Patho Final - Old Content
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
Differentiate atrophy, hypertrophy, hyperplasia, metaplasia, and dysplasia.
Size or number
Atrophy = size decrease
Due to decreased demand or supply
Hypertrophy: increase in cell size
Increased demand
Skeletal and cardiac
Hyperplasia: increase cell number
Increased demand
Skin, intestinal, gland, hepatic, reproductive (BPH)
Cell Type
Metaplasia: From one normal cell to another
Chronic irritation/inflammation
New cell type is TOUGHER and better to survive in harsh condition
“Barrett’s esophagus”
Reversible
Dysplasia: cells are MESSED UP
Chronic irritation or inflammation
New cell types are abnormal an do NOT function very well
Different than anaplasia (which is cancerous)
Using examples, interpret ABGs using the terms, metabolic acidosis, metabolic alkalosis, respiratory acidosis, and respiratory alkalosis and compensatory mechanisms
Metabolic Acidosis: Blood pH less 7.35
Too little BASE (HCO3) - ABG: Low HCO3/bicarbonate
GI loss of HCO3
TOO MUCH ACID
Renal failure
Ketoacidosis
Manifestations
Compensation: Kussmauls breathing - blow off CO2: LOW CO2
Disorient
Coma
Dysrhythmia
Metabolic Alkalosis
ABG: HCO3 TOO HIGH
Loss gastric acids, bicarbonate ingestion, etc.
PH over 7.35
Manifest: Cardiac dysruthmia
Comp: Lungs attempt retain CO2 slowing RR, Kidney retain H+
ABG: High CO2
Respiratory Acidosis:
CO2 TOO HIGH
Compensation: Kidney attempt reabsorb HCO3, Excrete H+
HCO3 ELEVATED, H+ LOW
Respiratory alkalosis
BASIC
CO2 LOW
Comp: Kidney try reabsorb H+ and excrete HCO3
HCO3 LOW, H+ HIGH
Know how to solve problems look at exmapls// picture

Understand how transcellular shift regulates potassium ion and hydrogen ion concentration
Potassium helps maintain intracellular osmolarity
Controls cell resting potential
Potassium-hydrogen transcellular shift (K+/H+)
Potassium exchanged for H+ to buffer changes in blood pH
Acidosis
Reg intracellular potassium, high H+ inside bloodstream
Potassium from inside cells pulled into bloodstream, low potassium intracellular
Alkalosis:
Reg intracellular potassium, low H+ inside bloodstream
Potassium moves from bloodstream into cells = high intracellular potassium
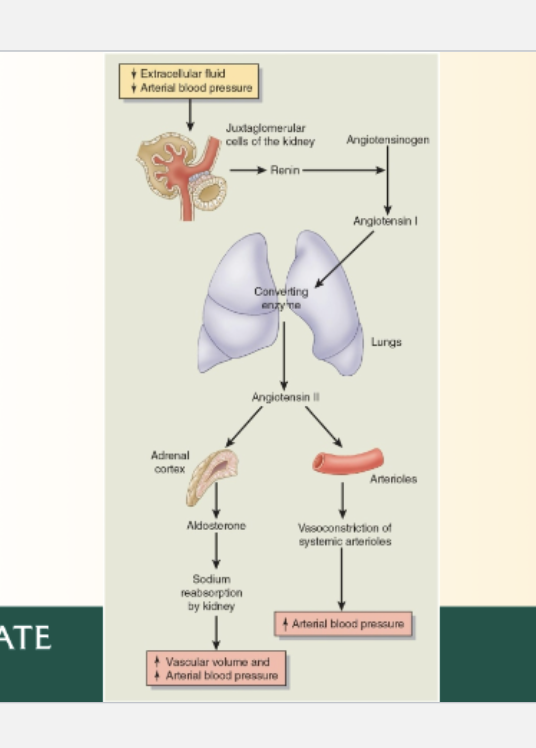
Describe how osmoreceptors and renin-angiotensin-aldosterone system (RAAS) maintain fluid balance.
Look at picture and STUDY
State the five cardinal signs of acute inflammation and describe the physiologic mechanisms involved in the production of these signs.
