Chapter 9 Inflammation & Dysfunctional Wound Healing
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Complications of Wound Healing
Keloid Formation
Contractures
Dehiscence
Evisceration
Stricture
Fistula
Adhesions
Kites Catch Drift Easily, Soaring Far Above
Complications of Wound Healing:
Keloid Formation
Excessive collagen causes thick scar tissue.
Complications of Wound Healing:
Contractures
Excessive tightening of tissue leads to limited movement.
Complications of Wound Healing:
Dehiscence
Wound reopens after partial healing.
Complications of Wound Healing:
Evisceration
Internal organs protrude through a wound.
Complications of Wound Healing:
Stricture
Narrowing of a tubular structure (e.g., esophagus).
Complications of Wound Healing:
Fistula
Abnormal connection between organs or tissues.
Complications of Wound Healing:
Adhesions
Bands of scar tissue form, connecting tissues that shouldn’t be connected.
Pathophysiology of Fever
Releases pyrogens (substances that cause fever, i.e. cytokines, microbial organisms, etc.)
Causes hypothalamus to raise body’s temperature set point
Risks of Fever
Can lead to febrile seizures in children
Dehydration
Excessive tissue damage in prolonged fever
Medications That Reduce Fever
Aspirin
NEVER GIVE CHILDREN ASPIRIN FOR FEVER
Ibuprofen (Tylenol)
Acetaminophen (Advil, Motrin)
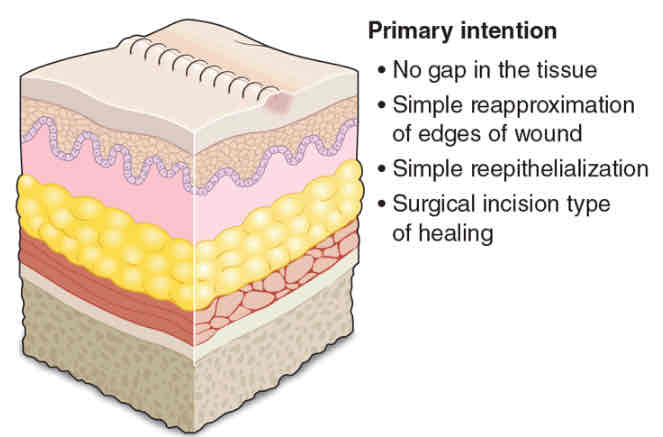
Primary Intention
Cleanly lacerated, clear wound edges, and easily brought together
e.g., surgical incision
Minimal scarring; easy healing
Simple epithelialization
Within 5 days (granulation tissue)
Within 30 days (CT covered by an intact epidermis)
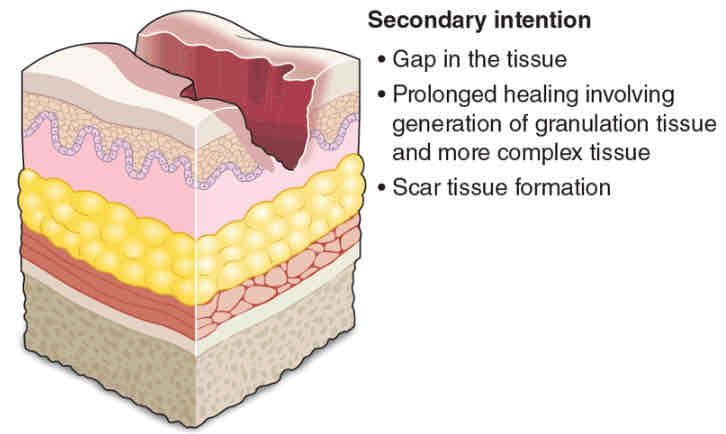
