Unit III - Health Assessment and General Survey
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms
Define “General Survey”, what kind of information gathered, and function.
General survey: your first look at the patient, before you even to talk to them
A quick, overall assessment of the patient’s health status
Areas to note:
Smells (can indicate wounds)
Appearance
Levels of consciousness (LOC)
Work of breathing
Verbal/non-verbal communication
Depending on the state and LOC of the patient, the information gathered might not be reliable
i.e. patient is manic
After collecting vital signs, you need to make a decision:
Is it safe to proceed with a full health history /assessment?
Do we need to perform more focused care?
You vital signs gives you a good baseline if you need to intervene immediately because they are too unwell, or if you can proceed with your assessment
Discuss the purpose and steps of the health interview and steps of the physical assessment.
→ Purpose of the Health Interview and Physical Assessment
Create a holistic baseline of a patient’s physical, mental, and social health status to guide diagnosis, treatment, and preventative care.
→ Stages of the Health Interview
Subjective data, patient perspective
Introductory - Introduce yourself and credentials. Reason for the interview. Establish Rapport with the patient.
Working - Information gathering. Use therapeutic techniques to collect and document data
Closing - Thank the client for their time, summarize information received (to confirm if you understood well). Answer any questions.
**Some people add Preparation before introductory!
→ Stages of the Physical Assessment
Objective data, measurable findings
Prepare for the exam - gather all equipment needed
Inspection - what you see, smell, hear?
Always compare symmetrically
Special equipment may be used
Palpate - what can you touch and feel?
Texture, temperature, moisture, vibrations, consistency, size, shape, strength of pulses
Use of finger pads, palmar surface, dorsal surface, and using both hands to compare bilaterally.
Light vs. Deep palpation
Percussion - Tapping of a body part to listen for sounds that reveal underlying structures.
Used primarily by advanced providers
Auscultation - what do you hear?
Uses stethoscope
Intensity, pitch, duration, quality of sound - hearing abnormalities
i.e. heart, stomach, lungs
Identify types of nursing assessments and differentiate a holistic nursing assessment from the physical medical assessment.
→ Types of nursing assessment
Initial comprehensive assessment
Establish baseline of health status
Focuses/Problem-Oriented Assessment
Ongoing/Continuous Assessment
Emergency Assessment
→ Holistic assessment vs physical assessment
Holistic Nursing Assessment
View the patient as a whole person, not just a disease (patient-centered)
Includes:
Physical health
Emotional and mental health
Social and cultural factors
Spiritual beliefs
Lifestyle, coping skills, and support systems
Used to guide nursing diagnosis and care plans
Promote overall health & quality of life
Physical Medical Assessment
Focuses mainly on biological and physiological status (disease centered)
Emphasizes:
Signs and symptoms
Disease processes
Organ systems
Primarily used for medical diagnosis and treatment
Describe effective verbal and nonverbal communication techniques to collect subjective client data and types of communication to avoid in the client interview.
→ Interview Techniques
Verbal communication - active listening, expressing empathy, respect.
Open-ended questions - encourage detailed responses. requires time and active listening
Clarification - helps ensure accurate understanding
Close-ended questioning - direct, non-complex, timesaving. Good for dementia patients for i.e.
Adaptative questioning - a form of open-ended questioning, encourage a patient to fully communicate without interruption. Starts with general questions, making them more specific as you move through the interview
Non-Verbal communication - appearance and demeanor, nonjudgemental attitude, Body posture, Body language/nonverbals (eye contact, touch, facial expression, gestures, physical proximity), power of silence.
Silence - gives the client time to think and share more
Eye contact - shows attention and interest
Facial expression - nonjudgmental encourage openness
Body posture - uncrossed arms, leaning forward
→ Types of communication to avoid
Overuse of close-ended questions, leading question, why questions, medical jargon, false reassurance, judgmental or disapproving statements, interrupting, changing subjects abruptly
More on later slides
Describe ways to adapt the interview for the older client and ways that ethnicity can affect communication patterns.
