CLINMIC LEC LAB SAFETY, INTRO TO URINALYSIS, RENAL FUNCTION
1/192
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
193 Terms
Universal precautions
All patients are considered to be possible carriers of blood-borne pathogens
Recommends wearing gloves when collecting and handling blood and body fluids contaminated with blood and wearing face shields when there is danger of blood splashing on mucous membranes and when disposing of all needles and sharp objects in puncture-resistant containers
Exclude urine and body fluids not visibly contaminated by blood from UP
Body substance isolation
Considered all body fluids and moist body substances to be potentially infectious
Personnel should wear gloves at all times when encountering moist body substances
Do not recommend handwashing following removal of gloves unless visual contamination is present
Standard precautions
Combined the major features of UP and BSI
Placed emphasis on patient contact. These are the principles most certainly can also be applied to handling patient specimens
Universal precautions
Handling and storage of specimen should follow what?
Biologic hazard
Source: infectious agents
Possible injury: Bacterial, fungal, viral or parasitic infections

Sharps hazard
Source: needles, lancets, broken glass
Possible injury: Cuts, punctures, blood-borne pathogen exposure
Chemical hazards
Source: Preservatives and reagents
Possible injury: Exposure to toxic, carcinogenic or caustic agents

Radioactive hazard
Source: Equipment and radioisotopes
Possible injury: Radiation exposure
This hazard cannot cause immediate harm

Electrical hazard
Source: Ungrounded or wet equipment, worn cords
Possible injury: Burns or shock

Fire/Explosive
Source: Open flames, organic chemical
Possible injury: Burns or dismemberment
Physical hazards
Source: Wet floors, heavy boxes, patients
Possible injury: Falls, sprains or strains

Ergonomic hazards
Hazards regarding posture
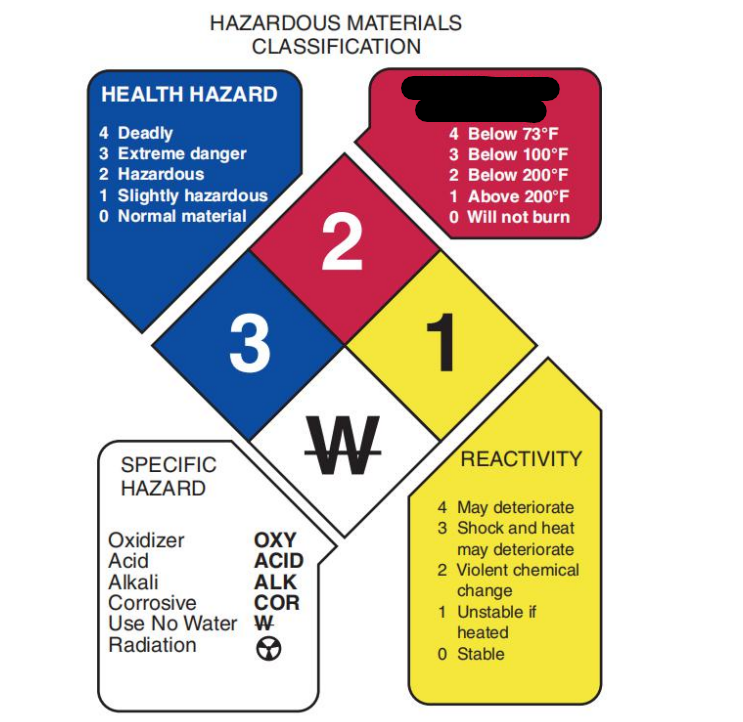
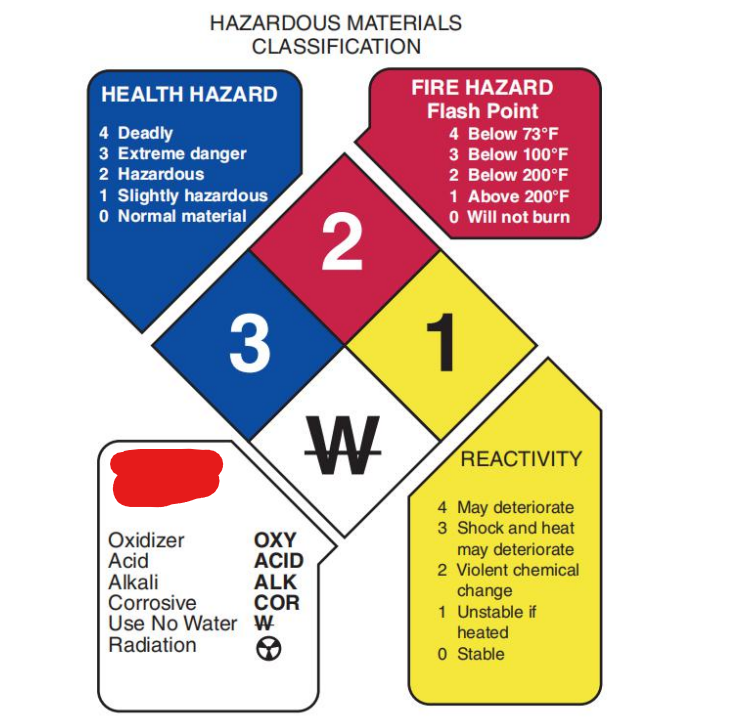
Reactivity
Yellow quadrant of the NFPA hazardous materials classification
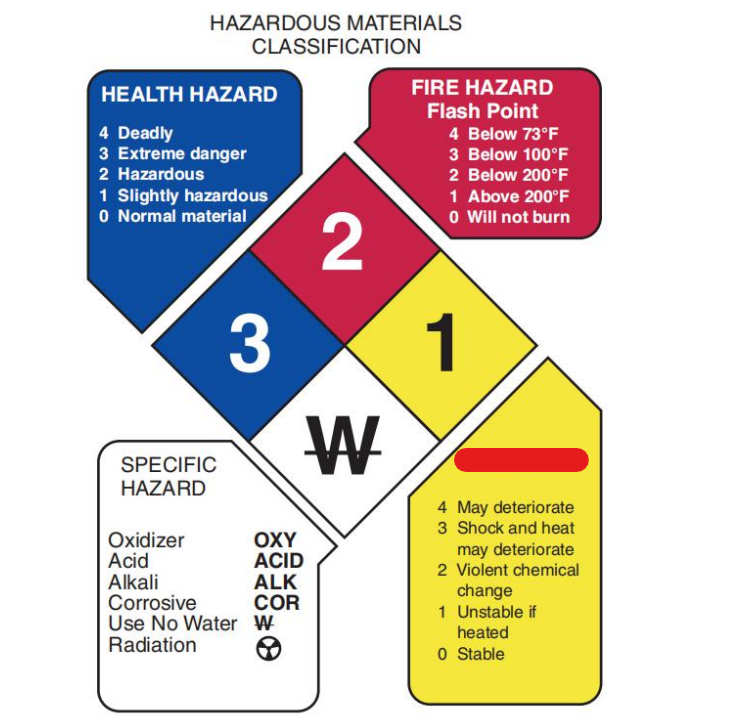
Fire hazard
Red quadrant of the NFPA hazardous materials classification
Flammables
< 37.8 degrees C
Combustibles
>37.8 degrees C
Health hazard
Blue quadrant of the NFPA hazardous materials classification
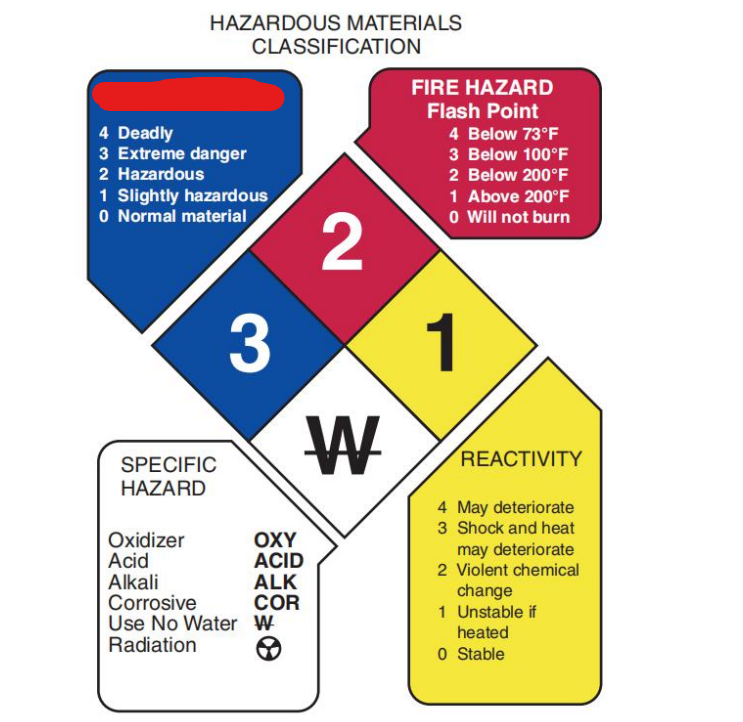
Specific hazard
White quadrant of the NFPA hazardous materials classification
Flush the area with large amount of water for 15 minutes, then seek medical attention.