ALL THESE DUE TO THE VASCULAR STAGE (Local response)
Local response is nonspecific, protective, coordinated
Inflammatory mediators released at area
Redness
Vasodilation to area causes redness, more blood
Vasodilation caused by inflammatory mediators (histamine and bradykinin) which enable blood vessels to dilate and become permeable
Swelling
Vasodilation of arterioles is followed by enhanced capillary permeability
Fluid flows OUT of blood vessels into injured tissues = swelling
Heat
Heat due to Increase blood
Pain
Loss of Function
Pain and loss of function caused by
Chemical mediators, histamine, bradykinin, prostaglandin cause nerve endings to be senstiive
Swelling causes pressure on nerve endings
LOF
Pain and swelling limit/ restrict movement
Tissue damage or disruption can also
PAIN and LOF can come from chemical stage as well as vascular stage
Chemical as a result of chemical mediators which can cause pain and disrupt tissues
Describe the processes of transcription and translation and identify the ultimate product
Transcription:
Process of making RNA copy of DNA
Occurs in nucleus
Intiation RNA poly binds
Elongation
Termination
PRODUCT = mRNA (carry genetic code out of nucleus to ribosome)
Translation
Happens at ribosome
mRNA provides code
tRNA provides amino acid
Ribosome forms peptide bonds
Intiation
Elongation
Termination
PRODUCT = POLYPEPTIDE (protein)
Describe the etiology, pathophysiology and manifestations of atherosclerosis
Causes/Etiology
Hypertension
Hypercholesterolemia
Smoking
Uncontrolled diabetes melitius
WHY? They all cause damage to endothelial tissue aka blood vessel tissue
Steps:
Epithelial damge causes migration of WBCs (leukocytes) and platlets
These adhere to the endothelial tissue
Endothelial tissue becomes permeable
Macrophages are adhere to endothelial tissue (they were leukocytes, macrophages ARE specific type of leukocytes)
Start to engulf LDL
Foam cell formation
Macrophages migrate inside epithelial tissue and become foam cells (foam cells = lipid loaded macrophages, LIPIS = LDLs)
Smooth muscle begins to migrate upward to make a FIBROUS CAP
Underneath lies machrophages, foam cells, necrotic core, lymphocytes collagen
Adherence and entry of leukocytes
Adherence and aggregation of platlets
This is a atherosclerotic plaque now, causes FATTY STREAKS
If ruptures, causes major clotting to occur and
If NOT just ISCHEMIA
Manifestations
Most common in:
Abdominal aorta + iliac
Coronary
Femoral, popliteal
Internal carotid
Verebral, basillar
Manifestations of
Stable angina
Dyspnea
Fatigue
If rutpure:
Mycardial infarciton
Unstabel angina
Cardiac death
Stroke
Define peripheral arterial diseases and explain S/Sx (including claudication, oxygen
demand/supply).
PAD also known as Peripheral arterial occlusive disease
Atherosclerotic plaque obstructs blood flow to a LOWER extremity (peripheral)
Risk factors:
Age, HTN, DM, SMoking
High fat diet, sedentary
Family history
Flow chart:
Occlusion of arterial blood flow
Reduction in blood flow
Oxygen supply LOWER THAN Demand
Ischemia, aerobic metabolism
Pain (intermittent claudication - bc its in legs)
Pallor
Weak pulse
paresthesia - numbness tingling in lower extremities DUH
Describe hallmarks of stable angina
Chest pain
Occurs when there is INCREASED myocardial oxygen demand (physical work, emotianl stress
Relieved by:
Rest DUH
NItroglycerin
From a FIXED ATHEROSCLEROTIC PLAQUE causing ischemia
Very common - intial presentaiton for MANY people with coronary artery disease
So hallmarks = chest pain or pain, relieved by rest or nitro and caused by something
Unstable is PAIN AT REST, and rest does not help duh
Explain how heart failure changes the following hemodynamic measurements: CVP, CO, pulmonary capillary pressure, and BP
Systolic Heart failure: Heart does not PUMP ENOUGH OUT (due to weak ventricle)
Diastolic: NOT ENOUGH BLOOD IN (due to stiff ventricle)
Dec CO
Dec SV
Decreaes BP as well, BP = CO x PVR
Also INCREASE pulmonary capillary pressure
Not enough out means BACKUP somewhere
Backward effect
backup of blood into atriums and pulmonary vessels
LVF = pulmonary edema = cough, orthopnea, noctural sypnea
RVF - lower extremity edema
Forward effect
Not enough out = dec BP
Dec BP = RAAS< ADH, SNS
Increase fluid retetnion = weight gain
Differentiate the three main categories and mechanisms of anemia (blood loss, hemolytic and impaired RBC production
Blood loss
Acute vs Chronic
Acute = rapid blood loss from trauma, childbrith, vessel rupture, etc.
