Microbiology and Immunology Test 1
1/161
Earn XP
Description and Tags
MDL 107
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
162 Terms

Label 1-5
Eyepiece/Ocular Lens
Diopter Adustment
Arm
Coarse Focus
Fine Focus
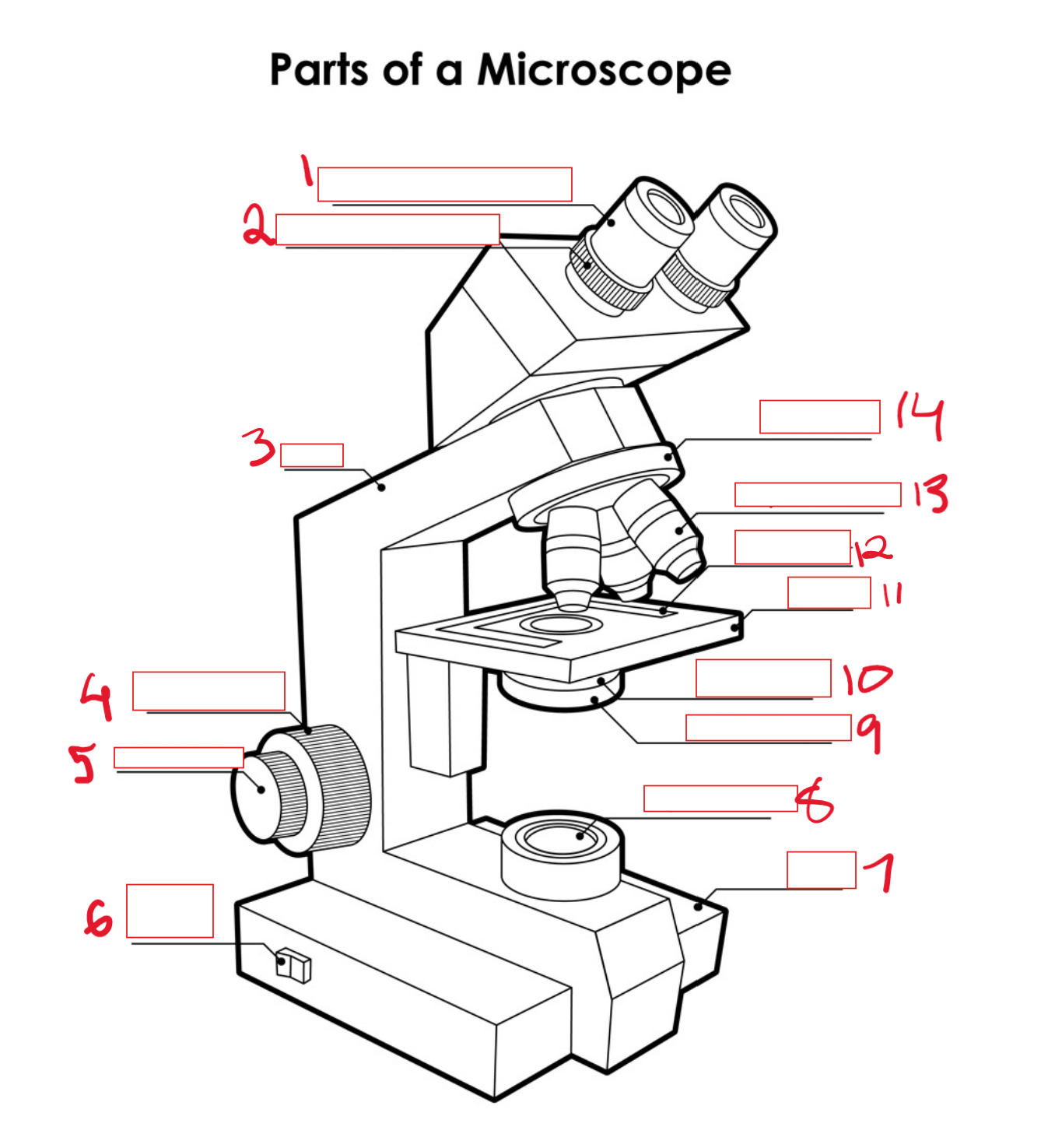
Label 6-10
on/off switch
base
light source/field diaphragm
iris diaphragm
condenser (w flip flop lens)
Label 11-14
Stage
Slide Holder
Objective Lens
Nose piece
Name the granular WBCs and their appearance
Neutrophil - light purple stain, multilobed nucleus
Eosinophil - Pink stain (from eosin stain), double-lobed nucleus
Basophils - dark purple stain, nucleus is obscured
Non-granular WBCs can be further divided into:
lymphocytes
monocytes
White blood cells (leukocytes) can be classified as
Granular (granulocytes)
Non-Granular
name the lymphocytes
B-cells
T-cells
natural killer (NK) cells
Monocytes in the blood become ___ or ___when they enter the tissues
macrophages, dentritic cells
What is the function of a neutrophil?
