PDA Lecture 26: Toxicology Principles for Management lecture 1
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
Toxicology
Field of science that helps us understand the harmful effects that chemicals, substances, or situations, can have on people, animals, and the environment
- derived from Greek term toxikos ("bow") and toxicon ("poison into which arrowheads are dipped")
Xenobiotic
describes chemical substances that are foreign to human life
- ex: plant constituents, drugs, pesticides, cosmetics, etc.
Poison
Any substance that can cause severe organ damage or death if ingested, breathed, injected into the body or absorbed through the skin
What is poisoning?
an adverse effect from a chemical that has been taken in excessive amount
Poisoning can produce ____________________ that may be treated readily in the outpatient setting or ____________________ that require intensive medical intervention
- minor local effects
- systemic life-threatening effects
Which of the following best defines the field of toxicology?
A. The study of drug absorption and metabolism
B. The study of how nutrients impact human health
C. The study of harmful effects caused by chemicals and substances
D. The development of new drug formulations
C. The study of harmful effects caused by chemicals and substances
T/F: All xenobiotics are harmful to the body
FALSE
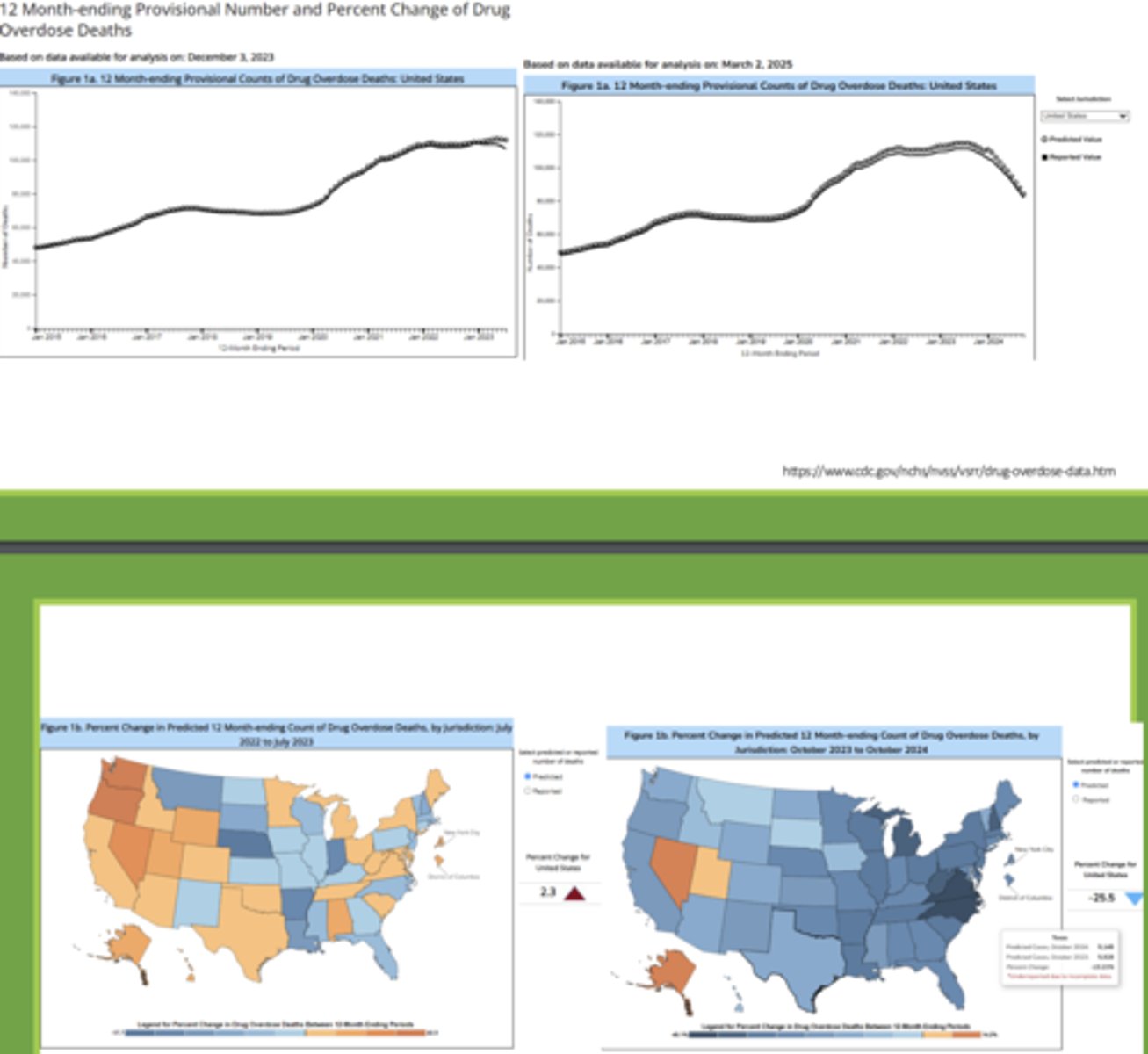
Annual poisonings in the US:
- ____________ overdose has remained a public health emergency since 2017.
