OP: White lesions
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
10 Terms
Surface deposits: Aetiology of Mucosal Burns
Electrical: biting on a live wire
Thermal: Ingestion of extremely hot food/beverages.
Chemical: placement of medications/other chemicals on the mucosa to treat pain i.e., Aspirin, sodium perborate, hydrogen peroxide, gasoline, turpentine, alcohol, and battery acid
Iatrogenic: dental materials e.g, silver nitrate, formocresol, dental cavity varnishes, and acid-etch material
Clinical features of various burns
Electric Burns
Children younger than four years
Lips and commissure (mucobuccalfold, tongue)
Adjacent teeth may be nonvital, with(out) necrosis of surrounding alveolar bone.
Malformation of developing teeth
Temporary facial nerve paralysis
Painless, charred, yellow area, no bleeding. When necrotic tissue sloughs off, bleeding.
Oedema up to 12 days
Thermal (Food) Burns
Palate & posterior buccal mucosa
Erythema, ulceration, and necrosis
Hot beverages: Upper airway swelling cause dyspnoea
Chemical burn Aspirin Burn
Patients place an aspirin tablet against the buccal mucosa
Caustic effect causing coagulation necrosis and formation of a region of white slough.
Clinical history provides the diagnosis. Treat with saline mouthwashes.
Developmental lesions: Fordyce granules
Ectopic sebaceous glands
Creamy yellowish soft granules between the vermilion and the oral mucosa of the upper lip
Buccal mucosa, RMR and lips
Children after the age of 3 years, increasing during puberty and later adult life
Mainly in adults- Prominent in men: advancing age, with oily skin, rheumatic disorders, in hereditary non-polyposis colorectal cancer syndrome: the most common site is the lower gingiva and vestibular oral mucosa.
No treatment is reliable or indicated, just reassurance
Developmental lesions: Leukoedema
Bilateral faint whitish lines in normal buccal mucosa disappear if the mucosa is stretched (a diagnostic test)
Variation of normal. Majority of the population. Often in Africans.
Aetiology not est.
Clinical Features
-Incidental finding, asymptomatic, symmetrical distribution in the buccal mucosa, lesser extent over the labial mucosa.
-Grey-white, diffuse, filmy, or milky surface alteration, wrinkling or corrugation.
Histopathology
-Parakeratotic and acanthotic epithelium
-Intracellular oedema of spinous cells
-Enlarged epithelial cells with small, shrunken nuclei in clear cytoplasm.
Differential Diagnosis
White sponge naevus, frictional hyperkeratosis, oral lichen planus
The disappearance on stretching is distinct
Treatment is not necessary
Reactive lesions: Hyperkeratosis(friction, linea alba)
-Friction-induced hyperkeratosis, in areas that are commonly traumatised. Protective white lesion from chronic rubbing, friction against an oral mucosal surface.
-Lips, lateral tongue, buccal mucosa, edentulous alveolar ridges
-Biopsy not indicated- taken shows hyperkeratosis no dysplastic change. Chronic inflammatory cells.
-Cause is removed, lesion should subside. In doubt, perform a biopsy!
Linea alba
-Horizontal streak level with the occlusal plane.
-Trauma from the buccal surfaces of the teeth.
-Bilaterally, asymptomatic, restricted to dentulous areas.
-Treatment is not required.
Diagnosis
-Clinically confident of traumatic cause, no biopsy may be required, in doubt, biopsy taken.
Treatment:
-Observation: Lesion should resolve or at least reduced in intensity over time, thus confirming clinical diagnosis. Allow unmasking of any underlying lesion that may not be related to trauma.