first cell at site of infection
phagocytosis
digestion done by hydrolase, myeloperoxidase, muramidase
What is the function of an eosinophil?
some phagocytosis (not its primary function)
control of parasitic infestations (releases enzymes extracellularly)
immediate hypersensitivity reactions
releases histaminase to inactivate IgE in allergic responses
What is the function of a basophil?
only in circulation for a few hours then migrate into tissues to become mast cells
some phagocytosis (not its primary function)
releases histamine in response to IgE binding to cell surface receptors
What is the function of a monocyte?
only in circulation for 8-10 hours before becoming macrophages
Antigen presenting cells (dendrites)
secrete proinflammatory cytokines and interleukins
express MHC II, complement, and antibody receptors (used in phagocytosis and antigen presenting cells)
What is the general function of B-lymphocytes?
antibody production in humoral immunity
What is the general function of T-lymphocytes?
regulates proliferation & differentiation of B and T lymphocytes
cell mediated immunity
Neutrophils make up ___% of circulating WBCs
50-70
Eosinophils make up ___% of circulating WBCs
2-5
Basophils make up ___% of circulating WBCs
1
Monocytes make up ___% of circulating WBCs
3-7
B cells mature in the ___ and localize in ___ ___ ___
bone marrow, peripheral lymphoid organs
The cell surface of B cells are lined with
antibodies (membrane bound)
T cells mature in the ___ and localize in the ___ ___ ___.
thymus; peripheral lymphoid organs
What is the function of natural killer cells?
Releases enzymes to lyse virally infected and defective (cancer) cells
natural killer (NK) cells are activated by
interferons
B and T cells can only be differentiated via
flow cytometry
lymphocytes account for ___% of circulating WBCs
20-30
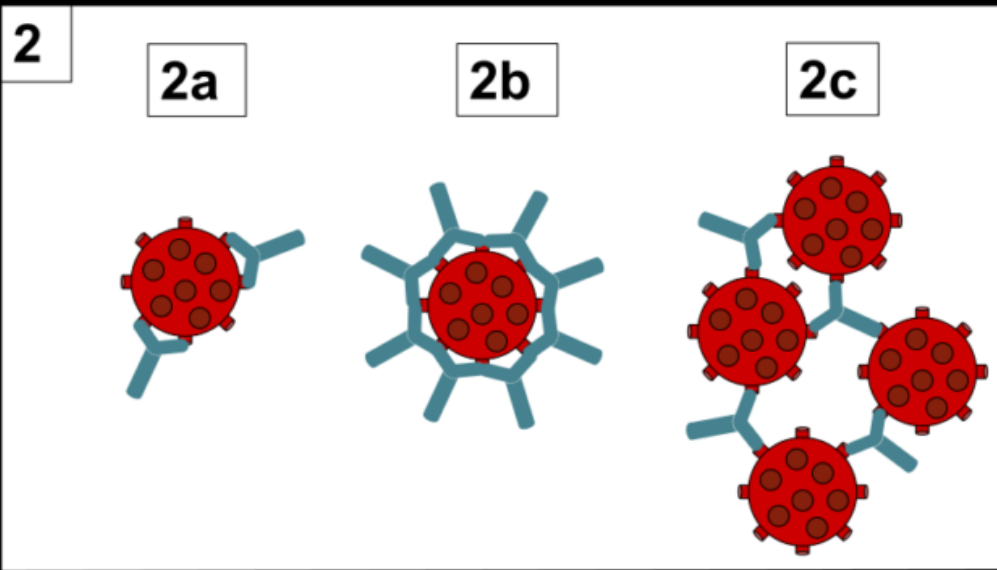
What are the 2 main cell lines for leukocytes?
