week 6
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
124 Terms
neurology chapter 22 keypoints
Headache is a common condition, and patients worry that they may have something wrong with their brain. The intracranial structures are not usually sensitive to pain, however, and most headaches do not originate in the brain.
Migraine is a very common disorder, which reduces quality of life to an extent underestimated by people who do not have it.
By no means all migraine patients experience aura.
There are definitions of migraine with and without aura, but these sometimes need to be applied somewhat loosely in practice.
There are several types of migraine, which can occur at different periods of one and the same patient’s life. A migraine diagnosis should therefore not be rejected just because the patient has a history of migraine and the symptoms are now ‘completely different’.
There is a difference between the treatment for migraine attacks and prophylactic treatment.
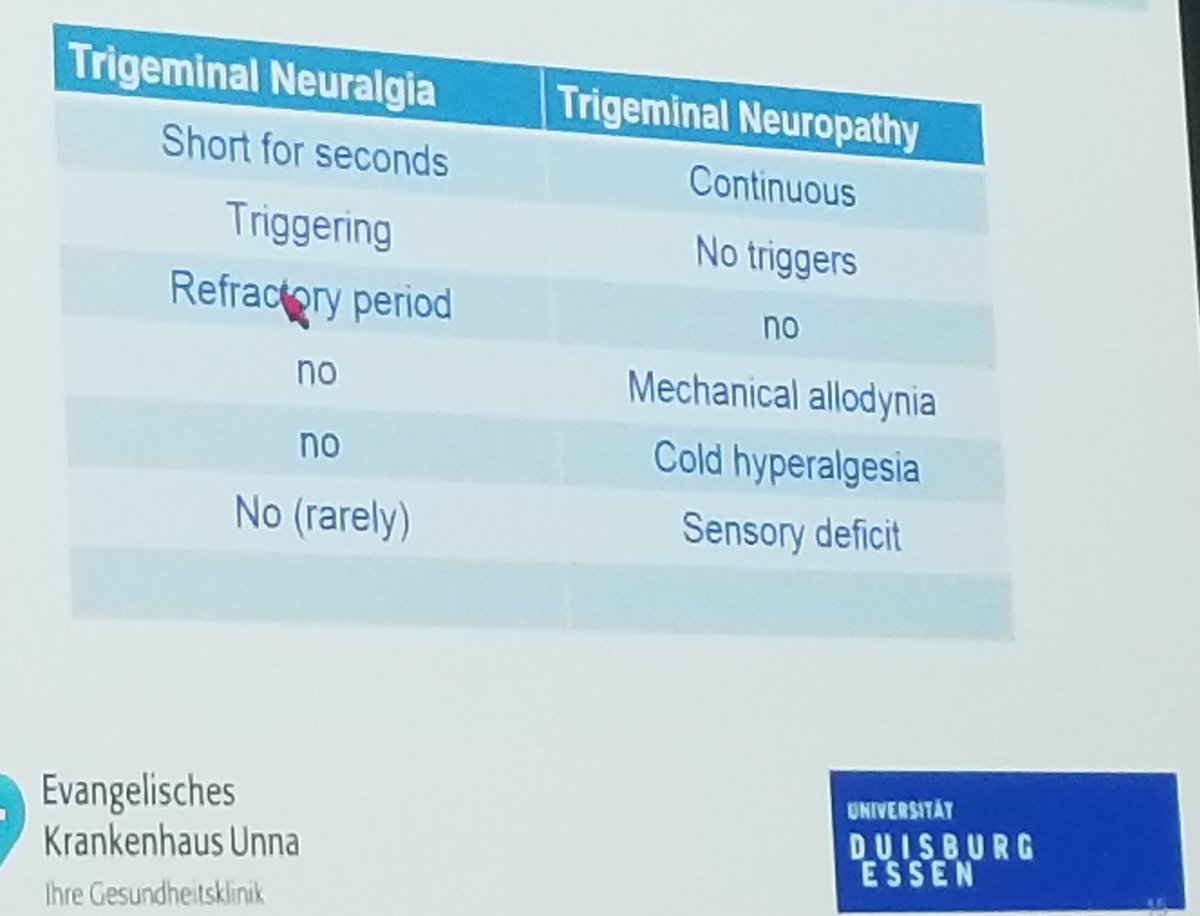
Different kinds of episodic pain can occur in the head and neck region. A shooting pain is referred to as ‘neuralgia’, trigeminal neuralgia being the most familiar type.
Trigeminal neuralgia is initially treated with sodium channel blockers. Surgery or radiosurgery to decompress the nerve is a good alternative.
Trigeminal neuropathy can cause chronic facial pain, which requires different treatment using analgesics for neuropathic pain.
It is not possible to diagnose all types of facial pain clearly.
Cluster headache follows a fairly characteristic pattern and should not be missed, as it is an excruciating pain that responds well to treatment.
A diagnosis of temporal arteritis should also not be missed in view of the risk of neurological deficit if it is not treated quickly.
Chronic headache is often referred to as ‘tension-type headache’. Overmedication should always be considered.
There are warning symptoms that every physician should be familiar with in cases of both chronic and acute headache.
Acute severe headache occurring for the first time should always be assessed in hospital.
examples of primary headaches
migraines or cluster headaches
more?
