Lecture 13: Bone Injury and Healing
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Differentiate micro-damage and micro-fracture.
Microdamage = de-bonding
Microfracture = breaking of mineralized structures
Which occurs more often, micro-damage or micro-fracture?
Micro-damage
Micro-damage is more common in which type of bone?
Cortical bone
Micro-fracture is more common in which type of bone?
Trabecular bone
Minor damage of bone may occur at near ___% strain
Minor damage of bone may occur at near 0.8% strain
T/F: Bone can sustain high numbers of cracks and de-bonding before failing
True!
T/F: As loading increases, micro-damage increases
True
T/F: As cycles increase, more load is needed to reach failure
False!
Less load is needed to reach failure with more cycles
Discuss loading history and how it can cause deformation and fractures.
Isolated overloads that do not cause fracture of bone can cause subtle, cumulative, and permanent deformation resulting in clinical fractures years later
How does fracture occur differently with tensile and compressive loading?
Tensile: single crack initiation occurs at a threshold level followed by multiple cracks (crack propagation) and then a coalescence of cracks which happens at fracture
Compressive: single crack initiation occurs at a much higher load level followed by a sudden fracture of the structure
What are the aging effects on bone?
Progressive net loss of bone mass and a change in bone material properties (resulting in bone tissue of reduced strength and modulus)
Young bone is more ________ than older bone so more ______ before breakage is allowed in young bone.
Young bone is more ductile than older bone so more strain before breakage is allowed in young bone
Why is younger bone more ductile than older bone?
Water content
When is maximum bone present?
~3rd decade (slightly younger in females)
How is geometric remodeling affected by aging?
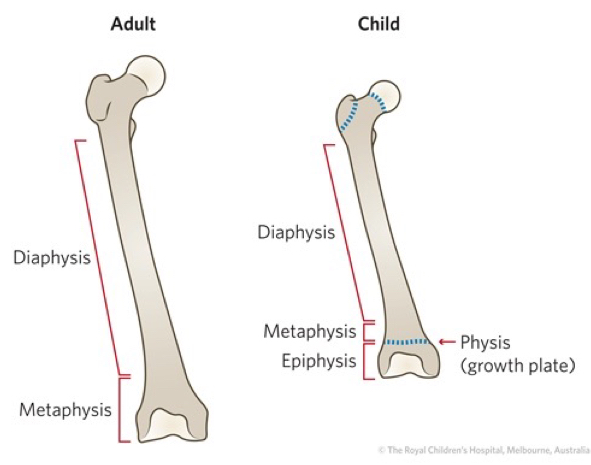
Cortex thins but the diaphysis becomes a cylinder of a larger diameter (as a mechanical compensation)
(Cortical areas remain almost constant in men, but they are decreased in women)
What contributes to degenerative joint disease?
Linked to failure of articular cartilage → shifts the load to the trabecular / subchondral bone → leads to more bone being laid down
How does compressive loading lead to degenerative joint disease?
Increased compressive loading → microfracture → bone remodeling → stiffening of subchondral bone → increased loading on already degenerated cartilage
T/F: Patients with osteoporosis are not as likely to get DJD.
Why or why not?
True!
Because osteoporotic bone is relatively soft and would act as a shock absorber
A joint with larger surface area relative to its load is (less/more) likely to develop DJD
A joint with larger surface area relative to its load is LESS LIKELY to develop DJD
OA in the knee is correlated with…
Body mass (especially in the medial compartment)
What are the pathomechanics of osteoporosis?
Osteoclasts continue to work but the osteoblasts become sluggish (result in greater bone resorption)
What is the best treatment of osteoporosis?
Exercise
Other options — drug cocktail of Ca2+, Vit D, and biphosphates
What medications can be used to treat pain for bone pathology?
Steroids — negatively affects bone density (may be okay for short term usage; ~ 7 days)
NSAIDS — not enough research to indicate negative impact on bone during fracture healing
What positive effects does regular exercise have on bone?
Positive effects on bone density, size, and most importantly shape
What is an important predictor of bone strength?
The location of increased bone mineral content/density (bone geometry)
Using the FITT Principle, how would you “strengthen bone?”
Frequency — at least 3x / week
Intensity — high impact exercises that produces large rates of deformation of bone matrix
Type — dynamic exercise (produces hydrostatic pressure changes on osteocytes which stimulates bone growth)
Time — short sessions (~ 20 -25 minutes) with longer rest breaks
For bone strengthening, is it better to increase the intensity, number, or time of the exercise session?
