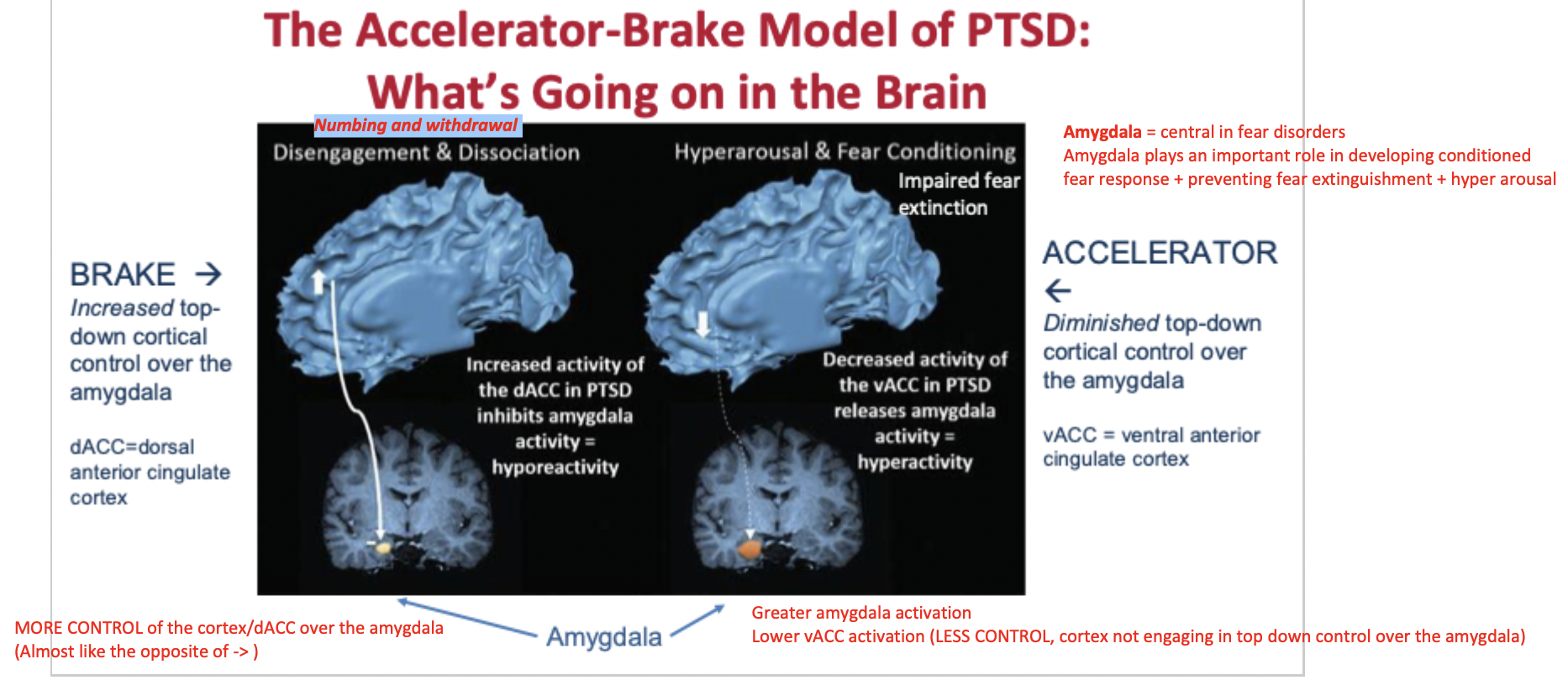
PTSD and the brain (accelerator-brake model)
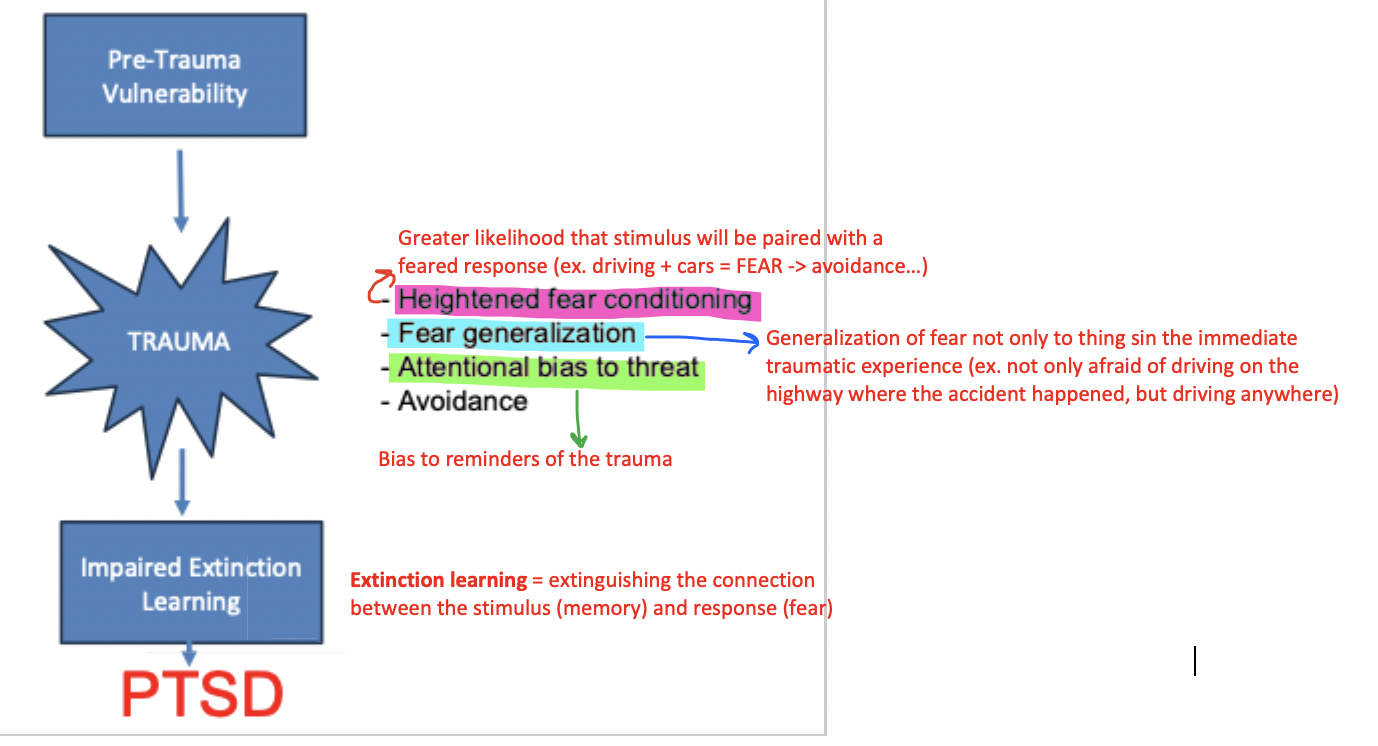
Potentiators of PTSD
Pre-trauma factors:
Family history or genetic vulnerability
Prior worse adjustment/symptoms
Prior trauma
Lower SES
Peri-trauma factors:
Trauma severity
Perceived life threat
Peri-traumatic emotions
Post-trauma factors:
Ongoing life stress or minority stress
What are the two gold standard treatments for PTSD?
Prolonged exposure
Cognitive processing therapy
Prolonged exposure
Exposure to trauma related memories (imaginal exposure) and situations (in-vivo exposure)
Client gets exposed to focus of their fears (AKA the memories of the trauma)
The point is to evoke distress and emotional engagement (because if client continues to run away at the peak, there is the maintenance/generalization of the anxiety)
Goal of the treatment = client repeatedly tells the story of their trauma in great detail
Therapists often record the story so that the client can listen to it back as homework
Therapist asks client their SUDs level throughout the story-telling (empirical approach-- look at their SUDs level each week with the goal of hopefully seeing a gradually decrease)
PE aims to extinguish traumatic response from the memory!
Imaginal exposure (prolonged exposure)
Client repeatedly tells story of trauma in as vivid and detailed a manner as possible
Involves:
Emotional engagement (activates trauma memory)
Habituation to the memory
Cognitive restructuring (NOT trying to restructure people to think that their trauma was a "good thing" that happened … but rather targeting maladaptive cognitive beliefs about themselves ex. "I am a bad person")
Imaginal reliving promotes habituation + reduces anxiety
Telling the trauma story out loud, repeatedly, helps the brain get used to it.
Deliberately confronting memory blocks negative reinforcement connected with fear reduction
Facing the memory on purpose breaks harmful avoidance pattern.
Reliving memory incorporates safety info
Learning that nothing dangerous is going to happen to you as you retell the story / think about the memory: “That happened in the past. I’m safe now.”
Focusing on trauma memory helps client differentiate that memory from other non-traumatic events
PTSD often blurs the trauma memory.
Focusing on the details helps organize the memory and separate it from everyday life.