myeloid - neutrophils, eosinophils, basophils, monocytes/macrophages, red blood cells, platelets
lymphoid - T cells, B cells, NK cells
What is an interferon?
proteins produced by virally infected cells to induce viral resistance in surrounding cells; signal NK cells to destroy virally infected cells
Which factors affect immunity?
age, nutrition, stress
How does age affect immunity?
Young children do not have a completely developed immune system.
Elderly experience decline in immunologically competent lymphocytes
How does malnutrition affect the immune system?
decreased lymphocytes
decreased antibodies
decreased phagocytosis
Why are processed foods bad for immunity?
high fat diets promote action of carcinogens
lack vit. A needed to maintain physical barriers (e.g., skin)
lack vit. C needed for phagocytosis
How does stress affect immunity?
temporarily boosts immune system
longterm → reduces NK cell activity, lymphoid organs atrophy, fewer lymphocytes, phagocytosis reduced
saprophytic microorganisms
grow on dead, decaying matter (e.g., fungi)
symbiotic microorganisms
live with humans in a mutually beneficial relationship (e.g., gut microbiome)
commensal microorganism
depend on their host for support and nourishment
define phagocytosis and which immune cells perform this action
the process of ingesting and digesting foreign material
performed by neutrophils and monocytes
Explain the steps of phagocytosis
phagocytes are attracted via chemotaxis and make contact w foreign material
cellular cytoplasm flows around foreign particle to form pseudopods and engulf it (ingestion) → now a phagosome
oxygen consumption in the cell increases (respiratory burst) to form superoxide radicals (e.g., hypochlorite)
phagosome fuses with lysosomes → phagolysosome
pH of phagolysosome lowers to digest foreign material → now a residual body
wastes in residual body discharged via exocytosis
The immune system can be divided into
innate (natural) immunity
specific (adaptive) immunity
Innate immunity involves:
preventing entry of pathogens through barriers (e.g., skin)
counterattack if barriers breached (phagocytosis)
Specific immunity involves
recognition and disposal of specific pathogens
immunologic memory
amplification/enhancement of innate immunity
What are the differences between innate and specific immunity?
specific immunity discriminates between self and non-self; innate doesn’t
specific immunity is specific to the type of pathogen; innate deals with any foreign material
specific immunity has memory of previous pathogens; innate doesn’t
specific immunity takes days; innate takes minutes to hours
immunology
the study of the body’s response to foreign substances
antigen
a foreign substance that induces an immune response
Define innate immunity
the ability to resist infections by means of normally present body functions
innate immunity is ___ ___ ___ and the ___ ___ of defense
present from birth; first line
What are the 2 parts of innate immunity?
external defense system
internal defense system
What are the 3 components of the external defense system?
physical barriers
chemical barriers
microbiological barriers
Give 3 examples of physical barriers.
Intact skin sheds and prevents microorganisms from attaching to living cells
Mucous prevents microorganisms from attaching to underlying epithelium
Cilia epithelial cells move microorganisms and other particles out of respiratory tract
(others: peristalsis of digestive tract, urine flushing out urethra, sneezing)
Give 3 examples of chemical barriers.
lysozymes in tears and saliva prevent infections.
low pH of stomach acid kills microorganisms
lactic acid on skin keeps pH at 5.6
(others: low pH and lysozymes in urine)
Give 2 examples of microbiological barriers.
Gut microbiome and normal flora on skin use up space and nutrients, leaving little available for infectious microorganisms (crowd out the pathogens).
