SSS Week 3
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
Herpes Simplex Virus infection (types, recurrence, complications, diagnosis, treatment
clinical sign: grouped vesicles on an erythematous base
spread via resp droplets or direct contact with an infected lesion or bodily fluids
HSV enters host through abraded skin or intact mucous membranes
targets epithelial cells initially but retrograde transport through adjacent neural tissue to sensory ganglia leads to lifelong latent infection
two types: HSV1 and HSV2
HSV1 is more associated with oral n facial infections (cold sores)
often initial episode has no symptoms but can be severe if have systemic symptoms
vesicles turn quickly into ulcers (red based)
HSV2 more associated with anogenital herpes
presents after onset of sexual activity
painful vesicles, ulcers, redness and swelling last for 2-3 weeks, often accompanied by fever and tender inguinal lymphadenopathy
minor injury helps inoculate HSV into skin
How can HSV recur
can either be local or systemic stimuli
UV light
fever
trauma
mensturation
sexual intercourse
stress
immunodeficiency
recurrence is often less severe
Complications
eye infection: dendritic ulcer
throat infection
eczema herpeticum (in patients with history of atopic dermatitis or darier disease)
erythema multiforme (target lesions, symmetrical plaques on hands, forearms, feet and lower legs)
cranial/facial nerve infections by HSV (bells palsy)
widespread infection —> disseminated infection (eg. can occur in a HIV patient)
Diagnosis
clinical diagnosis, culture and PCR
treatment
mild uncomplicated eruptions of herpes simplex require no treatment
sunscreen and other sun protection measures are crucial as sun exposure often triggers facial herpes simplex
for mild oral lesions: topical acyclovir
severe infection may require treatment with an oral antiviral agent
acyclovir
valaciclovir
famciclovir
theyre suppressive not curative
How can HSV recur
can either be local or systemic stimuli
UV light
fever
trauma
mensturation
sexual intercourse
stress
immunodeficiency
recurrence is often less severe
Diagnosis for HSV
Clinical diagnosis, culture, PCR
Treatment for HSV
mild uncomplicated eruptions of herpes simplex require no treatment
sunscreen and other sun protection measures are crucial as sun exposure often triggers facial herpes simplex
for mild oral lesions: topical acyclovir
severe infection may require treatment with an oral antiviral agent
acyclovir
valaciclovir
famciclovir
theyre suppressive not curative
Varicella (chickenpox) (rash, lesion characteristics, diagnosis, complications, treatment, vax?)
caused by varicella-zoster virus
remains in dorsal ganglia of the spinal cord —> can reappear later as shingles or herpes zoster infection
spread via inhalation of resp droplets or direct contact with the vesicles’ fluid.
RASH: begins on trunk and spreads to face and extremities (the opposite of rubella and measles)
LESIONS are: 2-4mm red papules —> become vesicular and umbilicated —> breaks and crusts over leaving an eroded red base
diagnosis
made clinically in typical cases
can be confirmed by PCR on a viral swab from base of vesicle
complications
secondary bacterial infection from scratching
dehydration from vomiting and diarrhoea
systemic:
~ viral pneumonia
~ encephalitis
~ thrombocytopenia
~ hepatitis
~ scarring
pregnancy complications
• If a non-immune pregnant woman is infected:
◦ Maternal varicella pneumonia (serious).
◦ Congenital varicella syndrome (limb hypoplasia, eye/brain defects, skin scarring in fetus).
◦ Severe neonatal varicella if infection occurs just before or after delivery.
treatment
symptomatic eg. antipruritis lotions, antihistamines?