→ How to adapt interview:
Have family member present that can assist you with patient
Explain information slowly, speak louder if they have trouble hearing
Print information for them as they might not be techy savvy
Face the client so they can see your lips and expressions
Ensure glasses and hearing aids are in place
Allow extra time for appointment
Use simple, direct language
Be mindful and respectful when asking questions that might be sensitive to patient (i.e. sexual status)
→ Ways ethnicity can affect communication
Language barrier (use interpreter), trust issues in the conventional medical system, eye contact (direct eye contact might be disrespectful), personal space and touch, communication style (direct vs indirect), role of family
Identify the major categories of a complete client health history. (8 in total)
→ A complete Health History Includes:
Demographic Data - name, date of birth (DOB), contact, race, gender, preferred pronouns, marital status, occupation, religion, allergies, resuscitation status.
Chief Complaint - patient’s reported signs and symptoms that have caused the patient to seek medical attention.
History of Current Illness (HPI) – Utilizing HPI assessment tools such as COLDSPA, OLDCARTS, WILDA, etc.
Chronological narrative of patient’s current health problem
HPI assessment tools:
COLDSPA - character (what feels like), onset (when it started), location, duration (how long it lasts), severity, pattern (what makes it better/worse), and associated factors (other symptoms
WILDA - words (can you describe the pain?), intensity, location, duration, alleviating/aggravating factors
Past History - previous treatments, surgeries or conditions.
Family History - Reviewing familial/hereditary diseases
Review of Systems (ROS) - Comprehensive review of each body system such as cardiovascular, musculoskeletal or urinary.
Head to toe
Lifestyle/ Health Practices - nutritional and exercise habits, sleep, substance use, relationships and support etc.
Functional Assessment - Patient’s ability to care for themselves
Describe the process for performing a ROS (Review of System)
Goal - Evaluate overall health and identify any unexpected manifestations of the body system in a head-to-toe manner
Skin
HEENT – head, ears, eye, nose, throat
Chest and Lungs
Cardiovascular and Peripheral Vascular
Abdomen and GI
Genitalia, anus, rectum
Musculoskeletal
Neurological
Depending on symptoms a patient reports in any area you should conduct a more thorough assessment of that area.
Describe questions to ask to assess the client’s lifestyle and health practices.
Do you exercise regularly? How many times per week? How long?
How many meals a day do you consume. Could you describe what you consume in each meal?
Do you smoke?
How many alcoholic beverages do you drink per week?
Differentiate variations of assessment across the lifespan.
Children - it is important to use age-appropriate language and communication techniques. An example is by engaging the child in play during the interview, this can decrease the child’s anxiety, provide distraction from the medical evaluation, and allow the nurse to assess developmental milestones.
Involve parent or guardian
Adolescents - may have unique health concerns related to puberty, sexuality, and mental health. It is important to use age-appropriate language and respect their privacy and confidentiality.
Involve them in their care decision, use nonjudgmental attitude
Adults - may have different health concerns based on their age, gender, and lifestyle factors. Younger adults will be worried about conception while older ones will be worried about stress
Consider the patient's cultural background, occupation, educational level, health status, and family history when conducting the interview.
Older adults - may have unique health concerns related to chronic conditions, functional decline, cognitive impairment.
Use clear and simple language and allow sufficient time for the patient to answer.
Be mindful of sensory and mobility impairments, and adjust the interview techniques accordingly.
Involve family members or caregivers as needed to provide support and help with communication.
Document assessment data.
“Clear, accurate, and accessible documentation is an essential element of safe, quality, and evidence-based nursing practice” (American Nurses Association, 2010).
Characteristics of good nursing documentation:
Accurate, relevant, and valid.
Clear, concise and complete
Authenticated
Legible (when handwritten)
Timely (dated and time-stamped) and completed in a timely manner (i.e. within your shift, right after care was done)
Reflective of the nursing process
Made using standardized terminology (nursing/medical language and abbreviations.)