T or F: stomach acid can destroy microorganisms and toxins
F, stomach acid can’t destroy toxins
What are the 4 components of the internal defense system
WBCs
phagocytosis
complement proteins
acute phase reactants
define chemotaxis
the movement of cells in response to chemical stimuli
define opsonins
a substance which binds to foreign microorganisms making them more susceptible to phagocytosis.
give 3 examples of opsonins
c-reactive protein (CRP)
complement
antibodies
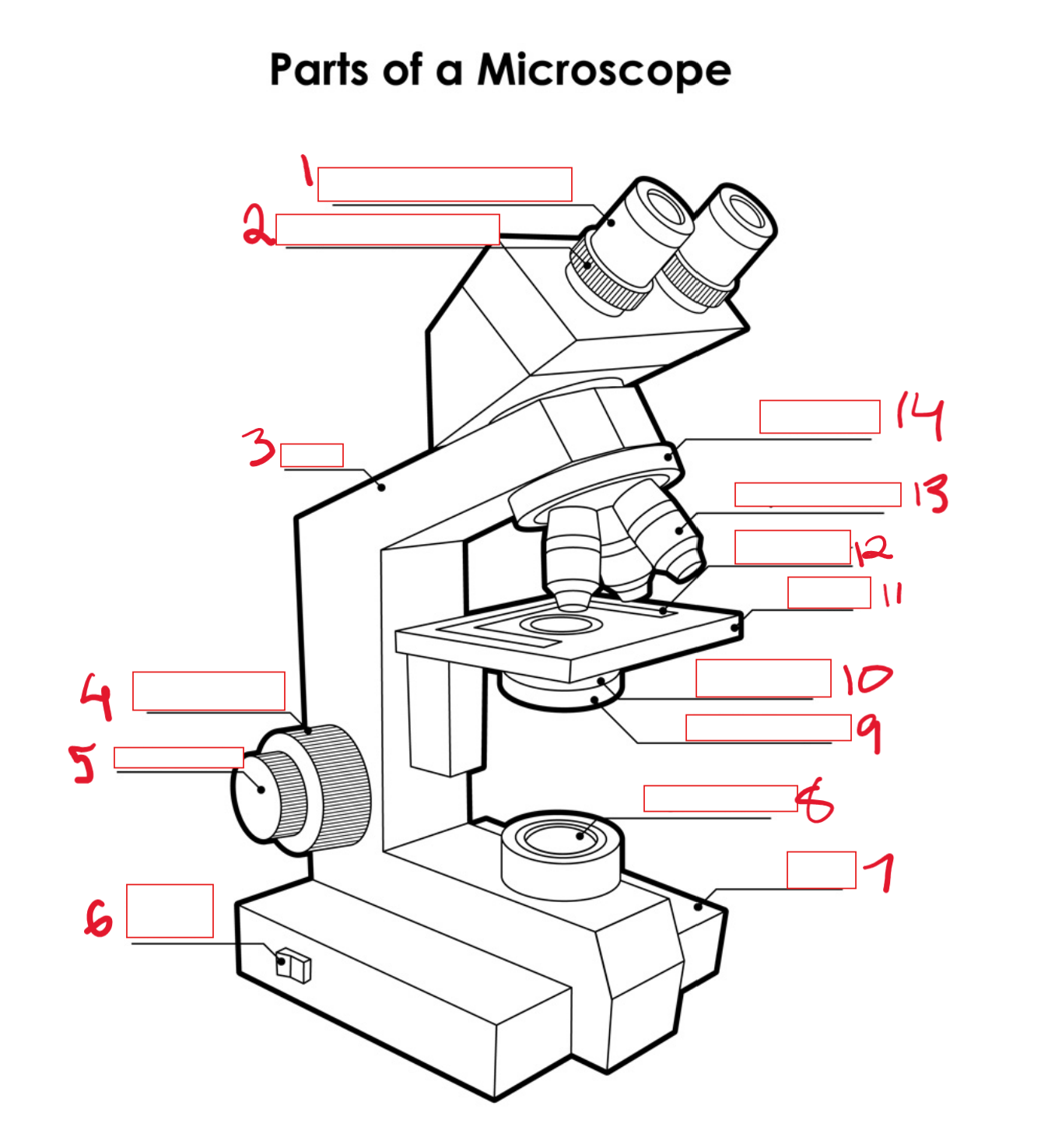
name the processes
a) opsonization
b) neutralization
c) agglutination
phagocytosis can lead to ___ of the phagocyte
apoptosis
what is the function of the complement system?