antiviral therapy is indicated for patients with complications or who are immunocompromised
antiviral agents include acyclovir, valacyclovir, famciclovir (same as HSV)
varicella-zoster immune globulin (VZIG) is indicated for immunocompromised and neonates exposed to varicella (must be given within 96 hours of exposure)
vaccination
immunisation schedule in australia for infants aged 18 months and children 10-13 years who have not been previously immunised or previously had varicella infection
zoster vax has also been introduced for patients over 60 and who are most at risk of this condition
Herpes Zoster (shingles) +diagnosis, clinical features, treatment
reactivation of varicella virus localised to one or two dermatomes (what ur auntie had)
virus remains in selected ?anterior? horn cells of spinal cord before it is reactivated and grows down the nerves to the skin
predisposing factors apart from age are immunocompromised individuals eg. HIV
Diagnosis
clinical
viral PCR for herpes zoster virus
clinical features
unitlateral
dermatome (one or several)
first sign of shingles is usually pain, which may be severe, in areas of one or more sensory nerves. the patient may appear quite unwell with fever and headache, lymph nodes draining the affected area are often enlarged and tender
pain —> closely grouped lesions start as erythematous papules or plaques —> turn vesicular and become crusted —>over a course of 2-3 weeks clear vesicles appear in the affected dermatome
complications
post-herpetic neuralgia (can last for years)
corneal damage if CN V involved
encephalitis
myelitis causing contralateral hemiplegia
*Hutchinson’s sign - vesicle on side or tip of nose in ophthalmic zoster (WHAT UR AUNTIE HAD)
treatment
antiviral medication within 72 hours
analgesia
vaccination for patients over 60
Viral exanthem
rash due to a virus
can be divided into
classic eg. measles rubella
non-specific (in children usually enteroviridae (coxsackie or echovirus))
whereas there are specific presentations with varicella, measles, rubella, hand, foot and mouth disease, parvovirus (slapped cheek), roseola, pityriasis rosea
What are the two non-specific presentations of viral exanthem in children
generalised, bilaterally symmetrical maculopapular rashes, often with confluence on the face
peripheral papular eruptions mainly on arms and leg
Measles (clinical presentation, diagnosis, complications)
spread via resp droplets
clin presentation
initially URTI symptoms of fever, malaise, cough and conjunctivitis
characteristic KOPLIK spots (pinhead size white spots on buccal mucosa) in prodromal stage —> a widespread morbilliform (macular) rash appears HEAD then spreads to TRUNK and limbs
non-pruritis rash
macules may coalesce, esp on face
when it fades —> purplish hue —> brown/coppery coloured lesions with fine scales
diagnosis
clinical n confirm with serology
complications (Did this in GH)
diarrhoea
otitis media
pneumonia
encephalitis
vax at 12 months of age
*notifiable disease
Rubella (german measles) = presentation, diagnosis, complications
mild pink maculopapular rash and lymphadenopathy
begins on FACE and spread to TRUNK and limbs (less widespread than measles)
mild fever, sore throat and rhinitis
adults have arthralgia and arthritis
infected by direct contact with nasal or throat secretions of infected individuals, infected personcontagious 7 days prior to rash, until 7 days after
diagnosis
clin and confirm with serology (same as measles)
complications
first trimester of pregnancy has 50% risk of congenital rubella syndrome (sensorineural deafness, CNS dysfunction, cataracts, cardiac defects)
*notifiable disease (like measles)
rubella vax is on national schedule
Hand, foot and mouth disease (clin presentation + DDx + diagnosis)
most often affecting young children under 5
due to coxsackie virus A16
children present with small red macules that rapidly evolve into cloud vesicles and surrounded by erythematous areola in the oral cavity
there may be lesions distributed over plams and soles, and dorsal fingers or toes
20% of cases have submandibular / cervical lymphadenopathy
DDx for hand, foot and mouth disease
enterovirus 71 infection
herpetic stomatitis
aphthous ulceration
herpangina
erythema multiforme
scabies
(see the ppt for explanation on ddx)
diagnosis
clin and serology (same as measles and german measles (rubella))
DDx for hand, foot and mouth disease
enterovirus 71 infection
herpetic stomatitis
aphthous ulceration
herpangina
erythema multiforme
scabies
(see the ppt for explanation on ddx)
Parvovirus infection - slapped cheek - fifth disease (clin features, treatment, complications, DDx)
parvovirus B19
transmitted via resp droplets
clin features
firm red burning-hot cheeks
rash follows with lace or network pattern on limbs and then trunk

treatment - supportive
complications
in pregnant women may cause foetal anemia and cardiac failure and fetal loss
arthralgia in adults
DDx
enterovirus exanthemata
rubella
scarlet fever
Roseola (clin presentation and treatment?)
transmitted via resp droplets
HHV-6B, HHV-7
clinical presentation
high fever and upper resp symptoms
rash appears as fever subsides (days 3-5)
rash: small pink or red maculopapular rash that blanch when touched, may be surrounded by lighter halo of pale skin
begins on TRUNK and may spread to neck, face, arms and legs (sort of like varicella)
non-itchy, painless and does not blister
no treatment required
Pityriasis Rosea (presentation)
rash of unknown cause (possible reactivation of Herpes 7 or 8 virus)
most commonly affects teenagers or young adults
PRESENTATION
single inner circlet of scaling, oval red or pink plaque (the HERALD patch) appears before general rash
few days later, smaller plaques appear on chest n back, uncommon on face
these lesions follow the relaxed skin tension lines (LANGER’S LINES) on both sides of upper trunk (so it looks like a fir tree?)