Labs = Normochromic Normocytic (BC its SUDDEN)
Chronic
Slow blood loss = GI Bleed or something
Leads to LOW IRON = iron deficiency anemia
Microcytic Hypochromic
Hemolytic/ SICKLE CELL
Autosomal recessive disease
Mutation causes sickle cell anemia RBCS
Upon exposure to hypoxia or stress, RBC contorts into a sickle shaped
= Cant pass through capillaries = hypoxia due to obstruction
ALSO leads to excessive RBC breakdown = jaundice
NORMOCYTIC NORMOCHORMIC (why?)
Impaired RBC production
Decreased production of RBCs by bone marrow
Essential nutrients
Iron: hemoglobin synthesis
Vitamin B12 and folic acid: for DNA and maturation
ANY Deficiency leads to decrease production leads to anemia
MICROCYTIC HYPOCHORMIC
Why- small due to lacking materials like hemoglobin
Hypochromic due to lacking hemoglobin
HEMOGLOBIN REQUIRES IRON
Describe how leukemias create each of these manifestations: anemia, thrombocytopenia, leukocytosis, neutropenia, bone pain, increased risk for infeciton
Leukemia general: Leukemia = a cancer of the blood forming tissues aka cancer of the bone marrow
Cancer of the bone marrow leads to overproduciton of abnormal white blood cells which CROWD OUT normal, healthy blood cells
Anemia
Overproduction of abnormal/ immature white blood cells overcrowd the bone marrow and decrease RBC production/ growth
Thrombocytopenia
Overproduction of abnormal/ immature white blood cells overcrowd the bone marrow and decrease RBC production/ growth
Leukocytosis
Stem cell precursuros for T and B lymphocytes in bone marrow do NOT function and mature, leading to low WBC
Abnromal leukocytes = NOT DEVELOPED FULLY or NONFUCNTIONAL or UNCONTROLLED PROLIFERAITON
Neutropenia
Bone marrow overcrowding
Fialure of normal cell formation, blasts stuck in early stages
Suppression by cytokines
Bone pain
Due to overcrowding
Increased infection risk
As a result of low WBC, neutrophils, etc. immune function is worsened
Create a table that compares and contrasts emphysema and chronic bronchitis in terms of most common cause- pathology and clinical manifestations.
Describe how COPD causes pulmonary hypertension (include hypoxic vasoconstriction in your explanation)
Chronic bronchitis - blue bloater
CANT GET IN
Mucus and edema inhibit ventalation = cough
Chronic hypoxia + cyanosis
Clubbing
Chronic hypxoia = pulmonary arterial vasoconstriciton
Leads to RVF = JVD, ascited, ankle edema (BLOATER) hepatosplenamoagoly
Chornic hypoxia leads to RIGHT SIDE HERAT FAILURE
Emphysema - PINK PUFFER
CANT GET OUT
Destruction of elastin = non recoil alveoli = CO2 retetnion
Chronic hypercapnia
Prolonged exhalation/ pursed lip
BARREL CHEST, cant get out duh
Diapghram pushed downard due to excess air
Explain changes in pulmonary function test (e.g., FVC, FEV1) in restrictive pulmonary diseases and explain what FVC and FEV1 are
FVC = forced vital capacity
Total volume of air a person can FORECFULLY EXHALE after a full inhalation
Reflects LUNG VOLUME
FEV1 = Forced expiratory volume 1 second
Volume of air exhaled in first second of FVC
Reflects airflow/ how QUICK air gets out
Restrictive disease = REDUCED LUNG EXPANSION = total volume shrink
Pulmonary fibrosis
Decreased FVC
If lungs CANT expand then there is less air to exhale and inhale
FEV1 decrease
If total lung volume smaller, amount exhaled is smaller
FEV1 decreases propritonall to FVC
BC FEV1 is APART of FVC
FEV1/FEC ration
If FEV1/FEC ratio over 0.9 its NO GOOD (aka closer to 1) THINK WHy
If its closer to one, that mean the amount dropped vs total amount out is very similar BECAUSE there is less to get out and its harder to get it out
After 1 sec its almost already all out
Describe the alterations in cardiovascular function that are characteristic of cor pulmonale.