mediation of inflammation
define acute phase reactants (APRs) and list the 6 examples discussed in class
proteins in the blood that increase in concentration in response to injury/infection
c-reactive protein (CRP)
alpha-1 antitrypsin
haptoglobin
fibrinogen
ceruloplasmin
alpha-1 acid glycoprotein
where are APRs made?
liver
What causes CRP to rise?
bacterial/viral infections
malignancies
myocardial infarction (heart attack)
CRP is an …
early reliable indicator of acute inflammation.
How is CRP clinically useful?
indicates if healing is proceeding normally
rise in levels may indicate infection, organ rejection, or return of malignancy
Explain alpha-1 antitrypsin’s role in maintaining the elasticity of the lungs
WBCs secrete elastase (a protease) to destroy bacteria and infected cells
liver produces α-1 antitrypsin in response
α-1 antitrypsin binds to elastase to prevent degradation of elastin and collagen in lungs
α-1 antitrypsin deficiencies can result in
COPD
emphysema
liver disease
What is the function of haptoglobin?
binds free hemoglobin in blood from intravascular hemolysis
prevents loss of iron by urinary excretion
prevents kidney disease
What is the function of fibrinogen?
forms fibrin clot when skin is cut (prevents spread of microorganisms)
stimulates fibroblast proliferation and growth for healing
What is the function of cerulosplasmin?
transports copper in plasma (blood) to cytochrome C oxidase to meet energy requirements of phagocytosis and wound healing
removes superoxide radicals generated from phagocytosis
what is the function of α-1 acid glycoprotein?
unknown
thought to transport and metabolize progesterone
binds and inactivates some drugs
Define inflammation
the overall reaction of the body to injury or invasion by an infectious agent
Describe the process of inflammation.
mast cells in damaged tissues release histamines, causing vasodilation → causes redness and heat
histamines cause endothelial cells of capillaries to contract, making them “leaky” → fluid leaks into tissues to cause swelling
neutrophils, clotting factors, and APRs, can now pass through leaky capillaries into damaged tissues → phagocytosis of microorganisms, amplification of coagulation system
monocytes migrate to area (now macrophages) a few hours later to clear the area
why is prolonged/chronic inflammation bad?
causes tissue damage and loss of function
If the body’s innate system gets overwhelmed, the body responds with
adaptive immunity
adaptive immunity consists of:
humoral response - production of antibodies (humoral immunity)
cellular response - activation of antigen-specific lymphocytes (cell mediated immunity)
MHC stands for
major histocompatibility complex
cell surface protein
type I on all nucleated cells
type II on macrophages, monocytes, B cells
How do antigen presenting cells (APCs) function?
APCs (e.g., dendrites) recognize pathogens, engulf and digest them (phagocytosis), and display the antigen on MHCII on cell surface
APC travels to lymphatic tissue (this is where the B and T cells are)
presents antigen to T cells until there is a match
Matching T cells are now active, adaptive immunity has been activated
Once activated by dendrites, T cells become
helper T cells - present antigens to B cells to activate them
cytotoxic T cells - destroy infected/defective cells
suppressor T cells - limits/controls immune response
memory T cells - retain the memory of the pathogen
Once activated by helper T cells, B cells become
plasma cells - secrete antibodies
memory b cells - retain the memory of the pathogen
Why are memory B and T cells important?
so an immediate, specific, and enhanced response can be launched in response to subsequent exposures
Describe the function of platelets
involved in clotting mechanism
change shape when activated to form a platelet plug
release cytokines to attract WBCs
Define reticula/reticular tissue
a type of connective tissue composed of reticular fibers (type III collagen) that creates a mesh-like structure to support other tissues and organs
What is the reticuloendothelial system (RES)?
phagocytic cells (primarily monocytes and macrophages) located in reticular connective tissues to filter and trap antigens
I which organs/tissues is the RES found?
spleen
lymph nodes
bone marrow
liver
lungs
What are the primary lymphoid organs?
bone marrow
fetal liver
thymus
What are the secondary lymphoid organs?
spleen
lymph nodes
mucosal associated lymphoid tissue (MALT)
the spleen and lymph nodes are ___ organs
encapsulated
What do secondary lymphoid organs do?
trap antigens
provide network for lymphocyte-antigen interaction (to activate lymphocytes)
what is the role of bone marrow in the immune system?