Prolonged reliving gives opportunities to focus on and modify negative evaluations
Opportunity for client to make restructure their own cognitions ("It's all my fault" -> "It's not my fault that this happened")
Discriminate true danger cues from false alarms and past experiences from the present
Your brain may treat harmless situations today as if they’re dangerous because they remind you of the trauma.
(Someone who was in a car crash may panic at the sound of screeching tires) “That sound is just a sound — not a sign I’m in danger again.”
In vivo exposure (PTSD)
In vivo exposure to situations avoided due to…
Painful memories
Overwhelming anxiety/panic
Guilt/shame
Involves "bad things" that the person is avoiding, typically neutral situations (ex. Driving)
Avoidance interferes with daily functioning
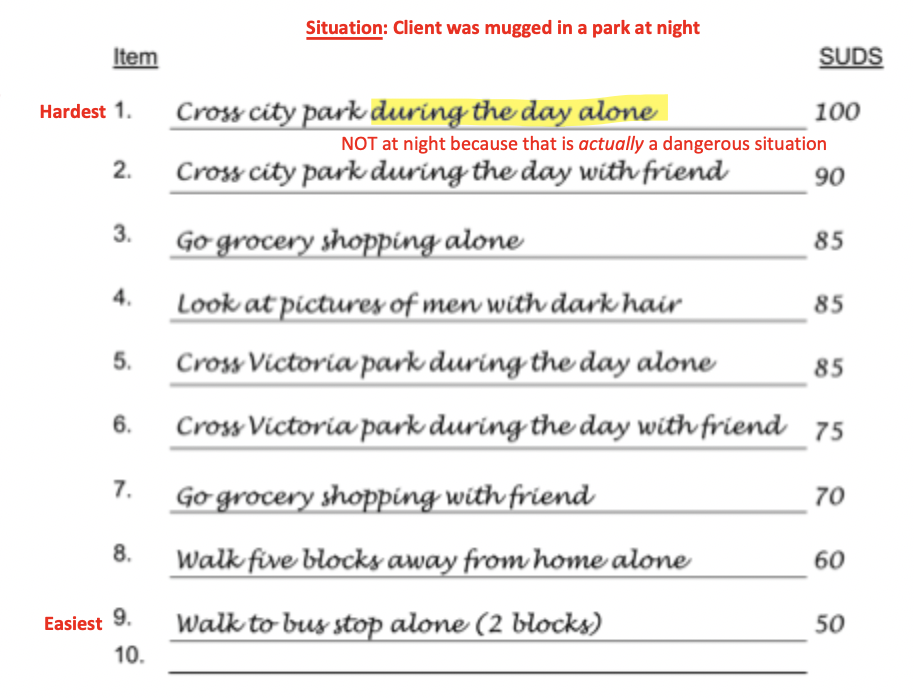
In vivo hierarchy (PTSD)
Cognitive processing therapy
Client writes a narrative account of the trauma and reads it aloud during session
Client uses this written narrative to identify problematic thoughts
CPT helps challenge beliefs through dialogue with therapist + completing worksheets
Examples of maladaptive beliefs challenged by CPT
Negative appraisals
Ex. "This trauma means I am a negative person"
Hindsight bias
Ex. "I should have been able to prevent this if I had just swerved …"
It is easy to see how things could have worked out differently in retrospect
Make the client realize that there was no way they could have prevented it
Self-blame
Ex. "It's all my fault! I should have prevented it"
Just-world violations
People who believe too strongly that the world is a safe place and nothing bad will happen to them = more likely to develop PTSD because trauma memory is a violation of their just-world bias
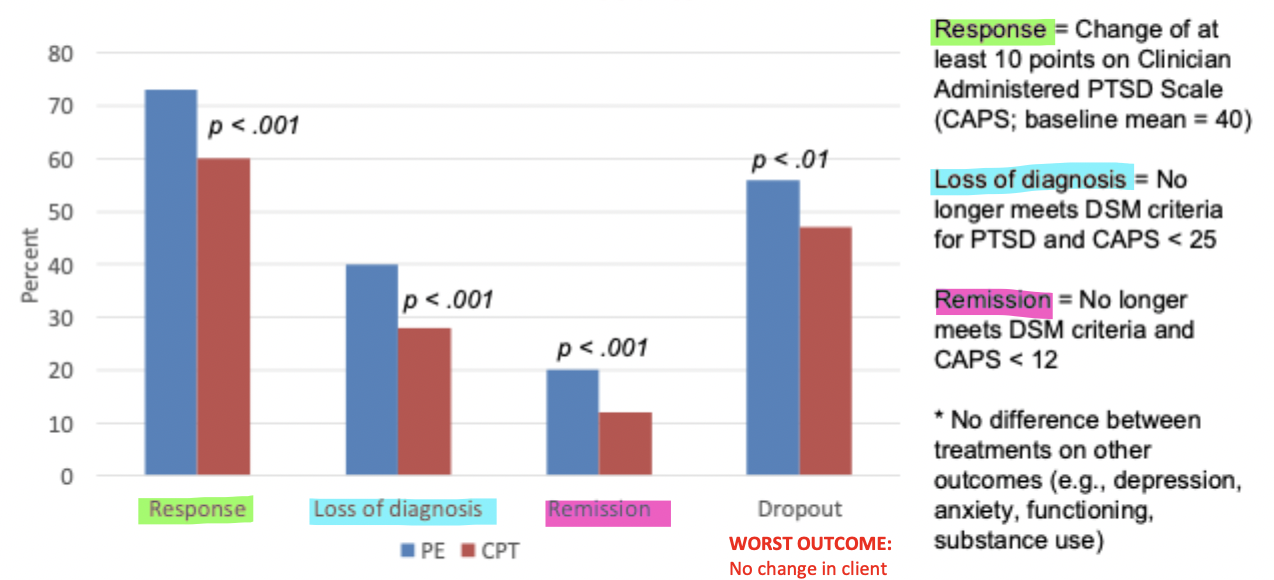
Is prolonged exposure (PE) or cognitive processing therapy (CPT) more effective for PTSD? (veteran study: Schnurr et al., 2022)
Study findings:
More veterans did better with PE
HOWEVER more people also dropped out of the PE treatment, meaning PE was not tolerated as well as CPT…
CONCLUSION:
Either treatment is satisfactory!
Critical incident stress debriefing (CISD)
Group intervention (~3-4 hours) for all victims 24-72 hours following the trauma
Secondary trauma victims = emergency service personnel (often mandated)
Primary trauma victims = accident victims, sexual assault victims, natural disaster survivors, etc. ("normal people" -> trauma did not happen as part of their job)
Educates individuals about stress reactions and ways of coping
Normalizes stress reactions (ex."It's totally normal that you are feeling this way")
