Controlling Blood Glucose
1/16
Earn XP
Description and Tags
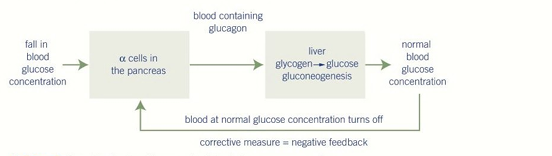
Blood glucose concentration must be carefully regulated to provide a constant supply of glucose for respiration, particularly to the brain which cannot use other substrates effectively. This regulation is a key example of negative feedback and involves the hormones insulin and glucagon, secreted by the islets of Langerhans in the pancreas.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Why is it important to regulate blood glucose concentration?
To ensure a constant supply of glucose for respiration, especially for the brain, which is dependent on glucose as a respiratory substrate.
Which organ and which specific cells detect changes in blood glucose?
The pancreas. Beta (β) cells and Alpha (α) cells in the islets of Langerhans.
How does blood glucose concentration increase?
Diet: eating carbohydrate-rich foods
Glycogenolysis: Glycogen → Glucose conversion
Gluconeogenesis: Glucose production from non-carbohydrate sources
What hormone is released when blood glucose is too high, and which cells release it?
Insulin, released by beta (β) cells.
What hormone is released when blood glucose is too low, and which cells release it?
Glucagon, released by alpha (α) cells.
Describe two ways insulin lowers blood glucose concentration.
(any two)
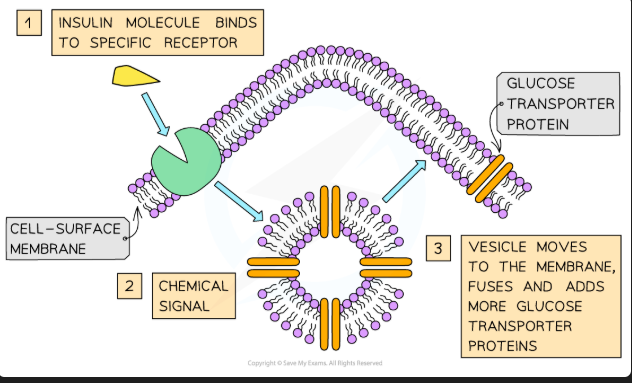
Increases uptake of glucose by cells by stimulating the movement of glucose transporter proteins to the membrane.
Stimulates glycogenesis - the conversion of glucose to glycogen in the liver and muscles.
Increases rate of glucose - fat conversion.
Describe two ways glucagon raises blood glucose concentration.
Stimulates glycogenolysis - the breakdown of glycogen to glucose.
Stimulates gluconeogenesis - the production of glucose from non-carbohydrates (e.g., amino acids).
Reducing amount of glucose absorbed by liver cells
In the second messenger model, what is the first messenger and what is the second messenger?
First Messenger: The hormone (e.g., glucagon).
Second Messenger: cyclic AMP (cAMP).
What are the effects to when insulin binds to its receptors?
Causes a conformational shape change to glucose transport channel proteins
This causes more glucose to enter the cell
When blood glucose rises or falls to a set level, and insulin and glucagon act to restore the blood glucose levels, what is this an example of?
Negative feedback, ensures that changed are reversed and returned to set level.
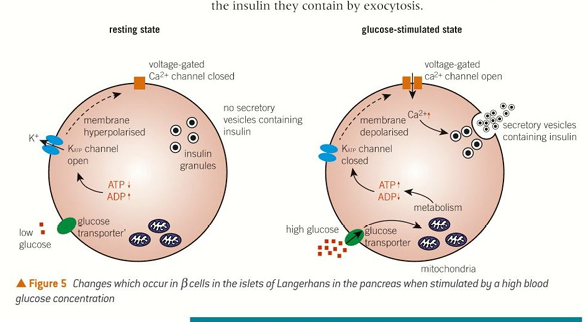
Describe the step-by-step mechanism by which a rise in blood glucose concentration triggers insulin secretion from pancreatic beta (β) cells.
High Glucose: Blood glucose rises → glucose enters the β-cell via a transporter.
ATP Production: Glucose is metabolised in the mitochondria, producing ATP.
Channel Closure: ATP binds to and closes ATP-sensitive K⁺ channels in the membrane.
Depolarisation: With K⁺ efflux blocked, the inside of the cell becomes less negative (from -70mV to ~-30mV), causing depolarisation.
Calcium Influx: Depolarisation opens voltage-gated Ca²⁺ channels.
Exocytosis: Ca²⁺ ions flood in and binds to secretory vesicles, triggering them to fuse with the membrane and release insulin by exocytosis.
Describe how insulin decreases blood glucose. (4 marks)
Insulin binds to specific receptors on target cells (e.g., liver, muscle).
This causes vesicles containing GLUT4 transporter proteins to fuse with the cell membrane.
This increases the permeability of the cell to glucose, so more glucose enters by facilitated diffusion.
Insulin also activates enzymes that convert glucose into the storage polymer glycogen (glycogenesis).
Explain the second messenger model for glucagon. (4 marks)
Explain the second messenger model for glucagon. (4 marks)
Glucagon (1st messenger) binds to a receptor on the hepatocyte membrane.
This activates a G-protein.
The G-protein activates the enzyme adenyl cyclase.
Adenyl cyclase converts ATP to cyclic AMP (cAMP), the second messenger.
cAMP activates a kinase enzyme cascade which ends with the activation of glycogen phosphorylase.
This enzyme catalyses the breakdown of glycogen to glucose (glycogenolysis).
Compare and contrast insulin and glucagon. (4 marks)
Comparison: Both are hormones secreted by the pancreas (by islets of Langerhans) in response to blood glucose levels and are involved in its regulation via negative feedback.
Contrast:
Insulin is secreted by beta cells in response to high blood glucose and lowers it by promoting glycogenesis and cellular uptake.
Glucagon is secreted by alpha cells in response to low blood glucose and raises it by promoting glycogenolysis and gluconeogenesis.
Explain glucose regulation during exercise. (3 marks)
Exercise increases the rate of respiration, lowering blood glucose.
This is detected by alpha cells in the pancreas, which secrete glucagon to stimulate glycogenolysis.
Adrenaline is also released from the adrenal medulla, which further stimulates glycogenolysis in the liver to ensure a rapid supply of glucose for muscle respiration.
Difference between glycogenolysis and gluconeogenesis. (2 marks)
Glycogenolysis is the breakdown of the stored carbohydrate glycogen into glucose.
Gluconeogenesis is the synthesis of new glucose from non-carbohydrate precursors (e.g., amino acids, glycerol).