can be very itchy and sometimes not at all. on darker skin they appear more pigmented or white due to scales

Monkey pox (MPox) - presentation, transmission, prevention, diagnosis, treatment and vax
viral zoonotic disease
presentation
general symptoms (fever, chills, headache, muscle aches, back aches, fatigue, swollen lymph nodes)
USUAL symptoms: rashes, pimple-like lesions or sores, particularly in areas like genitals, anus or buttocks…. ulcers, lesions or sores in mouth… rectal pain (with or without rash)
all lesions go crusted and fall off to reveal a fresh layer of skin
most people with MPox get better within a few weeks without needing any specific treatment
Mpox spread via
direct contact w rashes, blisters or sores, or contact w bodily fluids also
TOUCHING contaminated objects
who is at risk: men who have sex w men
prevention
isolation
hand hygiene
keeping lesions covered and wear a face mask
diagnosis
by lab testing
treatment
supportive care —> pain relief
antivirals for more severe disease
vaccine for at risk population!

Molluscum contagiosum - presentation, DDx, control spread, treatment
poxvirus
two peaks: in children (3-9) and young adults
spread from direct contact
the papules form a row —> known as pseudokoebnerised molluscum
presents as clusters of small pearly papules with a central umbilication, core can be expressed by firm pressure, occurs in warm moist areas like armpits, groin or behind knees in kids, in adults in groin
DDx
verrucae (but have no central umbilication)
herpes (rapid onset and vesicles)
treatment
in children leave alone
cryotherapy
can use tape occlusion
immune techniques such as imiquimod creme, topical retinoids
Viral warts - transmission, presentation, DDx, treatment
common benign growths
usually on hands, feet and extensor surfaces
HPV
transmission
direct contact w infected skin or contaminated surfaces (breaks in skin increase transmission)
presentation
comon warts (verruca vulgaris)
plane warts
plantar warts
digitate/filiform warts
characterised by papillomatous surace, loss of skin lines and papillary capillaries
DDx
Bowen’s disease
seborrheic keratosis
corns and callous
