chapter 13- cardiovascular blood circulation
1/42
Earn XP
Description and Tags
finish by week of november 15
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
What are the function of the circulatory system?
Transport of oxygen
Removal of waste
Regulation of Body temperature
Immune defense
Fluid redistribution
Example of Transport
delivery of glucose, amino acids, and oxygen (vis RBCs) to cells
Example of Waste removal
CO2 released by lungs; metabolic waste (urea, etc.) removed by kidneys
Example of Temperature regulation
vasodilation & vasoconstriction; e.g. vasodilation in skin vasculature releases heat, while vasoconstriction in vessels supplying the extremities (fingers and toes) retains heat
Example of Immune defense
WBCs, antibodies, histamine in response to infectious pathogens
Example of fluid redistribution
lymphatic drainage recollects excess fluids released into tissues during capillary perfusion
What are the two major circulatory circuits in the body?
Pulmonary circulation (blood flowing to/from the left and right lungs) and systemic circulation (blood flowing to/from the head, neck, and rest of the body’s tissues and organs).
What direction do arteries carry blood?
Away from the heart.
What direction do veins carry blood?
Toward the heart.
What does the red vs. blue coloring in diagrams represent?
Red = high oxygenation; Blue = low oxygenation.
What is the color difference between oxygenated and deoxygenated blood in the body?
Oxygen-rich blood is bright red; deoxygenated blood is darker red or dark crimson.
What is the blood flow pathway through the heart?
the superior and inferior vena cava, right atrium(RA), tricuspid valve(TV), right ventricle(RV), pulmonary semilunar valve(PSLV), pulmonary arteries(PA) to the lungs, pulmonary veins(PV), left atrium(LA), bicuspid valve(BV), left ventricle(LV), aortic semilunar valve(ASLV), aorta(A) and out to the body.
What is systole?
Contraction.
What is diastole?
Relaxation.
First step of cardiac cycle
Late diastole- both sets of chambers are relaxed and ventricles fill passively
Second step of the cardiac cycle
Atrial systole - atrial contraction forces a small amount of additional blood intro ventricles

Third step of the cardiac cycle
Isovolumic ventricular contraction- First phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves.
Fourth step of the cardiac cycle
Ventricular rejectio- as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected
Fifth step of the cardiac cycle
Isovolumic ventricular relaxation - as ventricles relax, pressure in ventricles falls, blood flows back into cusps of semilunar valves and snaps them closed.
What happens at the end of ventricular diastole?
Atria and ventricles are briefly relaxed, and passive filling of ventricles occurs as gravity allows blood to pass from atria to ventricles.
What happens during atrial systole?
Atrial contraction pushes additional blood into the relaxed ventricles.
What is isovolumic ventricular contraction?
Beginning of ventricular systole where blood pushes the AV valves shut (first heart sound “LUB,” S1) and ventricular pressure rises with no blood movement.
What produces the first heart sound (S1, “LUB”)?
Closure of the AV valves during isovolumic ventricular contraction.
What happens during ventricular ejection?
Ventricular pressure exceeds pressure in the aorta and pulmonary arteries, semilunar valves open, and blood is ejected from the ventricles.
What is end systolic volume (ESV)?
The volume of blood remaining in the ventricles after ventricular systole.
Are the AV valves open or closed during ventricular ejection?
Closed.
What happens during isovolumic ventricular relaxation?
Ventricular pressure decreases; blood flows back toward the heart and forces the semilunar valves shut (second heart sound “DUB,” S2).
What produces the second heart sound (S2, “DUB”)?
Closure of the semilunar valves at the start of ventricular diastole.
What is end diastolic volume (EDV)?
The volume of blood in the ventricles at the end of ventricular diastole (start of a new cycle).
Depolarization of the ________ spreads throughout the atria via gap junctions.
SA node
Depolarization of the ________ spreads throughout the atria via gap junctions. The depolarization is transmitted via internodal pathways to the ____________, which delays transmission of the depolarization signal to the ventricles by physically slowing down the opening of ion channels. Atrial depolarization is blocked from spreading to ventricles by the presence of fibrous tissue between the atria and ventricles. From the AV node, the depolarization moves through the ________, and the speed of the depolarizing signal rapidly increases. The AV bundle separates into the left and right__________. These further branch into the ________. In this way, the depolarizing signal that causes ventricular ________ (contraction) is rapidly spread throughout the entire ventricles, but only after the atria have stopped contracting and are in ________(relaxation).