when is a headache primary
if there is no obvious cause and there is a stereotypical time pattern w/ characteristic accompanying symptoms
does brain tissue feel pain
no
if the brain cannot feel pain, what does
the basal meninges and large blood vessels (both arteries and large sinuses) can feel pain
a headache can also be caused by reduced or increased CSF pressure
the pain-sensitive structures in the anterior and middle cranial fossa are innervated by…
the trigeminal nerve (CN V)
the pain-sensitive structures in the posterior cranial fossa are innervated by…
the glossopharyngeal nerve (CN IX) and vagus nerve (CN X)
if the cause of pain is intracranial…
this will generally be due to traction on or irritation of the meninges (eg. inflammation, blood breakdown products or displacement of meninges by space occupying processes such as tumours and bleeds) and blood vessels (eg. vasodilation)
migraines
common, occurs in 25% of women and 8% of men at least once
particularly common around 40 y/o but they usually begin at a young age (in women around the menarche)
of those with migraines, 50% have monthly attacks, 35% have weekly and 15% a few times a year
often a positive family history
tends to occur around menstruation in women and may cease during pregnancy and after menopause
however, some women get migraines for the first time during pregnancy
attacks occur during periods of rest
onset after 50 is uncommon, suggests other diagnoses → imagining is indicated
a complete attack compromises a prodromal stage lasting a few hours or days
< than ½ of patients experience aura with: positive or negative visual symptoms (95–99%), sensory symptoms (35–40%), dysphasia (15–20%) and, least commonly, motor symptoms (15%)
an aura develops gradually over 5-20 minutes and lasts less than an hour
aura phenomena are usually unilateral when there are hemisensory symptoms, hemimotor symptoms or dysphasia
now just falls under ‘migraine with aura'‘
auras usually precede the headache and there is a headache-free interval lasting 15-30 minutes, but not always
attacks typically cause them to lie in bed and become hypersensitive to light and sound (sometimes to smells as well)
pain is throbbing, sometimes tight
some patients end up falling asleep and the headache is less severe when they wake up
nausea is common → relieved by vomiting
how does a migraine present in children
abdominal pain, or hallucinations of bodily distortion, referred to as Alice in Wonderland syndrome
prodromal stage of a migraine
lasts a few hours or days:
neck pain, mood changes, a feeling of stress, tiredness, pallor, frequent yawning, blurred vision, eating sweets, craving for sweet foods, fluid retention or sensitivity to sensory stimuli
fewer than half of patients experience aura with positive or negative visual symptoms (95–99 %), sensory symptoms (35–40 %), dysphasia (15–20 %) and, least commonly, motor symptoms (15 %). Aura phenomena are usually unilateral
aura phenomenon are usually…
unilateral
develops gradually over 5-20 minutes and lasts less than an hour
migraine accompagnee is…
when there are hemisensory symptoms, hemimotor symptoms or dysphasia
now just falls under ‘migraine with aura'‘
negative vs positive aural symptoms
Negative visual symptoms:
range from loss of a large part of the field of vision to homonymous hemianopia
or there can be scattered patches
another variant is where both fields of vision gradually become restricted from the outside
Positive symptoms:
take on characteristic shapes eg. sawtooth lines (fortifications, tilting) or elementary shapes such as squares or triangles
sometimes these are clearly coloured, often move
there can also be a sensation as if the picture is blurred by moving hot air, as seen above a tarmac road on a hot day (scintillations)
diagnostic criteria for migraine
migraine w/o aura (if at least 5 attacks have occurred)
headache for 4-72 hrs (untreated)
at least 2 of the following
unilateral location
pulsating pain
moderate or severe pain intensity
aggravation by or cause avoidance of routine physical activity
plus at least 1 of these 2
nausea and/or vomiting
photophobia and phonophobia
migraine w/ aura
at least 2 aura attacks that meet the following criteria
1 or more of the following completely reversible aura symptoms
visual
sensory
speech and/or language
motor
brainstem
retinal
at least 3 of the following 6 types of pattern
at least 1 aura symptom that gradually spreads over ≥ 5 min
2 or more aura symptoms occur in succession
each individual aura symptom lasts 5–60 min
at least 1 aura symptom is unilateral
at least 1 aura symptom is positive (e.g. flashes of light or pins and needles)
the aura is accompanied, or followed within 60 min, by headache
are the things that occur in migraines permanent
usually not but permanent loss of function sometimes occurs especially in particular hemianopia due to infarction in an occipital lobe = migrainous infraction
what are risk factors for migrainous infarction
aura, hypertension, smoking and oral contraception
pathophysiology of migraine attacks
a neurovascular disorder
genetic factors are involved
headache: reduced stimulation of vascular and neuronal serotonin receptors in the trigeminovascular system → vasodilation and a neurogenic response by the meninges → headache and other migraine symptoms
stress, fatigue and intolerance to certain foods are often cited as trigger factors, but these probably play only a minor role
cortical spreading depression plays a role in the case of aura
what is cortical spreading depression
a wave of sustained depolarization (neuronal inactivation) moving through intact brain tissue and associated with brain ischemia, migraine aura, and seizures
→ temporary loss of neuronal function → neurological symptoms
unusual types of migraine
basilar migraine → mainly found in young people, attack begins with gradual loss of vision in both eyes (sometimes w/ vertigo), followed by ataxia, dysarthria and bilateral numbness or paraesthesia then vomiting and occipital headache
theres sometimes amnesia, very occasionally loss of consciousness
migraine equivalents or migraine sine hemicrania or migraine aura w/o headache → get true migraine attacks but also auras w/o headaches
ophthalmoplegic migraine → whos attack ends with diplopia due to dysfunction of one oculomotor nerve (85%) or abducens nerve (15%) → can persist for 1 to 8 weeks
It is somewhat dubious whether this actually is migraine; it is nowadays often referred to as ‘recurrent painful ophthalmoplegic neuropathy’
familial hemiplegic migraine → autosomal dominant, aura w/ hemiparesis that can persist for many days after the attack, begins at a young age