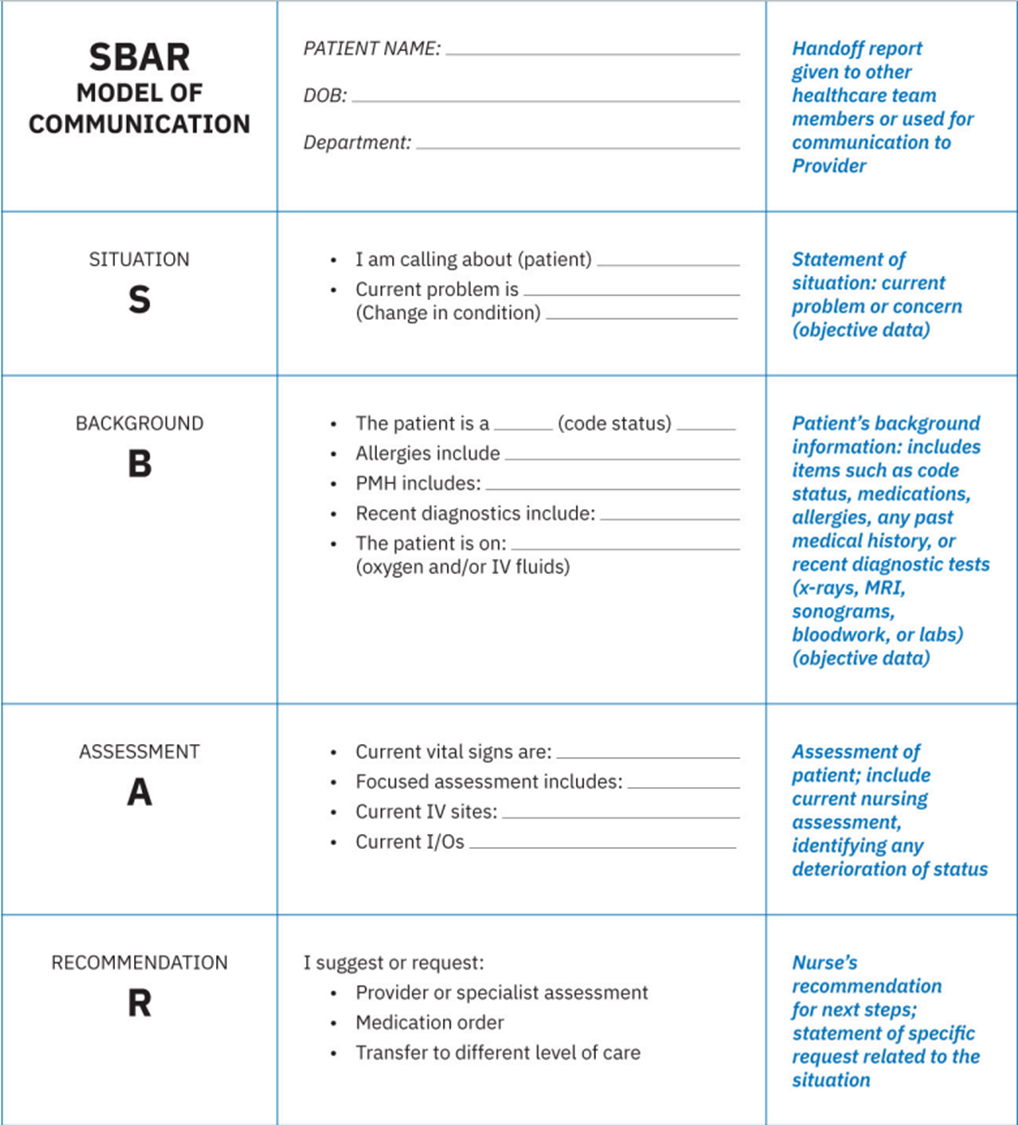
When giving report, nurse should always use the SBAR model:
Situation - current problem or concern (objective data)
Background - code status, medications, allergies, any past medical history, recent diagnostic tests (X-ray, MRI, sonograms), blood work and lab
Assessment - current nursing assessment, identify any deterioration of status
Recommendation - nurse’s recommendation for next steps; statement of specific request related to the situation,
Discuss the purposes of the client electronic health record (EHR) & safe documentation.
To allow communication of care to be available for all professionals working in the care team of a patient.
The electronic health record (EHR) is a digital format of a patient’s chart that contains data related to the patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results.