SA node, atrioventricular node (AV node), AV bundle, bundle branches, Purkinje fibers, systole, diastole
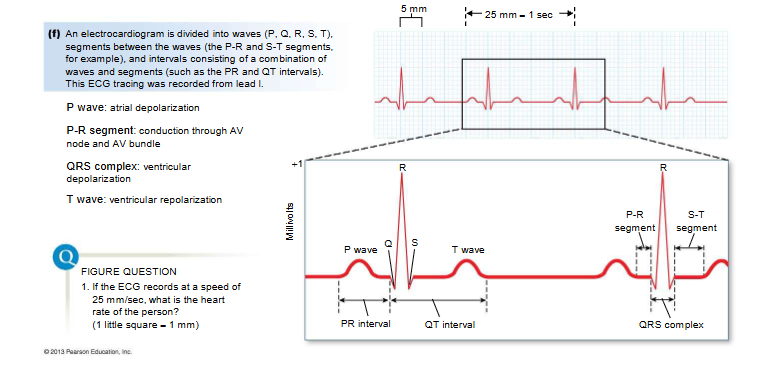
P wave
atria depolarize → atria contract during P-R interval
P-R segment
AV node delay
QRS complex
ventricles depolarize (atria repolarize but hidden)
Start of S-T
AV valves close → LUB → ventricles contract
T wave
ventricles repolarize → relax
End of S-T
semilunar valves close → DUB
Draw and label ECG
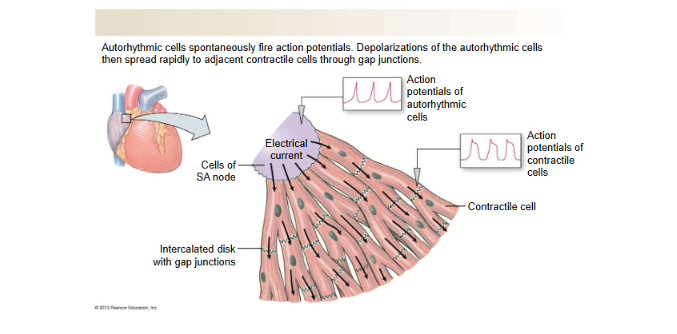
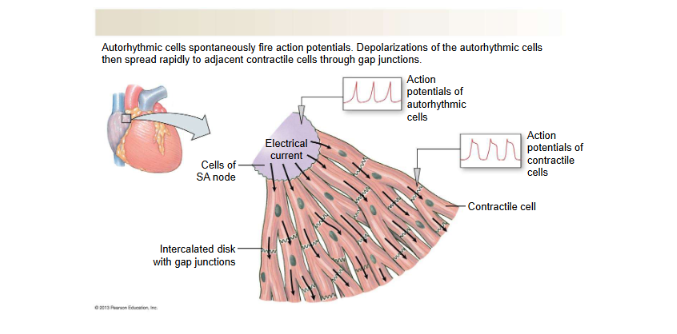
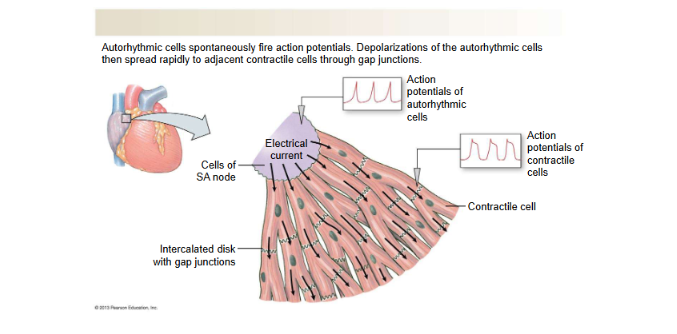
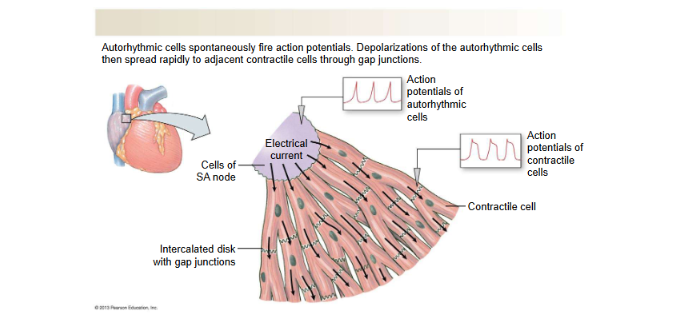
Conducting Cells
Include autorhythmic (pacemaker) cells like those in the SA node.
Generate spontaneous action potentials without nervous system input.
Their depolarization triggers nearly simultaneous atrial contraction (atrial syncytium).
Function: initiate and conduct the electrical signal through the heart.
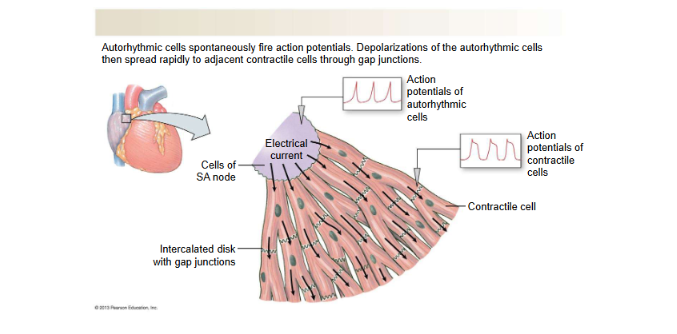
Contractile Cardiac Muscle Cells
Make up most of the myocardium (all non-pacemaker muscle cells).
Connected by gap junctions, so they contract together as a syncytium.
Function: produce force for heart contraction.
Non-Conducting Cells
Fibrous tissue forming the barrier between atria and ventricles.
Electrically insulates the atria from the ventricles.
Function: ensures electrical signals must pass through the AV node, controlling timing.
Pacemaker (Autorhythmic) Cells
Never rest at a stable membrane potential (no true RMP).
Always drifting upward via pacemaker potential.
Use Ca²⁺ influx (not Na⁺) for main depolarization.
Responsible for rhythm generation.
Contractile Cells
Must return to resting membrane potential (RMP) after each beat.
Have a long plateau phase due to Ca²⁺ influx + K⁺ efflux balance.
Plateau prevents tetany → ensures proper pump function.
Responsible for the force of contraction.