→ mutations have been found in genes that code for neuronal ion channels (CACNA1A gene for a calcium channel, the ATP1A2 gene for a sodium-potassium channel)
→ there is also a sporadic form
retinal migraine → negative or positive visual aura phenomena are limited to 1 eye, possible due to spreading depression of the retina
status migrainosus → migraine attack that lasts >72 hrs, aura status lasting more than a week can also occur
chronic migraine → when there is migranous headachace more than hald the time over a period of >3 months
this can occur w/ and w/o excessive use of analgesics
vestibular migraine → attacks of vertigo in those w/ a history of migraines
treatment of migraine
taking an antiemetic as soon as an attack threatens
after 30 minutes they can take paracetamol or an NSAID
if antiemetics, paracetamol or NSAIDs dont work, consider triptans (serotonin receptor agonists) → orally, rectally, subcutaneously or as a nasal spray
these must NOT be taken during the aura, only once the headache starts
ergotamine used to be prescribed before triptans were used (i think?) → bind serotonin receptors but theyre both blockers and stimulants
→ works quite well but its vasoconstrictive action and the risk of dependency makes it used less
some dont take medicine, they prefer to rest in a dark room or sleep for a few hours until the worst of the headache has subsided
prophylactic treatment:
recommended strategy is to start with propranolol or metoprolol, possibly followed by one of the following: flunarizine, sodium valproate, candesartan, topiramate of amitriptyline
use of ergotamine as a prophylactic is not recommended
antagonists to calcitonin gene related peptide are new → play a role in pain transmission in the trigeminovascular system
→ antibodies to CGRP or the CGRP receptor are effective as prophylaxis for both episodic and chronic migraine
approximately 10% of migraine patients experience…
transient chest tightness with tingling
but true angina symptoms are rare
which 2 migraine drugs should not be used during pregnancy
triptans and ergotamine
when is prophylactic treatment of migraines considered
if the attacks occur twice or more per month or are less frequent but very protracted (lasting for days)
types of facial pain
trigeminal neuralgia
other neuralgias in the head and neck region
trigeminal neuropathy
temporomandibular disorder
atypical chronic facial pain
trigeminal neuralgia
mainly found in >50 y/o
very brief minor attacks (1-2 s), very sharp ‘electrical’ pains on one side of the face
pain is usually felt in the area innervated by the 2nd or 3rd branch of the trigeminal nerve, rarely in the area of the first branch
varying frequencies
triggered by speaking, eating, local cooling or a draught and in around 50% its triggered by touching a circumscribed area of skin = a trigger point
some patients avoid all facial movements, stop shaving or become malnourished
sharp pains are sometimes accompanied by facial tics (tic douloureux)
can end/start gradually or suddenly
examination does not reveal any sensory impairments but there might be exaggerated touch sensation
in younger people it may be caused by MS due to demyelination of the nerve root entry zone in the brainstem
treatment:
carbamazepine is generally very effective, can be combined with baclofen if needed
gabapentin and pregabalin are also used
another good option is microvascular surgery (Jannetta procedure) → surgical decompression of trigeminal roots at the base of the skull
it’s often discovered during the procedure that the root is being stretched or compressed by adjacent structures (eg. thickened or tortuous arteries)
jannetta procedure is not suitable if the cause of the neuralgia is MS → alternative treatment is stereotactic radiotherapy to deliberately damage part of the nerve
if none of these work or are not considered appropriate → coagulation of the gasserian ganglion can be done
A rare but feared adverse effect is corneal anaesthesia (if the first branch of the trigeminal nerve is affected) with poor healing of any ulcers, sometimes resulting in perforation; the damage to the nerve can also cause long-term or permanent loss of sensation in the area of skin concerned and pain (anaesthesia dolorosa) in addition to the numbness
when is jannetta procedure not suitable
if the neuralgia is caused by MS
alternative treatment is stereotactic radiotherapy to deliberately damage part of the nerve
tic douloureux is also known as trigeminal neuralgia on the internet though??? or is TC = trigeminal neuralgia + spasms???
where is pain of trigeminal neuralgia usually felt
in the area innervated by the second or third branch of the trigeminal nerve, rarely in the area of the first branch
typically one sided
glossopharyngeal neuralgia
pain is localised to one side at the back of the throat, radiating into the ear
triggered by swallowing and sticking the tongue out
trigger point = tonsillar fossa or the posterior pharyngeal wall
It should be noted that the anastomosis of nerve IX with nerve X during the attack can cause bradycardia or even heart block, causing the patient to lose consciousness
treatment → carbamazepine, decompression may also be helpful
other neuralgias***
Neuralgia of the intermediate nerve (a branch of the facial nerve) causes a shooting pain in the ear. There are also neuralgias of the occipital nerve on the back of the head (a diagnosis sometimes wrongly made when there is a continual pain in the occiput) and of the superior laryngeal nerve in the pharynx, radiating into the ear. Imaging is indicated in these cases (see e.g. case study 2.1). These neuralgias are so rare that there is no standard treatment: medication as referred to above has been tried, as has infiltration of the nerves in question
trigeminal neuropathy
difference from trigeminal neuralgia → trigeminal neuropathy causes continuous pain which is exacerbated by touching but WITHOUT a trigger point AND sensation is impaired in the affected area
if this occurs in the first branch of the trigeminal n. its mainly post-herpetic neuropathy (= after herpes zoster infection in this area)
mostly clears up in the course of months or up to 2 years
most chronic forms cause hyperapthia = a painful syndrome characterized by an abnormally painful reaction to a stimulus, especially a repetitive stimulus, as well as an increased threshold
but its often painless, with symptoms mainly being an unpleasant unilateral or bilateral numbness → unpleasant sensations can sometimes be treated symptomatically w/ amitriptyline
the more chronic forms are often accompanied by a malignant disease or mixed connective tissue disease
gabapentin and pregabalin are also claimed to have an effect, but patients are often disappointed with drug treatments
