Ch. 20
1/26
Earn XP
Description and Tags
Urinary System
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
Identify the following structures
o Kidney
o Ureter right/left
o Renal medulla
o Renal cortex
o Renal pyramid
o Renal pelvis
o Glomerulus
o Capsular space
o Fibrous capsule = renal capsule
o Urethra
o Right/left renal veins
o Urinary bladder
Organs of urinary system
2 Kidneys
Contain nephrons that are responsible for removing waste producrs, stray ions, & excess water from the blood
*Nephron producces urine by filtration, absorption, & secretion
Structure of Renal pelvis & the calyces
Funnel-shaped sac that connects directly into the ureter, along w/many tubes that converge to form the funnel-shaped sac
2 Ureters
The ureters are bilateral, muscular, tublar, structures, each one responsible for taking urine from one kidney to the urinary bladder for storage, prior to excretion
Urine flows from renal calyces down ureters into bladder for storage
Bladder
Stores urine, allowing urination to be infrequent & controlled
The normal capacity of the bladder is 400-600 mL
Urethra
The tube that conveys urine outside the body
Kidneys
Locate retroeritoneally-outside of/behind the peritoneum
The kidneys aren’t located in the peritoneal cavity, but outside of it
Recall that the peritoneum is the double-layed serous membrane of the abdominal cavity
Function of Kidneys
Primary function of the kidneys
To regulate the volume & composition & pH of body fluids
In the process, the kidneys remove metabolic wastes & excess chemicals as well as excess water 7 electrolytes from the blood &, along w/the ureters, urinary bladder, & urethra, excrete them to the outside as urine
Electrolytes
Molecules that release ions in water
Role in water balance
Intracellular fluids
High concentration of potassium K+