Cor pulmonale = RIGHT SIDE HEART FIALURE
Cardiac alterations
Right ventricular hypertrophy due to HIGH AFTERLOAD from pulmonary hypertension
Rifht ventricular dilation THIS MORE IMRPOTANT (after time
REDUCED CO
Systemic venous congestion DUH
Signs and symptoms
Chronic hypoxia
Leads to a VQ mismatch
Leads to pulmonary vasoconstriction
Pulmonary hypertension
RVH, RVF (increased workload)
JVD, ascites, ankle edema
Describe the relationship between hypertension and the kidney dysfunction
Hypertension and kidney dysfunctino is BIDIRECTIONal
If one gets wrose, the other gets worse
AND VICE VERSA
HTN caused by atherosclerosis or whatever
Kidney disufnciton by dec GFR and urine output
WHY, decreased urine = increase fluid = more hypertension
More hypertention is wrose for kidney function, dec perfusion wahtever
Describe the three categories representing the causes of kidney dysfunction based on the mechanism of injury (prerenal, intrarenal, postrenal) and list examples of each dysfunction.
Prerenal
Issue BEFORE kidney = REDUCTION OF RENAL BLOOD FLOW
Kidney not getting enough
Dec perfusion = dec GFR
RAAS activates = water + sodium retention
Concentrated urine
Examples:
Shock
Dehydration
Vasoconstriction
HTN
Intrarenal
Problem WITHIN kidney itself = damage of tubules, glomeruli, interstria or vasculature
Kidney tissue is injured
Structural damage = impaired filtration, secretion, reabsorption
Acute Tubular Necrosis:
MOST COMMON
Ischemia, toxin, inflammation leads to sloughing of tubular endothelial cells which Block fluid flow through nephron
Acute interstitial nephritis
Postrenal
Urine flow blocked = obstruction of
pressure backs up = hydronephrosis = decreased GFR
Example:
Stones, tumors, enlarged prostate (BPH)
Understand the pathophysiology and clinical presentation of chronic kidney disease
Irreversible, progressive process with a GRADUAL onset
CRF will progres to end stage renal failure
Etiology;
Hypertension, Diabetes melitus, chornic glomerulonephritis
Patho
Kidney damge leads to increasingly worse GFR
As neprhons fail, renal fialure issues set in
EPO
Vitamin D
Acid/base
Renin functions lost
Signs and symtpoms
NO concentrated urine
Hyperphosphatemia - bone loss
Hypocalcemia - increase PTH
No EPO = anemia
Hyperkalmeia = acidosis
Metabolic acidosis
Fluid overload =
Edema
HTN
HF
Pulm edema
Neural
Ecephalopathy (cant filter)
Confusion, stupor
Thrombocytopenia
Anemia
Create a table that contrasts upper and lower motor neuron disorders (UMN and LMN) in terms of location of dysfunction and manifestations.