trigeminal neuropathy vs neuralgia
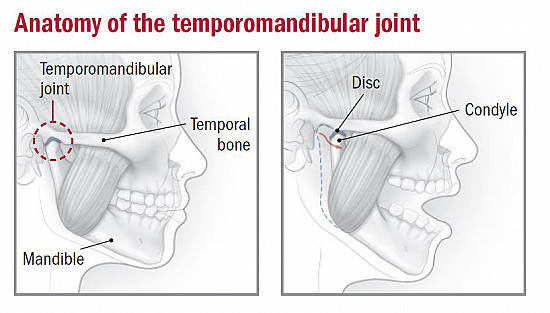
temperomandibular disorder********
= a group of disorders where a dysfunction of the maxillary joint and/or masticatory muscles occurs
disc displacement (check photo) can cause acute pain, usually with restricted movement
chronic pain in the region of the maxillary joint radiating into the temporalis that is exacerbated by chewing can be caused by discopathy and osteoarthritis
impaired occlusion and chronic tension in the masticatory muscles can be a contributory factor or a primary cause
atypical chronic facial pain***
The pain is deep-rooted and chronic and does not have the typical characteristics of the syndromes described above. A variety of specialists have been unable to find any cause in their areas. There is sometimes a depressive disorder, and the pain clears up if this is treated, but in many cases the cause remains unknown
cluster headache
= episodic, very severe throbbing or stabbing pain in and around an eye, radiating into the temple or the angle of the mandible
max pain is at 5-15 minutes, persists for 15 min to a few hours and subsides in 5-15 minutes
first attack is between 10-50 y/o
cause is unknown but dysfunction of the hypothalamus appears to play a role
90% of these patients are heavy smokers, but stopping smoking has not been found to affect the frequency of attacks
there are vegetative symptoms on the side where the pain is, e.g. lacrimation, conjunctival redness, nasal congestion or conversely nasal discharge, and a proportion of patients also have Horner’s syndrome, which can persist after the attack
hardly ever accompanied by nausea or vomiting unlike migraines
prodromal symptoms are rare but an aura can occur
Unlike the behaviour displayed by patients during a migraine attack, they do not seek bed rest but roam around at their wits' end, often inventing strange manipulation techniques to suppress the headache. Many patients report suicidal thoughts during an attack
forms
in clusters lasting weeks to months (episodic form), 1 or more times per 24 hr in each cluster
→ most common form
→ tendency to occur during nocturnal sleep
→ clusters occur with an average frequency of once a year but with a large individual spread
→ during a cluster period, small amounts of alcohol can trigger an attack, as can sublingual nitroglycerin
not clustered (chronic form) → no attack free periods
attacks often respond well to treatment
doesnt respond to traditional analgesics (even opiates) or carbamazepine or beta blockers
inhaling pure O2 helps in 65% of patients within 10-15 minutes usually in the case of milder attacks
subcutaneous injection of sumatriptan also helps
verapamil hydrochloride is an effective prophylactic if started at the beginning of a cluster
a brief course of prednisone is sometimes therapeutic
chronic form may respond well to lithium treatment
suboccipital injections of methylprednisolone and electrical stimulation of the greater occipital nerve have also been reported to be effective
on the affected side of a cluster headache there are…
vegetative symptoms → lacrimation, conjunctival redness, nasal congestion or conversely nasal discharge, and a proportion of patients also have Horner’s syndrome, which can persist after the attack
diagnostic criteria for cluster headaches
recurring (at least 5) attacks of severe or very severe unilateral orbital, supraorbital and/or temporal pain
duration: 15–180 minutes (when untreated)
frequency: from every other day up to eight times a day
Plus 1 or both of the following accompanying symptoms:
at least one of the following symptoms or signs on the side of the headache:
conjunctival injection and/or lacrimation
nasal congestion and/or rhinorrhoea
eyelid oedema
forehead and facial sweating
miosis and/or ptosis
sense of restlessness or agitation
during a cluster period in cluster head aches, … can trigger an attack
small amounts of alcohol can trigger an attack, as can sublingual nitroglycerin
>90% of cluster headache patients…
are smokers
chronic paroxysmal hemicrania**********
Another much rarer (a 100-fold less common) type of episodic headache, far more common in women than in men, is chronic paroxysmal hemicrania . This disorder can start at any age, but usually does so after the age of 30. The very severe unilateral headache attacks last 2–30 minutes but can recur between ten and twenty times a day. During an attack there is conjunctival injection. There would seem to be both stimulation of the parasympathetic nervous system (constricted pupil, nasal discharge, lacrimation, ptosis, swollen eyelid) and sympathetic nervous system (perspiration, reduced salivation). The attacks respond very well to indometacin, and this is a criterion for the diagnosis
short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT)*******************
an extremely rare condition, short-lasting unilateral neuralgiform headache with conjunctival injection and tearing ( SUNCT ), which causes a stabbing pain in the area innervated by the first branch of the trigeminal nerve, usually for five seconds to two minutes. These attacks too occur in clusters, three to 200 times a day. In many cases there is not only ipsilateral conjunctival redness and tearing but also nasal congestion, nasal discharge, eyelid oedema, miosis or ptosis, sometimes facial redness and sometimes perspiration. This differs from trigeminal neuralgia, then, in the occurrence of autonomic symptoms and the duration of the attacks
temporal arteritis
pain localised mainly in the temple where the skin and temporal artery are thickened and tender and arterial pulses are reduced or absent
usually form part of a more general arteritis which occurs particularly in the ocular arteries and can cause sudden vision disorders
unknown cause
there is also often pain in the pectoral girdle muscles (polymyalgia rheumatica → but not connected to rheumatism despite the name)
claudication of the jaw (pain when chewing) is a highly specific symptom of temporal arteritis
raised ESR + theres often moderate anemia
diagnosis is confirmed by biopsy from the temporal artery
high dose prednisone clears up the pain within a few days (sometimes a few hours), but a maintenance dose has to be taken over a long period (about 2 years)
what is a highly specific symptom of temporal arteritis
claudication of the jaw (pain when chewing)
why is there no pulse in the temporal artery in temporal arteritis???***
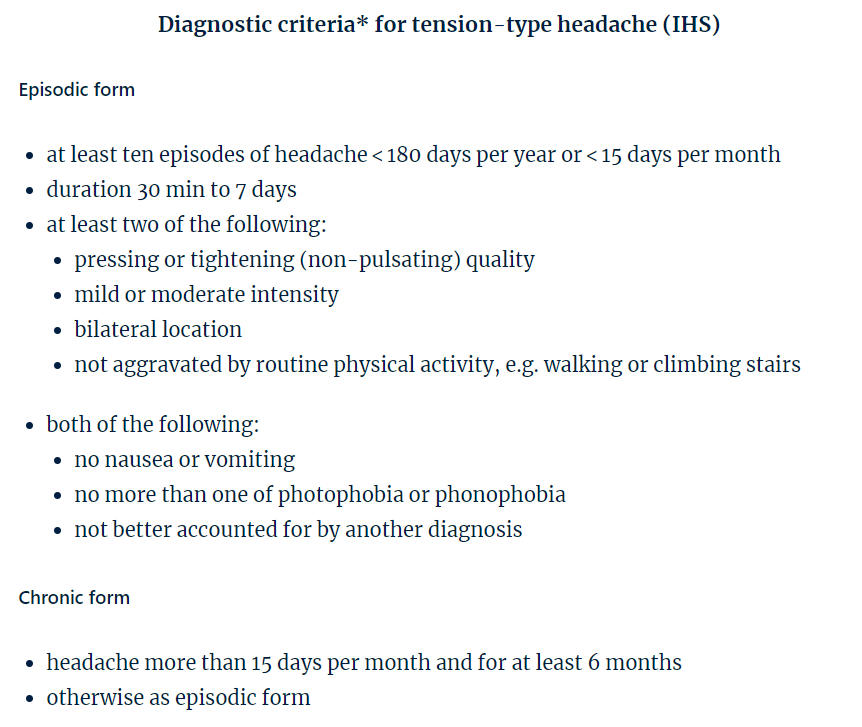
tension type headache
named despite there hardly ever being a connection w/ muscular or mental tension (but they also references to MUSCULE tension headache???)