These wastes include nitrogenous & sulfur-containing products of protein metabolism, such as certain metabolic acids
*The kidneys convert vitamin D from supplements or the sun to the active form of vitamin D that is needed by the body
Kidneys Pt. 2
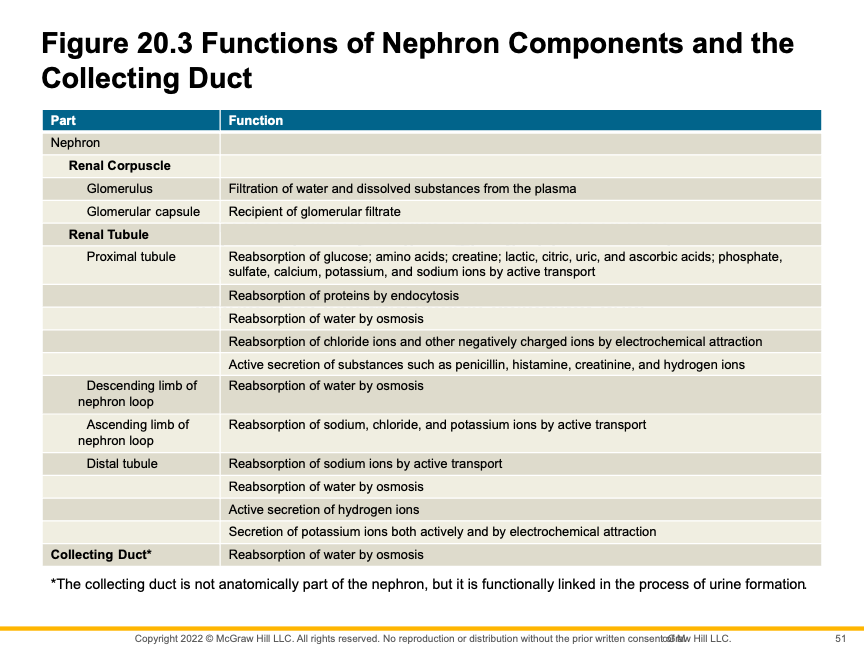
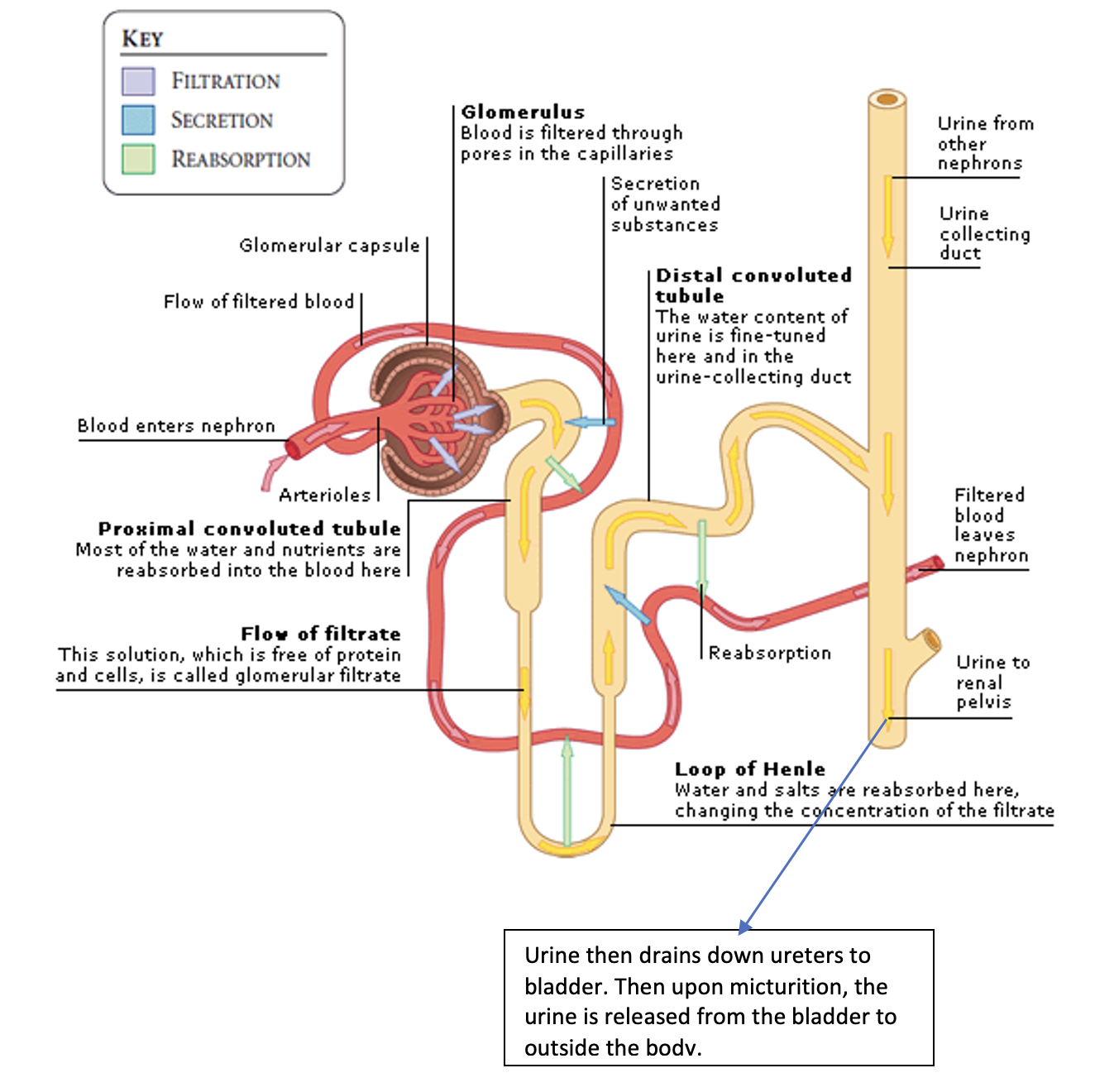
The formation of urine the nephron involves 3 processes:
Glomerular filtration- filtration that begins at renal corpuscle (Glomerulus)
The stage of urine formation that involves the production of filtrate w/the same composition as tissue fluid & plasma, while large molecules such as proteins & blood cells remain in the blood
High blood pressure would increase the rate of glomerular filtration
Tubular Reabsorption
Occurs as substances pass from the renal tubules to the peritubular capillaries
Returns usefule substances back into the blood
Water reabsorption from the proximal tubule is closely linked to the active reabsorption of Sodium (Na) ions
Tubular Secretion
Secretion occurs when substances pass from the peritubular capillaries (blood) into the renal tubules
Secretion of hydrogen ions (H+) is important for regulating the pH of body fluids
Kidneys function in the homeostatic regulation of pH of body fluids
Kidneys adjust excretion & absorption of hydrogens ions & bicarbonate as needed
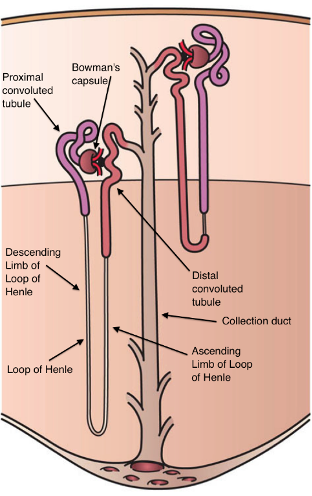
Trace the pathway of urine from the nephron to body’s exterior
The nephron is the functional unit within the kidney. The nephron has several segments, each w/more specialized functions
Glomerular capscule → proximal convoluted tubule → Nephron loop (ascending/descending Loop of Henle) → Distal convoluted tubule → Collecting duct
Sequence through tubules:
Proximal tubule, descending limb of nephron loop, ascending limb of nephron loop, distal tubule
What parts make up the nephron?