-blood cell production
-pluripotent hematopoetic stem cells can turn into various blood cells
-B cells maturation
RBCs and WBCs are produced in the ___ bone marrow
red
When is the thymus biggest
at puberty, then begins to shrink
T cell maturation occurs in the ___ and ___ of the thymus
cortex, medulla
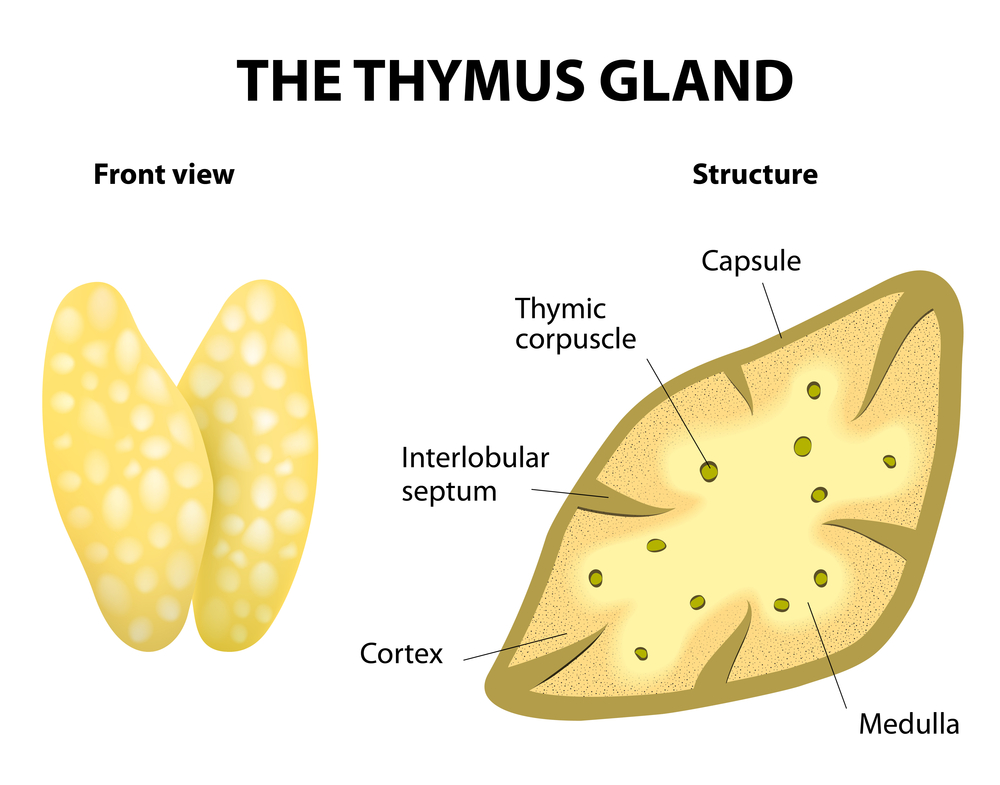
mature T cells are found in the ___ of the thymus
medulla
adaptive immunity begins in the ___ lymphoid organs
secondary
what are the common features of all secondary lymphoid organs?
specialized port of entry
areas where B&T cells migrate
structure maximizes trapping of antigens and lymphocyte-antigen interactions
What do lymph nodes do?
drain and filter fluid from extracellular spaces of tissue
Antigens get trapped in the ___ ___ and phagocytosed by ___. The antigens are then presented to the ___.