diagnosis when there is no other likely cause (??? not sure)
its chronic and intermittent often exacerbations but there can be spontaneous remissions sometimes lasting for years
types
episodic → pain comes in fits and starts or attacks
→ the most recent diagnostic criteria (IHS, 2018) further divide the episodic form into a non-frequent and a frequent form and a form with and without sensitivity around the head
chronic → virtually continuous
The treatment consists first and foremost in explaining the mechanism responsible (which is not a brain abnormality). Analgesics are indispensable during exacerbations, but continuous treatment with painkillers or tranquillizers (benzodiazepines) is undesirable. A temporary course of amitriptyline (10–75 mg ante noctem) may be worthwhile
analgesic dependent headache
due to long term use of various headache painkillers
attacks occur almost daily, especially in the morning
by definition it must be more than 14 days of headaches per month with more than 3 months of overmedication
occurs particularly in patients using the medication for another headache syndrome (often migraine or tension-type headache) and not e.g. in the case of chronic use of NSAIDs for disorders of the musculoskeletal system
only treatment is abstention from the medication in question for a few months
cough headache = a coughing fit followed within a few seconds by a splitting headache that can persist for up to 30 minutes
→ in some cases its reasonable to assume there is an anomaly in the craniovertebral junction (tonsillar descent, chiari malformation etc)
exertional headache = a diffuse headache following physical exertion that lasts between 5 minutes and 2 days
→ patients with this problem quite often have migraine or orgasmic/post-coital headache as well, so a migrainous cause is suspected
acute headache
if a patient suffers a sudden agonizing headache (thunderclap headache), the first thing to consider should always be subarachnoid haemorrhage or some other vascular cause
consider other possibilities once ^ are excluded (eg. cocaine use and acute hypertension (phaeochromocytoma) + the neurovascular causes in this summary)
usually theres no structural abnormality (idiopathic thunderclap headache) especially in post coital/orgasmic headache
post coital/orgasmic headache → occipital or diffuse pain, unilateral (33%) or bilateral (67%)
attacks last on average 30 minutes and never more than 24 hrs
many patients also have a type of migraine or muscle tension headache
what should firstly be considered with a sudden agonising headache (thunderclap headache)
subarchnoid haemorrhage or some other vascular cause
consider other possibilities once ^ are excluded (eg. cocaine use and acute hypertension (phaeochromocytoma) + the neurovascular causes in this summary)
warning symptoms in cases of headache
Acute headache
acute onset of maximum-intensity headache
fever
neurological symptoms during the headache
nausea and vomiting (except in the case of migraine)
diplopia
impaired consciousness
meningism
triggered by increases in pressure (cough, orgasm)
Chronic headache
onset after the 40th year of life
onset in the early morning
slowly progressive over a few weeks or months
neurological abnormalities
diplopia
triggered by increased pressure
triggered by change in position
meningeal irritation
morning sickness
papilloedema
hypertension, relatively low heart rate
if a headache presents no alarming features and no abnormalities are found on physical examination…
an organic lesion is very unlikely but of course never entirely out of the question
meningitis is usually caused by…
a virus, in which case the prognosis is good and the treatment is usually symptomatic
bacterial meningitis is less common but more severe
the key symptoms of infections of the CNS and cerebral meninges…
fever and headache but it doesnt mean theyre always there
very young and very old patients generally display even fewer classic symptoms
neurology chapter 24 key points
When treating bacterial meningitis, the first step is to administer corticosteroids. If meningitis is suspected, antibiotics should be started as soon as possible.
A diagnosis of meningitis always involves the preparation of blood cultures.
As a result of vaccination, meningitis has now become a disease of older adults. Pneumococci are the main pathogens in the western World.
Infections can sometimes produce a space-occupying lesion, rather like a brain abscess. As a result, an initial diagnosis of brain tumour is often made.
While syphilis is rare in North-West Europe, a failure to diagnose it can have serious consequences.
Neuroborreliosis is a multifaceted infection. This is an increasingly common disease in North-West Europe, as a growing percentage of ticks are infected with the bacterium.
CNS infections caused by fungi, yeasts and parasites are…
rare, except in patients with a weakened immune system (eg. in HIV)
in meningitis, the infection is confined to…
the meninges and subarachnoid spaces
purulent meningeal inflammations are caused by…
bacterial infections
which pathogens dont adhere to the ‘purulent = bacteria’ rule
TB, syphilis and spirochaetes
what is inflamed in encephalitis or myelitis
the brain parenchyma or spinal cord
bacterial vs viral encephalitis/myelitis
Bacterial infections are soon encapsulated, causing an abscess . When a purulent inflammation is found in the subdural space, this is referred to as a subdural empyema
Viral inflammations of the brain parenchyma cause more diffuse changes affecting the entire cerebrum or mainly one lobe (e.g. the temporal lobe)