Renal corpuscle
Renal tubule
Flow of urine coming out of nephrons in the kidneys (Plural)
Urine flows from the major calyces, into the renal pelvis, & then the ureters or another version for 1 kidney:
Calyx, renal pelvis, ureter, urinary bladder, urethra
Storage & Elimation of Urine
Ureters
The ureter is a tubular organ that extends from each kidney to the urinary bladder
Its wall has mucous, muscular, & fibrous layers
Peristaltic waves in the ureter force urine to the urinary bladder
Obstruction in the ureter stimulates strong peristaltic waves & a reflex that decreases urine production
Urinary Bladder
The urinary bladder is a distensible organ that stores urine & forces it into the urethra
The ureters & urethra open at the 3 angles of the trigone in the floor of the urinary bladder
Urethra
The urethra conveys urine from the urinary bladder to the outside
In females, it is short & empties between the labia minora
In males, it is long & conveys products of reproductive organs as well as urine
How do the following hormones affect the urinary system: ADH, aldosterone, ANP?
ADH
Water concentration in blood too high - ADH increases - results in increased reabsorption of water back into blood - urine volume decreases, darker in color as it is more concentrated
Water concentration in blood too high - ADH decreases - resuls in decreased ADH - decreases water reabsorption & urine volume increases, urine color pale, & very dilute concentration
If tubular reabsorption in the nephron didn’t occur then there would be excessive water loss
Aldosterone
Aldosterone stimulates Na+ reabsorption (conserved) & K+ to be excreted
Renin
Functions to increase blood pressure
How is active transport used in the renal tubule? Passive transport?
Ex. Active Transport
Active transport occurs in the kidney w/glucose molecules, bc there is a higher concentration of glucose in the blood than in the nephrons so to get the glucose to go into the blood active transport is required
This reabsorption of glucose all takes place in the proximal tubule
Ex. Passive Transport
Passive transport is osmosis, which is a passive transport bc it does'n’t require any energy to happen
An ex of this is the interstitial fluid (liquid found between the cells in tissue spaces), bc the intersititial fluid found outside of the kidney is more concentrated than the inside of the nephron tubules
So the water moves out of the kidney & into the blood by osmosis, a passive transport
Describe the histology of the glomerular capsule
Glomerulus: Also known as renal corpuscle
Renal corpuscle made up of:
Glomerulus
Glomerular capsule
Afferent arterioles delivers blood to each glomerulus
Capillary cluster that branches from afferent arteriole is glomerulus
Filters blood in each nephron
Renal arterioles deliver blood to each of the million or so glomeruli in each kidney
Remember capillaries are single layer structures that allows for substances to move in & out of capillary
What is the function of the glomerulus?