Remove contaminated clothing as soon as possible.
No attempt should be made to neutralize chemicals that come in contact with the skin.
What to do in case of a chemical spill? (3) (FRN)
Acid to water
What is proper procedure when mixing acid and water?
30-50 gallons of water per minute
20-50 psi
Safety showers should be able to release how much gallons of water per minute and at what pressure?
100 feet per 10 seconds travel time
Eye wash stations should accessible at an area within?
Explosion proof refrigerators
Where are flammables stored in?
Physical and chemical characteristics
Fire and explosion potential
Reactivity potential
Health hazards and emergency aid procedures
Methods for safe handling and disposal
What does the MSDS contain? (5)
Appropriate work practices
Standard operating procedures
PPE
Engineering controls (fume hoods, fire safety cabinets)
Employee training requirements
Medical consultation guidelines
What does the chemical hygiene plan entail? (6)
Pathogen
Reservoir
Portal of exit
Mode of transmission
Portal of entry
Susceptible host
6 parts of a chain of infection
Wet hands with warm water
Apply antimicrobial soap
Rub to form a lather, create friction and loosen debris
Thoroughly clean between fingers, including thumbs, under fingernails and rings, and up to the wrist for at least 15-20 seconds (MOST CRUCIAL PART)
Rinse hands in a downward position
Dry with a paper towel
Turn off faucets with a clean paper towel to prevent recontamination
Proper hand hygiene (7 steps)
Disposable towels
Best way of drying the hands is thru using?
Thoroughly clean between fingers, including thumbs, under fingernails and rings, and up to the wrist for at least 15-20 seconds
What is the most crucial part in handwashing?
60 seconds
Entire duration of handwashing?
Gown
Mask or respirator
Goggles or face shield
Gloves
Donning steps (GowMaGogGlo)
Inner gloves
In double gloving technique, what is the first step in donning?
Gloves
Goggles or face shield
Gown
Doffing steps (3) (GloGogGow)
Rescue
Activate alarm
Contain
Extinguish/Evacuate
What to do in case of fire? RACE
Evacuate
What does “E” stand for in RACE when it comes to arsenal fires/detonating agent?
Pull the pin
Aim at the base of the fire
Squeeze the nozzle
Sweep side to side
How to use the fire extinguisher? (PASS)
Urine
All biological wastes except _________ must be placed in an appropriate container labeled as biohazard
Pouring it into the sink
Urine may be discarded by ________________ avoiding splashing and flushing it with water.
1:5 (20%)
1:10 (10%)
2 dilutions of sodium hypochlorite that can be used in daily disinfection of the sink
1 month
Sodium hypochlorite solutions are stable for how many months if protected from light after preparation?
Class A
What fire type? (a ASH, when these materials are burned they turn to ash)
Wood, paper, clothing
Water
Extinguisher for Class A fires?
Class B
What fire type?
Flammable organic materials
Dry chemical
CO2
Foam
Halon
Extinguishers for Class B fires (DCFH)
Class C
What fire type?
Electrical
Dry chemical
Carbon dioxide
Halon
Extinguishers for Class C (DCH)
Class D
What fire type?
Combustible materials (Mg, Na, K)
Dry chemicals
Most commonly used fire extinguisher?
Class K
What fire type?
Grease, oil, fats
Liquid designed to prevent splashing and cool the fire
Extinguisher for class K?
Monthly
When should fire extinguishers be inspected?
Frederik Dekkers
discovered albuminuria in 1694 by boiling urine
Thomas Bryant
wrote about a book about “pisse prophets”; inspired the passing of the first medical licensure laws in England
Thomas Addis
developed the first method of quantitative urine microscopic examination
Henry Bence-Jones
father of CC
95% Water and 5% solutes
Urine is how many percent water and how many percent solutes?
Urea
Creatinine
Uric acid
Hippuric acid
Organic components of the urine (UCUH) (4)
Urea
Primary organic component
Creatinine
product of creatine metabolism
Uric acid
product of nucleic acid breakdown
Hippuric acid
excretion form of benzoic acid
Ammonium
Chloride
Calcium
Sodium
Potassium
Phosphate
6 inorganic components of the urine (ACCSPP)
Chloride
Primary inorganic component
SODIUM
Primarily from salt intake
POTASSIUM
Combined with chloride and other salts
PHOSPHATE
Combines with sodium; buffers the blood
AMMONIUM
Regulates blood and tissue fluid acidity
CALCIUM
Combines with chloride, sulfate, phosphate
Clean, dry, leak-proof, wide-mouthed, flat bottom, must be made from clear material
50mL
Characteristics of urine containers
Labels
Must include patient’s name and identification number, date and time of collection
– Additional information such as patient’s age and location, physician’s name
– Must be attached not on the lid
– Should not be detached when specimen is refrigerated or frozen
Requisition form
– Must accompany the specimen when delivered to the laboratory
– The information on this form must match the specimen label
– Additional information can include method of collection, type of specimen, medications, clinical information
– The time the specimen is received should be recorded on the form
Specimens in unlabeled containers
Nonmatching labels and requisition forms
Specimens contaminated with feces or toilet paper
Containers with contaminated exteriors
Specimens of insufficient quantity
Specimens that have been improperly transported
NOTE: Never discard any specimen without consulting with the chief.