bacterial meningitis
in 50% it presents as an acute illness w/ symptoms developing within 24 hrs
40% of adults have risk factors for bacterial meningitis = disorders that impact the immune system (immunosuppressants, HIV, alcoholism, diabetes etc) and bacterial infections elsewhere in the body
one particular group of people who are at increased risk are those who have suffered a skull fracture in the past or who have liquorrhoea (CSF leak) from the nose or ear following an accident or operation → provides the bacteria with a port of entry to the brain
>80% develop headache, vomiting, photophobia and high fever
80% have a stiff neck but the ‘classic triad’ of a stiff neck, fever and diminished consciousness is only found in 50%
illness is often preceded by a few days of general malaise and inflammation of the ear or paranasal sinus
20% are in a coma on admission, some develop cerebral herniation within a few hours due to the fulminant (sudden) inflammation
in the acute phase, 1/3 have a neurological deficit, usually aphasia, hemiparesis or cranial nerve palsy
the most common cranial nerve palsy involves the oculomotor (III), abducens (VI), facial (VII) and vestibulocochlear (VIII) nerves
a small proportion have an epileptic seizure, this is particularly the case in pneumococcal meningitis
meningococcal meningitis → usually has a mixed presentation of meningitis and sepsis w/ disseminated intravascular coagulation which causes petechiae or exanthema which are small infarctions caused by embolisms containing infected material (so the meningococcus can be cultured from a skin biopsy of the petechiae or exanthema)
symptoms of meningeal irritation and fever are often mild or absent in young infants and neonates
!! in neonates it may present with hypothermia !!, jaundice and poor feeding
in infants → general malaise, drowsiness, unwilling to eat, vomiting or diarrhoea, they may cry when their diapers are changed (leg pain during changing due to meningeal irritation)
in infants w/ bacterial meningitis, why may they cry when their diapers are changed
due to leg pain during changing due to meningeal irritation
how may bacterial meningitis present in neonates
hypothermia !!, jaundice and poor feeding
patients with meningococcal meningitis often have a mixed presentation of…
meningitis and sepsis, with disseminated intravascular coagulation causing small skin bleeds (petechiae or exanthema) = small infarctions caused by embolisms containing infected material. The meningococcus can, therefore, be cultured from a skin biopsy taken from these skin abnormalities
which type of meningitis is more likely to present with an epileptic seizure
pneumococcal meningitis
(if it occurs) what is the most common cranial nerve palsy in the acute phase of bacterial meningitis
palsy of the oculomotor (III), abducens (VI), facial (VII) and vestibulocochlear (VIII) nerves
what is the ‘classic triad’ in bacterial meningitis despite only being found in 50%
stiff neck, fever and diminished consciousness
80% have a stiff neck but the triad is way less
…% of adults have risk factors for bacterial meningitis
40
= disorders that impact the immune system (immunosuppressants, HIV, alcoholism, diabetes etc) and bacterial infections elsewhere in the body
other → otitis, sinusitis, liquorrhoea
what is one specific risk factor for bacterial meningitis (not immunosuppression or other bacterial infections)
those who have suffered a skull fracture in the past or who have liquorrhoea (CSF leak) from the nose or ear following an accident or operation → provides the bacteria with a port of entry to the brain
CSF leak / liquorrhoea
an abnormal communication between the intracranial compartment and the sinonasal or tympanomastoid cavities of the skull base
most patients w/ bacterial meningitis develop
headache, vomiting, photophobia and high fever
illness is often preceded by a few days of general malaise and inflammation of the ear or paranasal sinus
diagnosing bacterial meningitis
not hard if the classic triad is there, but its only there in 50%
DDx will always include viral meningitis or encephalitis, sepsis or influenza
if bacterial meningitis is suspected, history taking and physical examination are generally insufficient to rule it out, so CSF testing will be needed
a lumbar puncture can be dangerous due to risk of cerebral displacement, withdrawing CSF at lumbar level creates a pressure difference that displaces brain structures in the caudal direction, which can cause compression of the brainstem
patients with severely diminished consciousness or focal neurological signs therefore need to undergo a brain CT scan before the lumbar puncture is carried out
!! if a CT is needed before a lumbar puncture, start them on antibiotics and dexamethasone before being sent to radiology BUT do take a blood culture to test the bacteria for
always correct a coagulation disorder before a lumbar puncture
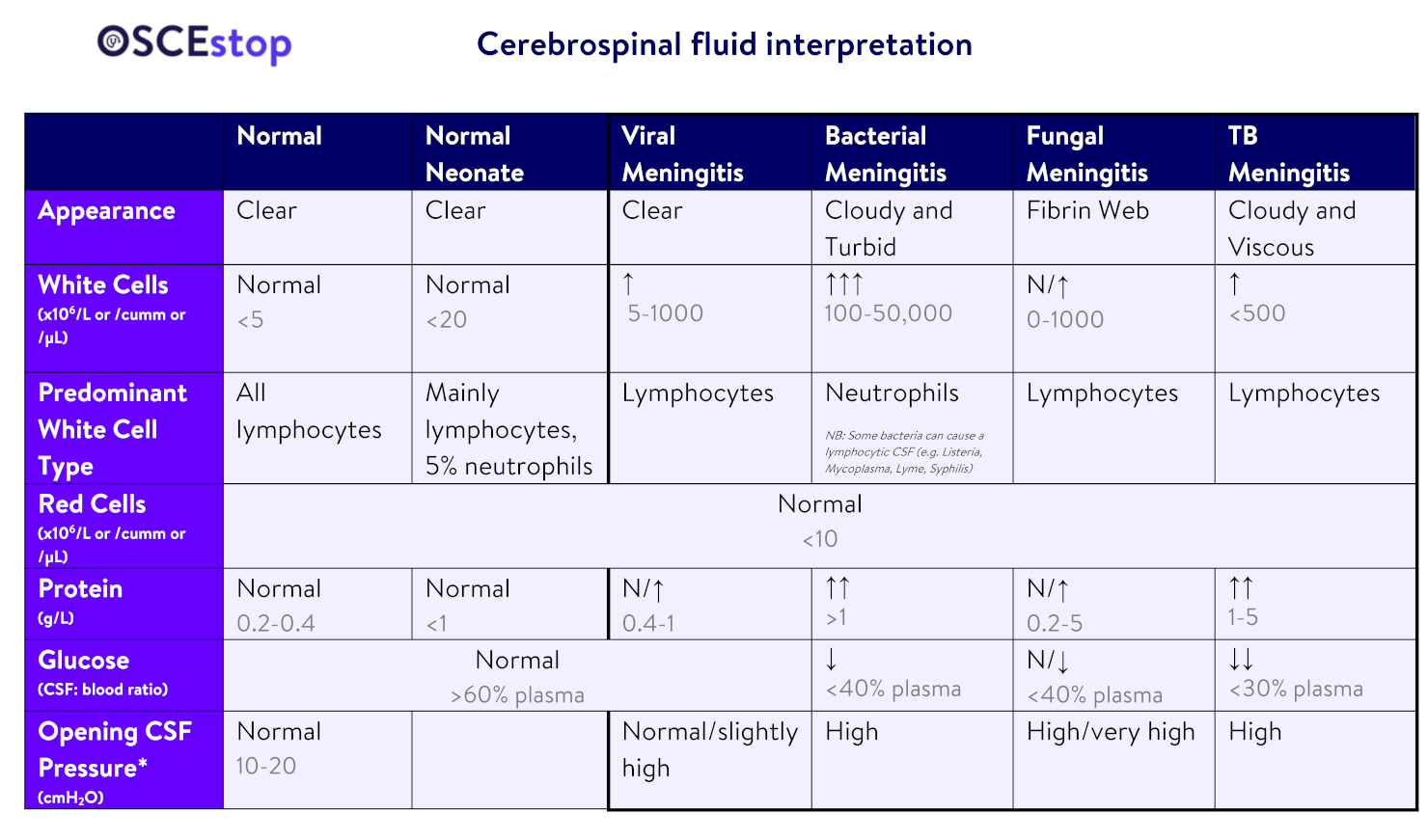
features of the CSF → markedly elevated opening pressure in a lumbar puncture, yellow and cloudy (purulent), leukocytosis, mainly granulocytes, reduced sugar and increased protein
gram preparation of the CSF → usually positive after 1/2 days but it remains negative in around 20% especially those given an antibiotic before the puncture
!! this is why a blood culture is taken if patients need a CT before a lumbar puncture and are therefore given antibiotics before the puncture
PCR can also be used
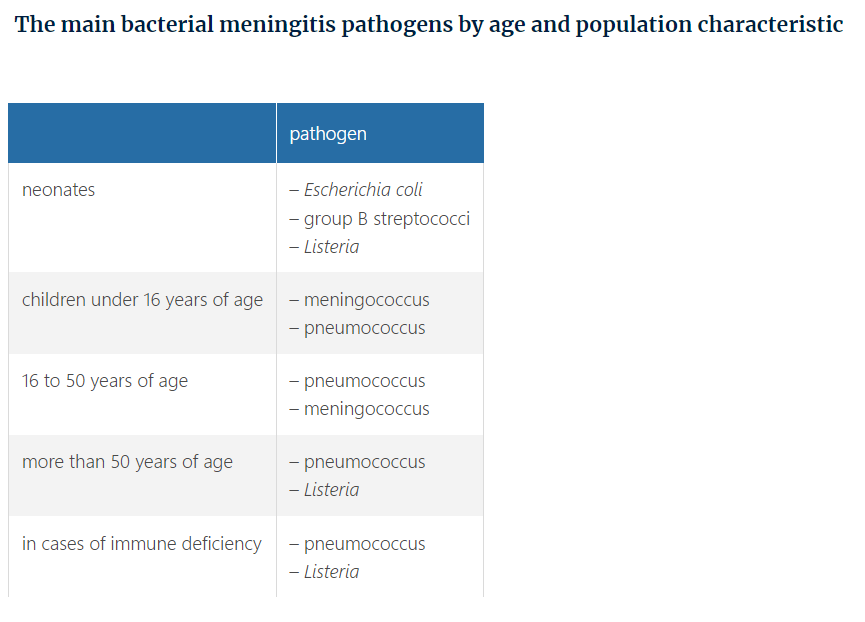
what is the most common pathogen causing bacterial meningitis/meningitis in general