The glomerulus is a small bundle of capillaries (blood vessels) located at the beginning of each nephron in the kidney
These capillaries are important in the filtration of blood
The glomerulus allows smaller molecules, such as water & nutrients, to pass through its pores into the surrounding Bowman’s capsule
Larger molecules, such as waste products & red blood cells, are to large to pass through the pores & remain in the blood
The glomerulus transports water & small solutes from the body to the outside
Aside from waste, the filtrate contains important ions, glucose, amino acids, & smaller proteins that the body requires
Altering the diameter of arterioles leading into & draining from a glomerulus will alter the filtration pressure wthin that glomerulus
** Vasoconstriction of the afferent arteriole &/or vasodilation of the efferent arteriole
Results in a decrease in glomerular filtration rate (GFR)
Renal Tubule: tubule w/multiple names for various sections of nephron each having different function:
Leading away from the capsular space, filtered fluid enters the renal tubule on the proximal end of the nephron, which is appropriately called the proximal tubule, The renal tubule continues as the hairpin-shaped nephron loop (loop of henle). The proximal tubule dips toward the renal pelvis to become the descending limb of the nephron loop. The tubule then curves back toward its renal corpuscle & forms the ascending limb of the nephron loop. The ascending limb returns toward its renal corpuscle of origin, where it becomes the distal tubule
*Putting together in short form:
Extends from glomerular capsule to collecting duct
*Filtrate proceeds from Glomerular Capsule → (renal tubules) Proximal tubule → Nephron loop (loop of henle, composed of a descending & an ascending limb) → Distal tubule
Distal tubules of several nephrons (remember there are approximately 1 million nephrons/kidney) empty into a collecting duct
Collecting duct continues through the medulla & drains through the renal papilla into a minor calyx
Detrusor Muscle
The bladder serves to store urine until an appropriate time for urination. The wall of the bladder is made of the detrusor muscle, which is smooth muscle, & an overlying mucosal layer which is lined by uroepithelium
The detrusor muscle is essentially what most people refer to as “the bladder”
The detrusor muscle relaxes to allow urine to fill the bladder & stretches to hold more urine
When it is time to urinate, the detrusor muscle contracts to push urine out of the bladder
The detrusor muscle can malfunction in 2 main ways
It can be overactive (contract too much, when not needed) or underactive (doesn’t contract when it should)
If the detrusor muscle is overactive, it contracts to squeeze the urine out even when the person is not ready to urinate
This can cause a sense of urgency or severe desire to urinate.
When this urge occurs but the patient doesn’t loose urine, we call it overactive bladder/overactive detrusor muscle
If the squeeze of the detrusor muscle is strong enough, it can push urine out even if the patient is ready to urinate
When you lose urine bc of an overactive detrusor muscle, it is called urge incontinence
If the detrusor muscle doesn’t contract (squeeze) or is overstrecthed, it can be difficult to get urine out even when you are trying to urinate
Bc of that, you will retain urine, called urinary retention
External Urethral Sphincter
The urethral sphincters allow regulation of urine flow
Made up of skeletal muscle
Micturition-the act of urinating
The micturition reflex can be suppressed by higher centers of the brain
So if you aren’t near a restroom & you have to urinate, the brain will send a signal down the spinal cord to the urethra to inhibit the micturition reflex
If you are ready to urinate, the brain sends the signal allowing you to voluntarily contract the external urethral sphincter & release urine into the toilet
Summary:
**The detrusor muscle contracts, the interal urethral sphincter relaxes, & urine is expelled through the urethra
The micturition reflex subsides, the detrusor muscle relaxes, the internal urethral sphincter contracts, & the bladder begins to fill w/urine again
Thirst
Highest percentage of intake comes from beverages we drink
Water intake must equal water loss to maintain water balance
Primary regulator of water intake → Thirst
Thirst Center - Located in brain
What substances should not be found in urine when testing?
Glucose- all reabsorbed back into bloodstream unless diabetic- exceeds renal threshold of 170mg/dl & above that level the rest remains in urine
Protein- kidney damage, infection
WBC- infection, pyelonephritis
RBC- infection, trauma to kidney, glomerulonephritis, tumor
Bilirubin- hepatitis, liver disease, etc
What is normal constituents of urine?
Main constituents of urine: urea & creatinine
Urea- a by product of amino acid catabolism in the liver
What terms are used to describe an increase or decrease in urine output?
Polyuria- increased output of urine
Oliguria- decrease output of urine
Anuria- zero output of urine-bad → renal failure
Hormone produced in kidney?
Erythropoietin
Helps to control the rate of red blood cell production
When plasma glucose concentration exceeds the renal plasma threshold → then glucose appears in urine
Remember as blood enters into the glomerulus for filtration, all of the glucose is filtered out into the filtrate & must be put back into the bloodstream. This occurs through the sodium-glucose cotransporters. If blood glucose exceeds 180 mg/dl, the renal threshold to reabsorb glucose is exceeded & the excess glucose will remain in the urine
Fasting urine sample
An abnormal finding in the urine would be glucose
FYI: If fasting, a normal person’s blood glucose would be between 70-100 mg/dl & glucose does not exceed the renal threshold & would all be reabsorbed back into the blood- no glucose in urine which is normal
FYI: If a person is a diabetic, & their fasting blood glucose exceeds about 180 mg/dl then you would expect to find glucose in the urine
Diurectics
Increase volume of urine excreted
Aging
Decrease in the release of renin
Impacts the control of blood pressure
Which substances get reabsorbed within the & secreted within the different parts of the Nephron?