6 instances where in specimen is rejected
2 hours
Following collection specimens should be delivered in the laboratory promptly and tested within how many hours?
2-8 degrees Celcius
The most routinely used method of preservation or refrigeration is at what temperature?
Room temperature
Specimens must be returned to what temperature before chemical testing by reagent strips because the enzyme reactions on the strips perform best at room temperature?
24 hours
Specimens for culture should be refrigerated on transport and kept refrigerated until culture for up to how many hours?
pH
Bacteria
Odor
Nitrite
Color
What analytes will increase if urine is unpreserved? (pBaON)
Glucose
Most affected analyte in unpreserved urine?
Protein
Least affected analyte in unpreserved urine?
Refrigeration
Most routinely used method of preservation; does not interfere with chemical tests
Disadvantage: precipitates amorphous phosphates and urates
Prevents bacterial growth for 24 hours
Boric acid
URINE PRESERVATIVES
Prevents bacterial growth and metabolism
Disadvantage: Interferes with drug and hormone analysis
Keeps pH at about 6.0: can be used for urine culture transport
Formalin
URINE PRESERVATIVES
Excellent sediment preservative
Disadvantage: Acts as a reducing agent interfering with chemical tests for glucose, blood, leukocyte esterase and copper reduction
Rinse specimen container with formalin to preserve cells and casts
Sodium fluoride
URINE PRESERVATIVES
A good preservative for drug analysis
Inhibits reagent strip glucose, blood, and leukocytes
Phenol
URINE PRESERVATIVES
Advantage: Does not interfere with routine tests
causes an odor change
● Use 1 drop per ounce of specimen
Thymol
URINE PRESERVATIVES
Preserves glucose and sediments well
Interferes with acid precipitation test for protein
Toluene
URINE PRESERVATIVES
Floats on the surface of the specimen and clings to pipettes and testing materials
Saccomano’s fixative
URINE PRESERVATIVES
50% ethanol + 2% carbowax
Preserves cellular elements; used for cytological studies
Formalin
What is the 2nd best choice used in cytological studies next to Saccomano’s fixative? (If Saccomano’s fixative isn’t in the choices)
Concentrated HCl
URINE PRESERVATIVES
10 mL of 6N HCl + 3-4 L container
Catecholamines (epinephrine, VMA, 5 HIAA)
Hydrochloric acid
Glacial acetic acid
Boric acid
URINE PRESERVATIVES
Quantitative analysis of steroids, hormones (HGB)
Boric acid at 1g/dL
URINE PRESERVATIVES
Estriol and estrogen for up to 7 days
Random specimen
TYPES OF URINE SPECIMEN
Most commonly received specimen
Useful for routine screening tests to detect obvious abnormalities
First morning specimen
TYPES OF URINE SPECIMEN
Ideal morning specimen; most concentrated
'Prevention of false-negative pregnancy test and evaluation of orthostatic proteinuria
Timed specimen
TYPES OF URINE SPECIMEN
Quantitative chemical tests
Measurement of analytes exhibiting diurnal variations
50mL
Volume of aliquot used in urinalysis
Catheterized specimen
TYPES OF URINE SPECIMEN
Collected under sterile conditions by passing a hollow tube through the urethra into the bladder
Midstream clean-catch
TYPES OF URINE SPECIMEN
Provides a safer and less traumatic method of obtaining urine for culture
Alternative to catheterized specimen
Suprapubic aspirate
TYPES OF URINE SPECIMEN
Preferred sample for bacterial culture and cytological examination
Pediatric specimen
TYPES OF URINE SPECIMEN
Done using soft, clear, plastic bags with hypoallergenic skin adhesive to attach to the genital areas
Bag is checked every 15 minutes until the needed amount of sample has been collected
Drug testing specimen
TYPES OF URINE SPECIMEN
Collection and handling of specimen must follow the chain of custody
Urine volume: 30-45 mL
Container volume: 60 mL
Urine temperature: 32.5 to 37.7 degree Celsius tested within 4 minutes after collection