Better off increasing the intensity or number of sessions (rather than increasing the time of the exercise)
T/F: Vigorous exercise when you are a child and young adult can reduce your fracture risk later in life
True
After a reduction of bone mass (osteoporosis), what kind of effect can exercise have on bone mineral density?
Exercise can only have a moderate effect on BMD
Fracture risks may still be reduced (secondary to remodeling the geometry of the bone)
Balance training and postural stability will help with avoiding falls
Failure of bone due to tension loads is related to…
Debonding at the cement lines and pulling out of the osteon
What is the resulting fracture of a tension load?
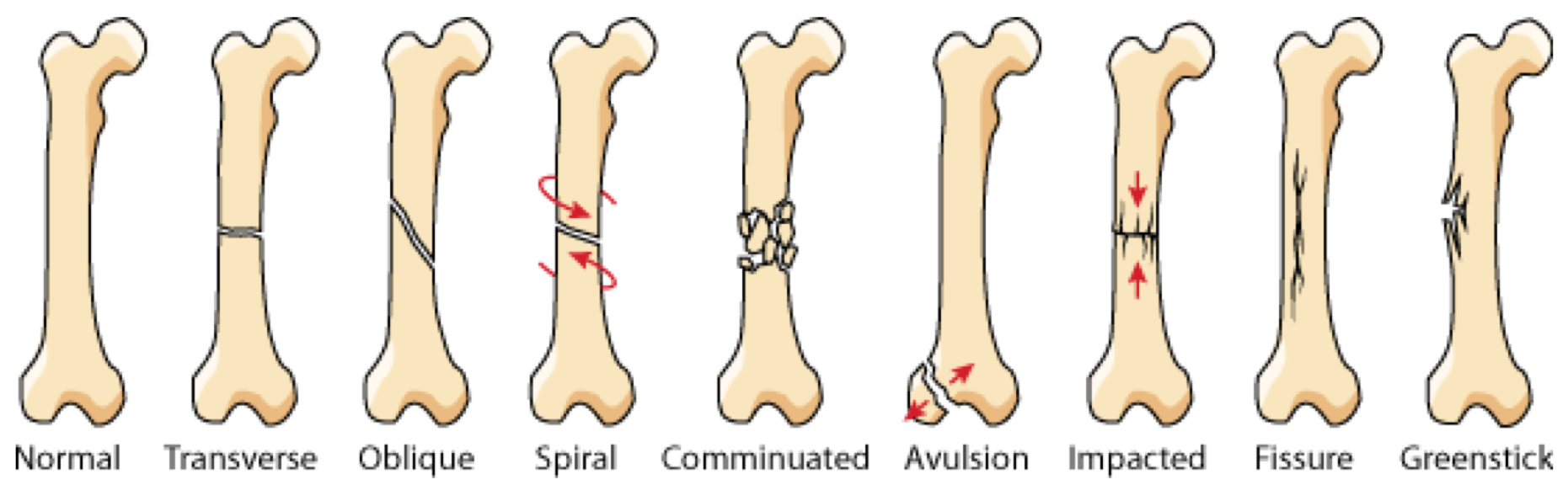
Transverse fracture
Where do pure tension fractures tend to occur?
Tends to occur in areas with large proportions of cancellous bone (e.g., calcaneus and base of 5th metatarsal)
Failure due to compressive loads is mainly seen as…
Oblique cracking of the osteons (~30 degree angle)
What is mostly responsible for fractures that occur due to compressive loads?
Shear forces that result from the compressive load
Where do compressive load fractures typically occur?
Mostly seen at the metaphysis where the cancellous bone is weaker (e.g., spondylolysis — vertebral fracture)
[However, few fractures occur in strictly compression mechanics]
Discuss the fracture mechanics of bone with bending loads
Bending loads cause compression and tension but these forces are not equal (since bone is not symmetrical)
Transverse fracture will start on the tension side (since bone is weaker in tension)
As the fracture propagates, the neutral axis shifts towards the compression side
Causes an oblique fracture on this side
When the cracks meet, a “butterfly” segment occurs
What is an example of a 3-pt bending fracture?
Ski boot fracture
In immature bone, bending loads cause what type of fracture?
Buckle fracture (where you see the tension side start to crack, but it never propagates all the way to the compressive side)
T/F: All loads will produce a shear load
Why or why not?
True
Bone is asymmetrical (therefore difficult to have pure compression, tension, or bending)
Shear loads tend to affect what type of bone?
Affects trabecular bone (more than cortical bone)
How does a torsion fracture occur?
Begins with failure in shear with the creation of a crack parallel to the neutral axis; then followed by failure in tension
(results in twisting about a neutral axis)
What type of fracture occurs from torsion?