An electronic medical record (EMR) is the digital version of a patient’s chart at any one practice. Not meant to be shared or transferred to other facilities
The EHR, on the other hand, is more of a snapshot of the patient’s entire medical history. The purpose of the EHR is to enable multiple healthcare professionals across different platforms to easily view the patient’s health history, risks, health promotion, education, and actual long-term care issues
Access to EHRs is monitored and limited to only those who have a need to know in order to complete their job
The EHR is the nurse’s best form of evidence detailing interaction with a patient
The coordination of care among team members can occur with proper exchange of patient information across an interlinked healthcare system that allows for all stakeholders to have access to the same information.
If the health record is inadequate or erroneous, a provider may make an incorrect clinical judgment that could adversely affect continuity of care and result in poor patient outcomes.
HIPAA regulations state that a healthcare facility may release protected health information without written consent in certain situations, such as the investigation and prosecution of a crime, public health and emergencies, research, judicial and administrative proceedings, and quality improvement, licensing, and regulation.
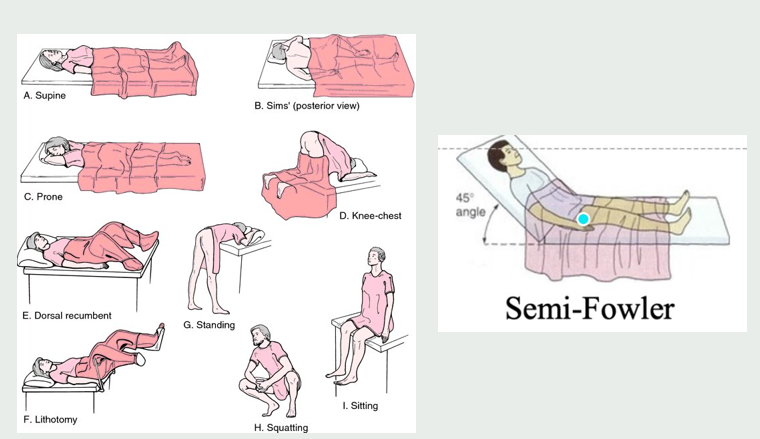
Describe all the position names below:
A. Supine
B. Sims’
C. Prone
D. Knee-chest
E. Dorsal recumbent
F. Lithotomy
G. Standing
H. Squatting
I. Sitting
J. Semi-Fowler
Prone position allows for lung expansion
Define therapeutic communication and the 5 steps of it
Definition: the specific techniques and strategies nurses use to establish a therapeutic relationship with patients and promote the patient’s well-being
Develop specific communication goals - use the SMART model to identify a goal
Create the message - develop a plan to achieve the goal and find a way to communicate the plan to the patient in an understandable way (consider cognitive abilities, educational levels, cultural preferences, etc.)
Deliver the message - includes verbal and nonverbal communication. use a clear tone and plain language, be mindful of the patient’s body language, use the patient’s preferred language so they understand, actively listen to the patient, and demonstrate patience and respect throughout the conversation.
Listen to the response - this is a two-way process. Feedback comes in verbal and nonverbal.
Seek clarification of the response - clarify any indirect, unclear, or ambiguous responses with the patient when possible. i.e. if patient sounds mad in the response, try to understand why
List 4 effective therapeutic communication techniques and some nontherapeutic communication techniques
→ Characteristics of Effective Therapeutic Communication (build good relationship)
Build trust through honesty - trust increase adherence to the treatment plan and improved outcomes
Build a trusting relationship through admitting mistakes/errors, honoring patient’s autonomy and choices, finding unknown answers and following up to close the loop, providing realistic expectations, building rapport, demonstrating consistent behavior, and encouraging open communication, being transparent
Active listening - we are communicating verbally and nonverbally that we are interested in what the other person is saying while also actively verifying with the speaker that we understand.
i.e. clarification, make sure you understood, withhold judgement, provide feedback
Respect the patient’s values and beliefs - through cultural awareness, understand and value other beliefs
Show compassion - communicate with empathy
→ Characteristics of Nontherapeutic Communication (to avoid)
Asking personal questions
Giving personal opinions
Changing subjects
Providing false reassurance
Stating generalization and stereotypes
Asking why questions