penile pearly papules and equivalent papillomatosis of vulva
treatment
spontaneous resolution usually 2 years
topical salicylic acid, podophyllin or cryotherapy
imiquimod topical treatment
specialist referral if conservative fail
HV vax
reason we see viral warts as doctors
cosmetic
teasing from school mates
exclusion from sport
increasing number of warts
pain in weight bearing
distortion of structure
concern of diagnosis
Scabies * presentation, diagnosis, complications, treatment
scarcoptes sscabiei hominus
transmitted by body-to-body contact
burrow through strateum corneum, produce 2-3 eggs a day which mature in 2-3 weeks
presentation
variable due to allergic reaction which is dependent on individual
generalised eruption and itchiness is thought to be caused by sensitisation to their products eg. faeces and eggs
pruritic excoriated nonspecific rash on trunk with scaly burrows on fingers and wrists
papular or nodular lesions are often seen on genitals and nipples in adults and major flexor surfaces of children
in infancy, rash on face
diagnosis
confirm with scrapping from burror and examine under microscope
dermoscopy sometimes helps
pracical method is positive response to anti-scabicide
complications
secondary bacterial infection, rarely glomerulonepritis or RHD
crusted scabies —> more on this
treatment
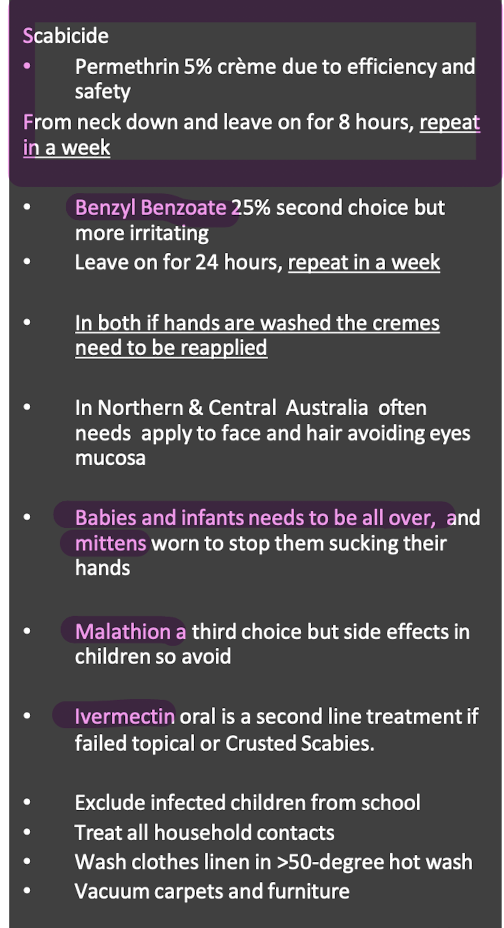
What are crusted scabies
severe variant of scabies
often seen in immunosuppressed
numerous more mites
widespread, scaly and hyperkeratotic rash
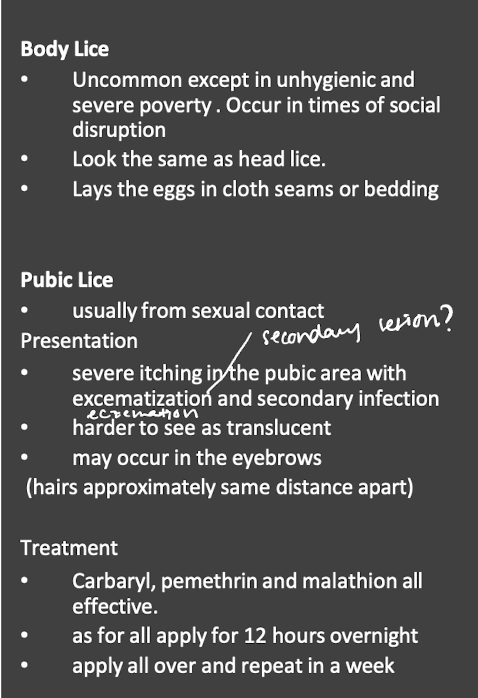
Head lice (transmission, presentation, complication, diagnosis, treatment, prevention)
head-to head contact
presentation
itching
may see excoriations or local lymphadenopathy
complication
secondary bacterial infection
Insect bites (presentation, treatment)
bites present as persistent itchy, oedematous papules
bullous reactions are common on legs of children
treatment
preventative measures like with insect sprays
treat fleas if present
treat infection if present
calamine lotion
local potent topical steroids
wet dressings for severe cases
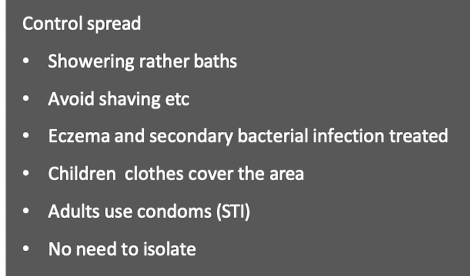
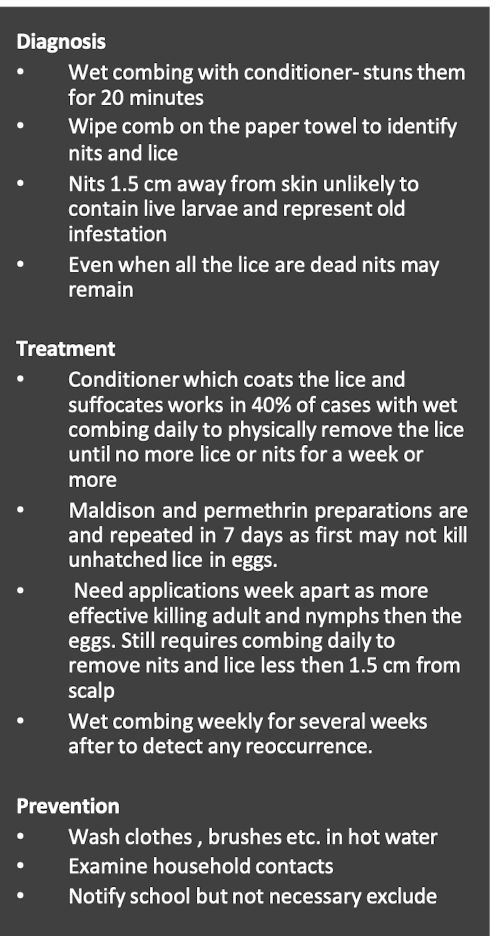
Body and public lice
so yeah