-Control the habit/ smoothen
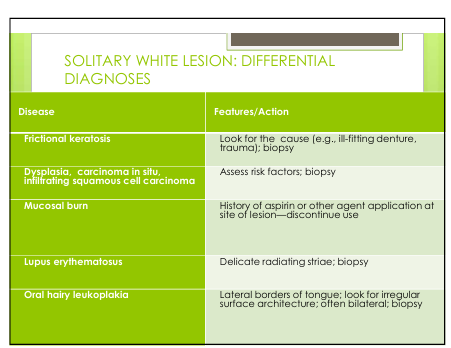
DDx for Solitary white lesions
Reactive lesions: White hairy tongue
Clinical term referring to a condition of filiform papillary overgrowth on the dorsal surface of the tongue of variable colour.
Initiating or predisposing factors: Broad-spectrum antibiotics, such as penicillin. Systemic corticosteroids. Oxygenating mouth rinses, smokers, radiotherapy, hematopoietic stem cell transplantation
Aetiology: Alteration in microbial flora, with proliferation of fungi and chromogenic bacteria, along with papillary overgrowth.
Diagnosis: The clinical features are usually characteristic, confirmation by biopsy is not necessary, cytologic or culture studies are of little value. Identification and discontinuation of predisposing factor. Brushing the tongueand maintaining good oral hygiene.
Reactive lesions: Oral hairy leukoplakia
Associated with immunosuppression e.g. (esp. AIDS and organ transplantation)
Represents an opportunistic infection by Epstein Barr Virus(EBV)
Presence of OHL in a patient with no known cause of immunosuppression, is highly suggestive of HIV infection. Pt with known HIV infection CF sufficient.
May occur before or after the diagnosis of AIDS, may be secondarily infected by Candida albicans.
Unilateral < bilateral on lateral margins of the tongue
White mucosal plaque that does not rub off, white vertical streaks to shaggy surface leukoplakia
For a definitive diagnosis, demonstration of EBV (by in situ hybridization, PCR, immunohistochemistry, Southern blotting, or electron microscopy. )
Histopathology
-Viral inclusions or peripheral displacement of chromatin with a smudgy nucleus.
-Hyperparakeratosis
-The spinous cell layer shows: ballooning degeneration, perinuclear clearing.
-C. albicans hyphae, extending into superficial epi
-Scant Langerhans cells
DDx:
IL, tobacco leukoplakia, lichen planus, LE, frictional hyperkeratosis, CHC.
Treatment and Prognosis
-Investigation for HIV infection or other causes of immunosuppression should be undertaken. Treatment of underlying cause. Often AIDS assoc.
-10% of individuals with diagnosed oral hairy leukoplakia have AIDS at the time of diagnosis, 20% develop within a year of the diagnosis.
-Cosmetic reasons treat w antivirals( acyclovir, ganciclovir, famciclovir,)
Immune mediated lesions: Lichen planus
• Disorder of skin & squamous mucosa
• May result from CD8+ T cell mediated cytotoxic immune response against antigens in basal cell layer & dermo-epidermal junction
Clin Features:
o Mainly affects middle ages individuals
o Children rarely affected
o Female predominance
o Most common type: Reticular form
▪ Numerous interlacing white keratotic lines/ striae (Wickham’s striae) • Produce annular/ lacy pattern ▪ Buccal mucosa: most common site, symmetric pattern, bilateral.
o Plaque form of lichen planus
▪ Resemble leukoplakia clinically but multifocal distribution ▪ Range from slightly elevated to smooth & flat ▪ 1˚ sites: dorsum of tongue & buccal mucosa
o Erythematous/ Atrophic form
▪ Appears as red patches w/ v. fine white striae ▪ May be seen in conjunction w/ reticular/ erosive variants
Erosive/ulcerative lichen planus
▪ Attached gingiva: commonly involved ▪ burning, sensitivity & generalized discomfort. Erythematous patches with ulceration and fine white striae.
Bullous LP when seperation of under CT.
Differential Dx:
o Other diseases w/ multifocal bilateral presentation. Lichenoid drug rxns, (LE), white sponge nevus, hairy leukoplakia, cheek chewing, graft versus host disease, candidiasis, IL & squamous cell carcinoma