Promotes emotional processing and sharing of event (ex. "Let's all talk about our feelings as a group and work through them together")
Provides opportunities for further investigation (What are the next steps / resources for those who may need it?)
Why is the CISD problematic?
Many different studies have found that CISD has no effect on individuals, or even makes them worse off post-intervention (intervention = iatrogenic)
Intervention has very high face validity
Intervention seems like it should work, prevention is a good thing, social support is helpful, etc.
Appearing helpful ≠ Actually being helpful.
BUT this intervention was rolled out way before it was scientifically evaluated… (which is very different from most other treatments, as they often require vigorous testing)
Despite these findings and pushback, the CISD is still mandated in many fields…
This is because it is very hard to something away once you have put it out there and it has face validity
To lay person populations, removing CISD may look like removing support from trauma survivors (even if the evidence says otherwise)
MDMA-assisted psychotherapy for PTSD
*Emerging area in PTSD treatment
MDMA induces seratonin release by binding to presynaptic serotonin transporters
In animals models = MDMA enhances fear extinction, encourages fear memory reconsolidating, and enhances social behaviours
In humans = MDMA reduces amygdala activity to negative stimuli
MDMA may facilitate recall of threatening memories while lessening negative emotions (shame) and hyperarousal -> better processing and consolidation
MDA may support therapeutic alliance because of social bonding
How effective is MDMA treatment? (double-blind, placebo controlled study: Mitchel et al, 2021)
Study details:
Patients received 3 doses of MDMA or placebo in a controlled clinical environment
Patients also received 18-week-long manualized prolonged exposure therapy
Study findings:
People who received MDMA showed SIGNIFICANTLY BETTER SYMPTOM OUTCOMES:
Greater reduction in CAPS (clinician administered PTSD scale) scores
Greater reduction in depression symptoms
Significantly better social functioning
Greater % of individuals in remission stage after 3 sessions of MDMA
What is the cost-effectiveness of MDMA therapy?
Predictions over 30 years:
Healthcare savings = 132.9 million
Premature deaths averted = 61.4
Quality-adjusted life years generated (1 year lived in perfect health) = 4,856
OVERALL:
MDMA gets more people better QUICKER
(no relapse = less treatment= money saved)
MDMA leads to improved health of PTSD population + saves huge amounts of money