Spiral fracture
What are the different types of fractures?
What do high rates of loading imply regarding bone fractures?
Higher rates of loading imply that more energy is stored quickly within the bone prior to failure
When failure occurs this energy is released instantaneously which can lead to comminuted fractures
T/F: Comminuted fractures are possible with higher loads
True
How do fatigue fracture (aka stress fractures) occur?
Repeated cycles of sub-failure load
Can occur from a high load repeated a few times or a low load repeated many times
T/F: Fatigue fractures (stress fractures) can be complete fractures
False
Through the cortex only — not complete fractures
How does frequency affect the likelihood of stress fractures? Why?
As frequency of the load increases the likelihood of stress fracture increases
If loading occurs too frequently then there is no time for remodeling to occur
How can muscle fatigue potentially lead to stress fractures?
If a muscle is fatigued, it can affect their ability to transmit loads; this results in more load being transmitted to the bone (and the bone cannot sustain it)
What are the phases of healing for a bone fracture?
Inflammation
Initial Union
Remodeling of Callus
What occurs during the inflammation phase of fracture healing?
Hematoma around fx site within 3 days
Mesenchymal cells produce fibrous tissue (to surround broken ends)
Injured tissue and platelets release vasoactive mediators
Growth factors and other cytokines are released
Influences cell migration, proliferation, differentiation, and matrix synthesis
Macrophages, PMNs, and mast cells begin process of removing debris
When does the inflammatory phase of fracture healing occur?
Occurs from the time of injury to 24-72 hours
What occurs during the initial union (reparative response) phase of fracture healing?
Vasoactive substances cause neovascularization and local vasodilation
Undifferentiated mesenchymal cells migrate to fx site (have ability to form cartilage, bone, fibrous tissue, etc.)
Hematoma is organized; fibroblasts and chondroblasts appear between the bone ends
Cartilage is formed (type III collagen)
How does the stability of the fracture impact the following stages of healing?
Stable Fracture — fibrous tissue is vascularized
Osteoblasts form bone along the periosteal surface of the fibrous layer and bridge the fracture site
Unstable Fracture — fibrous tissue is non-vascularized
New bone is formed along the periosteal surface, but it does not bridge the fracture line
When does the initial union phase occur?
From 2 days to 2 weeks
During the initial union phase the amount of callus formed is ________ proportional to the amount of immobilization of the fracture
During the initial union phase, the amount of callus formed is inversely proportional to the amount of immobilization of the fracture
T/F: In fractures that are fixed with rigid compression plates, there can be primary bone healing with little or no visible callus formation
True
When does the remodeling phase of fracture healing occur?
Middle of repair phase and up to 7 years
During the remodeling phase of fracture healing, the remodeling of woven bone is dependent on what?
Dependent on the mechanical force applied
When is fracture healing complete?
When there is repopulation of the medullary canal
How does remodeling occur in cortical bone (from fracture)?
Occurs by invasion of osteoclasts (to “cut down the bone”) which is then followed by osteoblasts to lay down new lamellar bone (osteon)
How does remodeling occur in trabecular bone (from fracture)?
Occurs on the surface of the trabeculae which causes it to become thicker
T/F: More than one process/phase of healing can occur at any given time
True
Usually just one process dominates and therefore it is labeled as that phase
What are some systemic factors that could influence fracture healing?
Age
Hormones
Functional activity
Nerve function
Nutrition
Drugs (cortisone = decreased callus production)
Pathologies (e.g., diabetes)
What are some local factors that could influence fracture healing?
Degree of trauma (e.g., injury to surrounding soft tissue)
Degree of bone loss
Vascular injury
Type of bone fractured
Degree of immobilization
Infection
Local pathologic condition
What is the interfragmentary strain hypothesis?
States that the type of tissue formed in a healing gap depends on the strain that it experiences
Strain is between 10-100% → granulation tissue can be expected to form
Strain between 2-10% → fibrocartilage will form
Strain <2% → bone will form
0% Strain → result in no growth
Using the inferfragmentary strain hypothesis, if the gap had movement of 0.5 mm (16% strain) what would occur to the bone mineral density?
Increased bone mineral density
Using the inferfragmentary strain hypothesis, if the gap had movement of 2.0 mm (66% strain) what would occur to the bone mineral density?
Decreased bone mineral density
T/F: Considering the interfragmentary strain hypothesis, the mecahnism of loading is not important regarding bone healing (e.g., tensile or compressive), but what is important is the strain produced
True (change in length is important)
What are the goals for fracture treatments?
Successful reduction of fracture
Provide good stability, rapid healing, and minimization of any subsequent deformity
Prevent malunion