UMN
Pathology in the CNS
Above brainstem = affects opposite side
Below brainstem = affect SAME side
Spastic/hypertonic paralysis
Hyperreflexia
(bc its affecting the root, think like disease affecting the generation = rapid fire)
LMN
pathology in PNS
Affects SAME SIDE ALWAYS (bc the source of the problem is motor nerves that exit the spinal cord)
There is NEVER any crossover, lower left issue results in lower left issue
Flaccid/weakness paralysis
Hyporeflexia/ decreased reflexes
Briefly explain the mechanisms of ischemic stroke and state common causes
Ischemic stroke = blocked blood flow to brain tissue
Tissue becomes ischemica = cerebral infarciton
Common causes
Anyting that increases risk for developing atheroslcerosis = increased risk for ischemic stroke
It is cerebral atherosclerosis
Carotid stenosis
Atrial fibrialtion
Ischemic penumbra = perimeter around CORE ischemic area
Rapid reperfusion of htis area is critical as it will also suffer infarciton soon after
HOWEVER, reprofusion causes free radicals to carry in blood stream (free radicals develop after cellular damage
Understand the mechanisms and S/Sx of Cushing’s triad
Physiological response to elevated intracranial pressure
happens due to cerebral edema or anything else, bc skull CANT change shape/ give way
brain tissue damage = inflammation = edema in skull = increase ICP = cushing triad
Parts:
Hypertension
Bradycardia
Irregular respirations
Increaed ICP = reduced cerebral perfusion
Reduced cerebral perfusion leads to sympathetic activation
Leads to vasoconstriciton + hypertension (to help push blood into brain)
Leads to high pulse (widened pulse)
Rise in BP = baroreceptor reflex = bradycardia
Bradycardia to compensate for high blood pressure
Brainstem compression
Compression of pons and medulla leads to IRREGULAR RESPIRATIONS
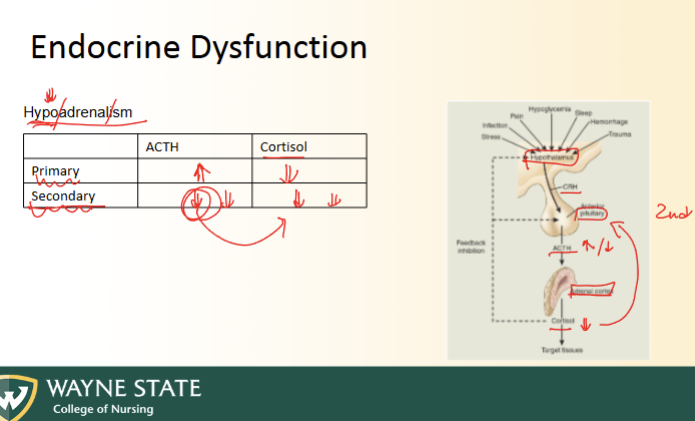
Using the hypothalamic-pituitary-endocrine gland axis feedback mechanism, differentiate primary endocrine disorders from secondary endocrine disorders
Hypothalamic-Pituitary-Hormonal axis
Hypothalamic portion of brain secretes RELEASING FACTOR (stimulates pituitary)
Pituarity secretes TROPIC/STIMULATING hormone (stimulates endocrine organ)
Endocrine organ secretes SPECIFIC HORMONE (to act on body)
Primary = abnormality in peripheral gland
Secondary = abnormality in pituitary
Tertirary = abrnoamlity in hypothalamus
THINK NEGATIVE FEEDBACK LOOP
Look picture- SUPER EASY
Identify common signs/symptoms of Cushing’s Syndrome
Cushing’s Syndrome = HYPERADRENALISM
Due to hyperactive adrenal gland which secretes too much cortisol
Causes:
Endogenous cushings - tumor on adrenal gland or hyperplasia
Ectopic cushings - tumor release ACTH
Exogenous - long term or overuse of glucocorticoid
S/sx:
Glucocorticoid excess
Hyperglycemic
Fat redistribution (buffalo hump and moon face, and large abdomen (increase waist to hip)
Thin skin + striae
Osteopororsis - due to increase bone resorption
Increase gluconeogensis = hyperglycemic DUH LOOK HERE
Decreased inflammation + immune response = more infection
Mood:
Irritible
Cognitive impariment
Fatigue (long term stress hormone = exhaustion)
Fluid, electorylte imbalance - Aldosterone/mineralcorticoid
Increase NA upkeep
Increase fluid
Increase BP
More acidic???
Androgens - Sex hormone
Females get hirsutism and menstrual irregularities
Recognize the chronic complications of diabetes including autonomic neuropathy, peripheral nephropathies, retinopathies, macrovascular complications, poor wound healing, foot ulcers, and infection
Micro: AKA HYPERGLYCEMIC DAMAGE (affects smallest arterial blood vessels first) — RNN
Retinopathies (damage of eye)
Blindless
Cataracts
Glaucoma
Neuropathies (affects neurons (arterial vessels of neurons = small)
Sensory - pain sensation is blunted)
Nephropathy - very small
LEADING cause of chronic renal failure
Macro:
Peripheral vascular disease
Coronary heart diease
Cerebrovascular disease
Stroke or TIA
Causes damage to larger epithelial tissue
Mos