lymph nodes, macrophages, lymphocytes
the largest lymphoid organ is the ___ and it ___ ___
spleen, filters blood
The inside of the spleen is split into ___ ___ and ___ ___
red pulp, white pulp
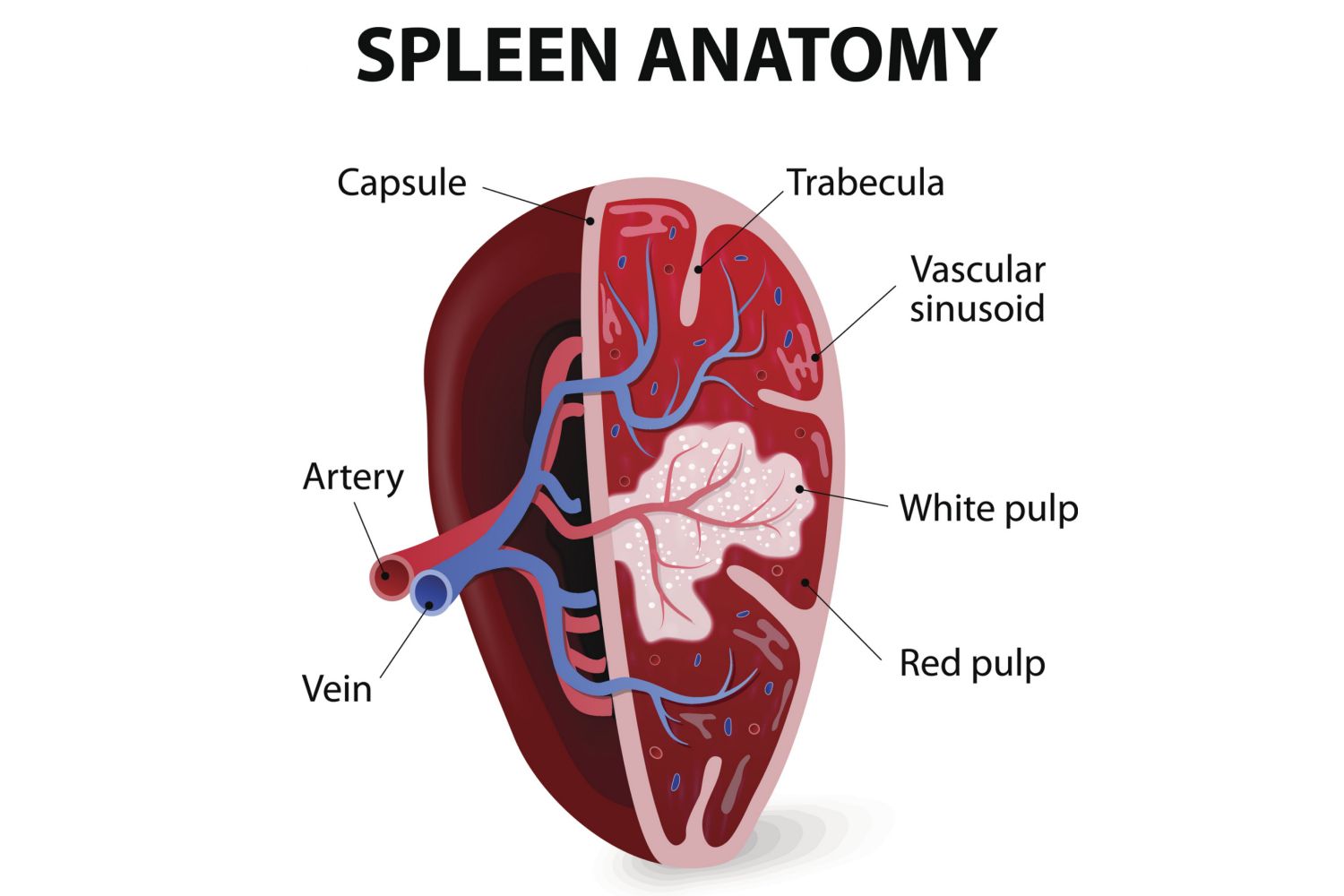
What is the function of the spleen’s red pulp?
destroys old and abnormal RBCs
What is the function of the spleen’s white pulp
provide an area for antigens and antigen presenting cells to activate lymphocytes