Secondary Intention
Abundant granulation and fibrotic tissue formation
To replace and restore structure of tissue
Regeneration takes longer; needs new tissue
Myofibroblasts
CT cells that cause contraction
Increased risk for scarring
Highly susceptible to
Infection
Complications
Deformity
NOTE:
Regeneration of same cells to replace lost tissue is NOT possible
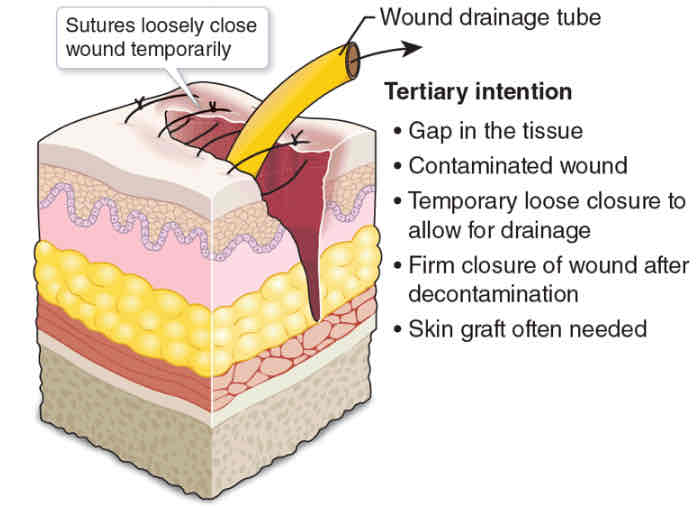
Tertiary Intention
Missing large amounts of deep tissue
Delayed closure due to infection or other factors
Cleaned and left open (4-5 days)
Pack with sterile gauze
5th day
Phagocytosis of contaminated tissue
Epithelialization
Collagen deposition
Maturation
Prominent scarring
Skin graft needed
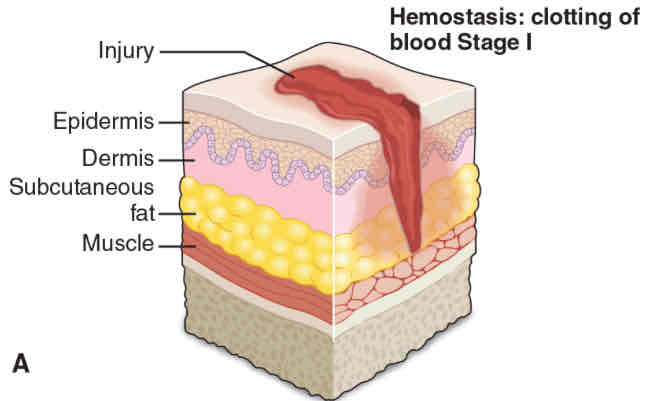
Four Phases of Wounding Healing
Hemostasis
Inflammatory Phase
Proliferation Phase
Maturation/Remodling Phase
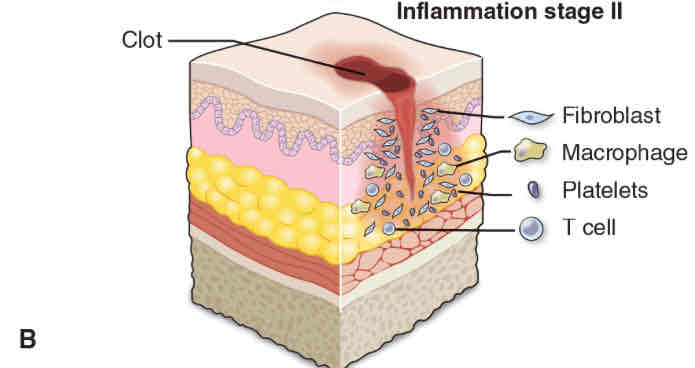
Hemostasis
Exposed collagen of injury
Attracts platelets
Platelets aggregate
To secrete inflammatory mediators
Vasoactive amines
Cause short-term vasoconstriction
Inflammatory Phase
WBCs clear debris and fight infection
Vasodilation, increased vascular permeability, & chemotaxis
5 Cardinal Signs of Inflammation
Redness (Rubor)
Heat (Calor)
Swelling (Tumor)
Pain (Dolor)
Loss of function (Functio laesa)
(Should review acute and chronic inflammation later)
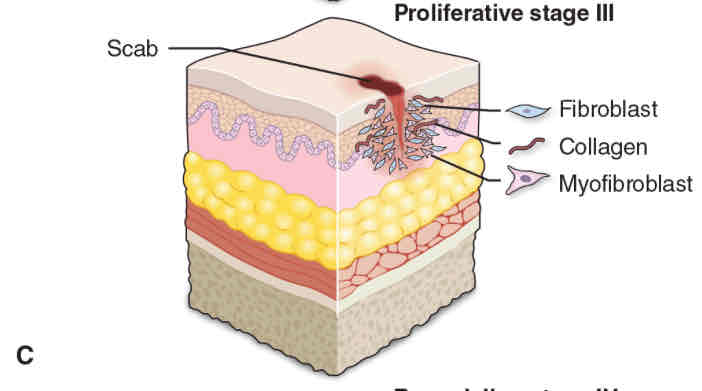
Proliferation Phase
Fibroblasts (a CT tissue)
Synthesizes collagen
24 - 48 hrs, forms granulation tissue for foundation of scar tissue
Wound contraction (due to shortening of fibroblasts)
Creation of new BV (Angiogenesis)