pneumococcus, followed by meningococcus (found mainly in children and young adults)
Other types of pathogens are often found in particular patient populations. Listeria monocytogenes is the third most common pathogen responsible for bacterial meningitis and is found mainly in the elderly and in patients with a compromised immune system. The causes of some small-scale Listeria epidemics have been traced to contaminated foods such as soft cheese and ready meals. Patients with a combination of bacterial meningitis and endocarditis are at high risk of Staphylococcus aureus Meningitis in neonates (up to the sixth week after birth) is usually caused by group B streptococci ( Streptococcus agalactiae ) or Escherichia coli
CSF gram preparation remains negative in…
around 20% especially those given an antibiotic before the puncture
this is why a blood culture is taken if patients need a CT before a lumbar puncture and are therefore given antibiotics before the puncture
features of the CSF in bacterial meningitis
markedly elevated opening pressure in a lumbar puncture, yellow and cloudy (purulent), leukocytosis, mainly granulocytes, reduced sugar and increased protein
if a CT is needed before a lumbar puncture…
start them on antibiotics and dexamethasone before being sent to radiology
what is dangerous to do while trying to diagnose (bacterial) meningitis
lumbar puncture due to risk of cerebral displacement, withdrawing CSF at lumbar level creates a pressure difference that displaces brain structures in the caudal direction, which can cause compression of the brainstem
what can cause cerebral displacement
a brain abscess, cerebral infarction, subdural empyema or hydrocephalus
and i guess a lumbar puncture
statement: Lumbar punctures, besides being diagnostic, can be used to drain CSF thus reducing the ICP. The limitation to this is raised ICP secondary to mass effect with a possible risk of herniation if the CSF pressure drops too low
pneumococcal meningitis
most common bacterial meningitis pathogen
pneumococcus is found in 70% of adults and a large proportion of children beyond the neonatal period
most patients will have a predisposing factor for bacterial meningitis (eg. otitis, sinusitis, pneumonia, liquorrhoea, or an immune deficiency (in particular diabetes, alcoholism, splenectomy, cancer, and HIV infection))
at A&E, 1/5 are already in coma and >80% have diminished consciousness
common complications while in the hospital → cerebral infarctions, cerebral venous sinus thrombosis, epilepsy, cerebral oedema and hydrocephalus (> 1/2 develop a neurological complication of this kind while in hospital, but systemic complications such as sepsis and respiratory insufficiency are also common)
due to the high frequency of complications about 20% of patients die
almost ½ of those who survive have residual symptoms (eg. hearing loss, focal neurological deficit such as hemiparesis or loss of sensation, and cognitive disturbances)
→ ½ of those patients who do not apparently have any residual symptoms are found to have mental sluggishness and cognitive disorders
to prevent reinfection from an otogenic or sinogenic focus of infection, consult an ENT specialist at an early stage to track down the focus and clean it out if needed
also consult them if there is a hearing disorder (bc a cochlear implant surgery can only be performed at an early stage following meningitis)
treatment:
high doses of IV penicillin, amoxicillin or a cephalosporin, depending on the resistance pattern
temp. course of dexamethasone (prior to or at the same time as antibiotics) cuts the mortality rate from 30 to 20%
if there is a hearing disorder following meningitis…
consult an ENT as soon as possible bc a cochlear implant surgery can only be performed at an early stage following meningitis
> ½ of those w/ pneumococcal meningitis develop … in the hospital
neurological complications such as cerebral infarctions, cerebral venous sinus thrombosis, epilepsy, cerebral oedema and hydrocephalus
but systemic complications such as sepsis and respiratory insufficiency are also common
meningococcal meningitis (neisseria meningitidis)
responsible for small scale epidemics of meningitis in places where adolescents and young adults live together in close proximity (eg. military barracks and student accommodations)
meningococcus is found as a commensal in the nasopharynx in many people
in a small proportion it gains access into the bloodstream and avoids the immune system → crosses the BBB
recall that it can cause a mixed presentation of sepsis and meningitis
If sepsis is more prominent, toxic shock syndrome can develop, causing disseminated intravascular coagulation in addition to the sepsis. Small skin bleeds (petechiae) are a manifestation of this
^ is referred to as waterhouse-friderichsen syndrome (check separate card)
other complications that occur reasonably frequently are autoimmune arthritis (12%), hearing loss (20%) and cranial nerve palsy (6%)
mortality rate is 7% in adults and 4% in children mainly due to simultaneous occurrence of sepsis
it MUST be reported to the municipal health authority + those in the patients immediate social circle must be given a 2 day course of oral rifampicin or ciprofloxacin as a prophylactic to eliminate the meningococcus from the nasopharynx (bc its a contagious disease)
treatment:
penicillin, because penicillin resistant meningococci are rare
oral rifampicin or ciprofloxacin are also given to the patients before discharge from hospital if the treatment was penicillin monotherapy, not indicated for those given cephalosporin
meningococcal meningitis is a contagious disease so…
it MUST be reported to the municipal health authority + those in the patients immediate social circle must be given a 2 day course of oral rifampicin or ciprofloxacin as a prophylactic to eliminate the meningococcus from the nasopharynx
oral rifampicin or ciprofloxacin are also given to the patients before discharge from hospital if the treatment was penicillin monotherapy, not indicated for those given cephalosporin
meningococcus is found as…
a commensal in the nasopharynx in many people
meningococci can cause both…
meningitis and sepsis → mixed presentation
if petechiae are present in meningococcal meningitis / sepsis it means…
that toxic shock syndrome has developed
waterhouse-friderichsen syndrome***
defined as adrenal gland failure due to bleeding into the adrenal glands, commonly caused by severe bacterial infection. Typically, it is caused by Neisseria meningitidis
leading to massive blood invasion, organ failure, coma, low blood pressure and shock, disseminated intravascular coagulation (DIC) with widespread purpura, rapidly developing adrenocortical insufficiency and death
why is there a bleeding tendency in waterhouse-friderichsen syndrome
due to consumption of coagulation factors
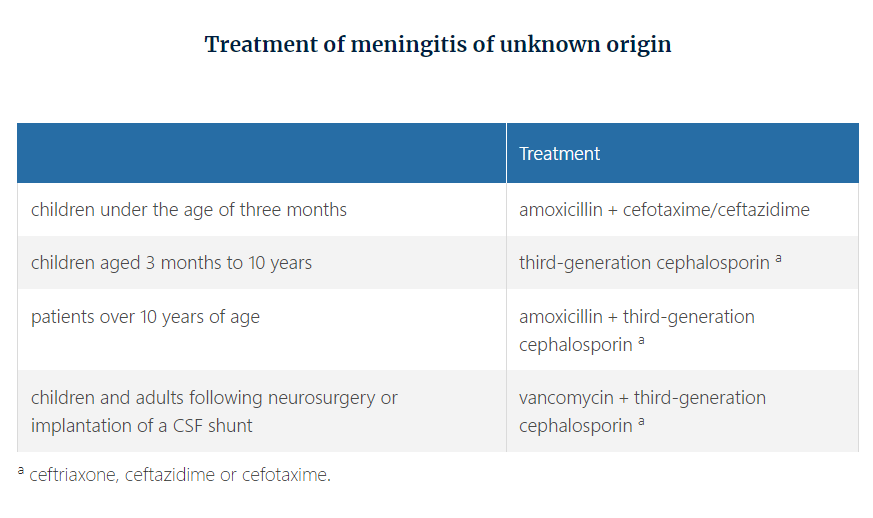
treatment of meningitis of unknown origin
Targeted parenteral antibiotic treatment needs to be continued for seven to 14 days, or three weeks in the case of some pathogens such as Listeria, E. coli and staphylococci. The focus of the infection (otitis, sinusitis, empyema, abscess, endocarditis) needs to be determined in all patients with pneumococcal meningitis and meningitis caused by H. influenzae or S. aureus. Any primary focus of infection should be cleaned out if necessary. If any additional infections, such as endocarditis, are identified, this may cause antibiotic treatment to be extended by up to six weeks.
… are almost always sensitive to penicillin
meningococci, pneumococci and other streptococci
Haemophilus influenzae frequently has reduced sensitivity to penicillin, and Listeria monocytogenes is insensitive to cephalosporins
adding dexamethasone to the antibiotic treatment has substantially improved the prognosis for…
pneumococcal meningitis (at least in adults)
brain abscess
caused by local inflammation of the brain tissue (local cerebritis)
40% of brain abscess cases are due to spread of an ENT infection (25% → invasion of bacteria from the blood stream, 10% → penetrating head trauma, 20% → no focus found)
if it occurs due to metastasis of pus from elsewhere, its usually the lungs
most common microorganisms are: streptococci, staphylococci, E. coli and Proteus mirabilis
manifests as a space occupying lesion and/or inflammatory process
classic triad → fever, focal neurological signs and headache but only found in 20%
65% → headache, 60% → nausea, 50% → neurological deficits, 25% → epileptic seizures, 5% → fever
CT or MRI is the test of choice
1/5 have multiple brain abscesses
suspected? → consult with a neurosurgeon at an early stage → confirm by a puncture (open or stereotactic aspiration) and identifying the pathogen
drain or excise (only in those who have an easily accessible superficial abscess) the abscess at the same time
be wary with lumbar punctures due to the risk of herniation
CRP, blood cultures and CSF testing can assist with DDx but rarely ever diagnose brain abscess or identify the pathogen
always find the focus to treat it
no clear focus? need to be examined by a cardiologist (including an echocardiogram), a dentist to rule out a dentogenic focus and an ENT specialist (with imaging of the mastoid process and sinuses)
drain or excise? antibiotics for a minimum of 6 weeks
treat cerebral oedema w/ dexamethasone
around 30% of patients are left with focal neurological deficits due to scarring, usually in the form of focal epilepsy
excision of a brain abscess is done…
only in those who have an easily accessible superficial abscess
if there is no clear focus in a brain abscess…
need to be examined by a cardiologist (including an echocardiogram), a dentist to rule out a dentogenic focus and an ENT specialist (with imaging of the mastoid process and sinuses)
40% of brain abscess cases are due to…
spread of an ENT infection
25% → invasion of bacteria from the blood stream, 10% → penetrating head trauma, 20% → no focus found
if it occurs due to metastasis of pus from elsewhere, its usually the lungs
most common microorganisms in brain abscesses are…
streptococci, staphylococci, E. coli and Proteus mirabilis
viral meningitis
fever, headache, nausea, NO neurological deficit, only a MILDLY stiff neck if any
can have a fairly acute course, typically resembling severe influenza
main pathogens in children = enterovirus, parechovirus, Coxsackie virus, and mumps virus
herpes simplex 2 can cause recurring viral meningitis
CSF → not much leukocytosis (they’re increased but not like bacterial), normal CSF protein and glucose levels, clear fluid
final diagnosis is usually based on PCR
virus remains unidentified in > ½
mumps meningitis is accompanied by parotitis in around ½
symptoms clear up within a few days to a maximum of 2 weeks, without specific treatment
most common causes of viral meningitis in children
enterovirus, parechovirus, Coxsackie virus, and mumps virus
viral vs bacterial meningitis?
viral has no neurological deficits and only has a mildly stiff neck if any
viral CSF → not much leukocytosis (they’re increased but not like bacterial), normal CSF protein and glucose levels, clear fluid