Granulation tissue Secretes VEGF (vascular endothelial growth factor)
Epithelial cells (Epithelialization)
Migrate and proliferate to fill wound gap
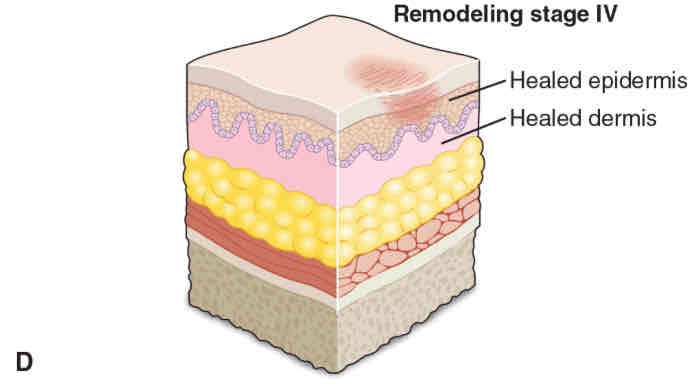
Maturation/Remodeling Phase
Scar tissue is structurally refined and reshaped by fibroblasts and myoblasts
Takes ~3 weeks after injury to start remodeling
Factors That Affect Wound Healing
Nutrition: + nitrogen balance (vitamins also)
Oxygen: Facilitates collagen synthesis and WBC function
Circulation: Helps remove waste
Immune strength: Stronger immune system = better
Infection: Single most significant factor in delayed wound healing
Foreign bodies: Debris in wound
Mechanical factors: Torsion, localized pressure, mechanical stress
Make sure to reposition every 2 hours
Age: Older adults having slowest healing process
“Never Overlook Clever Ideas If Fun Moments Arise”
What Stimulates Histamine Release
Physical injury
Immune reactions
Cytokines
Other inflammatory mediators
Histamine is Produced by
Basophils
Platelets
Mast cells (richest source)
Systemic Effects of Histamine
Arteriolar vasodilation
Large artery vasoconstriction
Increased permeability of venules
Ex. Responses if histamine released in upper respiratory tract)
Sneezing
Runny nose
Pharyngeal irritation
COX-1 Prostaglandins Pathway
Breaks down arachidonic acid enzymatically into helpful PGs
Stimulate gastric mucus production
To protect gastric mucosa
Enhance renal perfusion
Assist platelets to aggregate and form clots
(thrombus formation)
COX-2 Prostaglandin Pathway
Yields harmful PGs
Perpetuate inflammation
Causing
Pain
Fever
Swelling
Muscle contractions
Potentiate effects of other inflammatory mediators