- Accidental poisonings account for ________________ deaths annually
- ~_______________-related ED visits are due to poisoning
- opioid overdose; 18-45 age group most common cause of death
- ~69,000; ~0.2% of poisoning involve children younger than 5 years
- ~2.3 million drug-related
Spectrum of toxicity
Mild:
Severe:
Mild: local effects that may be treated readily in the outpatient setting
Severe: systemic-life threatening effects that require intensive medical intervention
Recognizing the poisoning risk: (6)
• The substance involved: is it toxic in small amounts?
• The dose: how much was taken?
• Time: when did it happen?
• Patient-specific factors: like age, weight, medical conditions
• Route of exposure: swallowed, inhaled, injected, or absorbed through skin
• Symptoms: are they present yet? How severe?
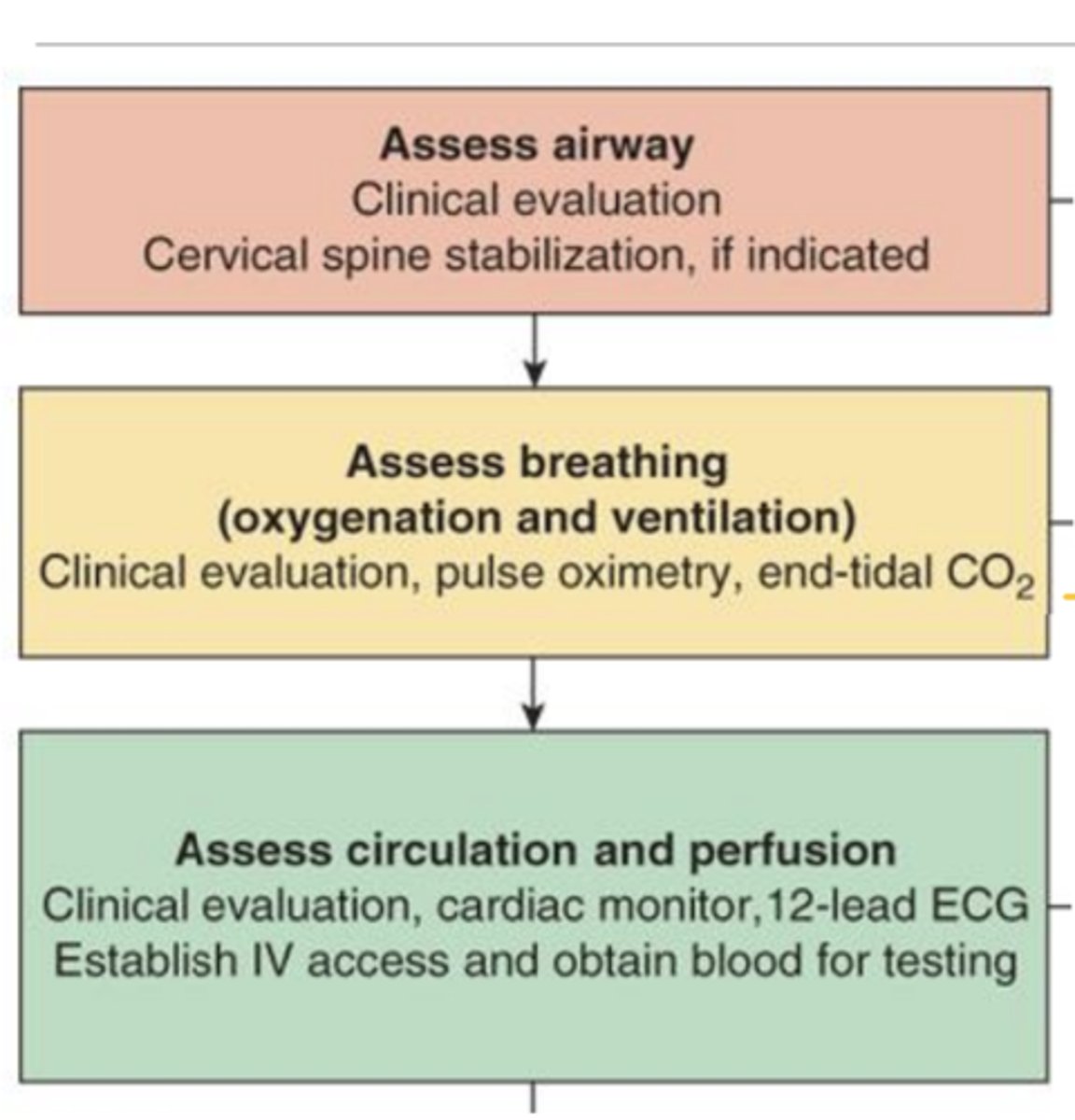
Basic Guide to Management of Poisoned Patients: Initial Evaluation and Stabilization (ABCs)
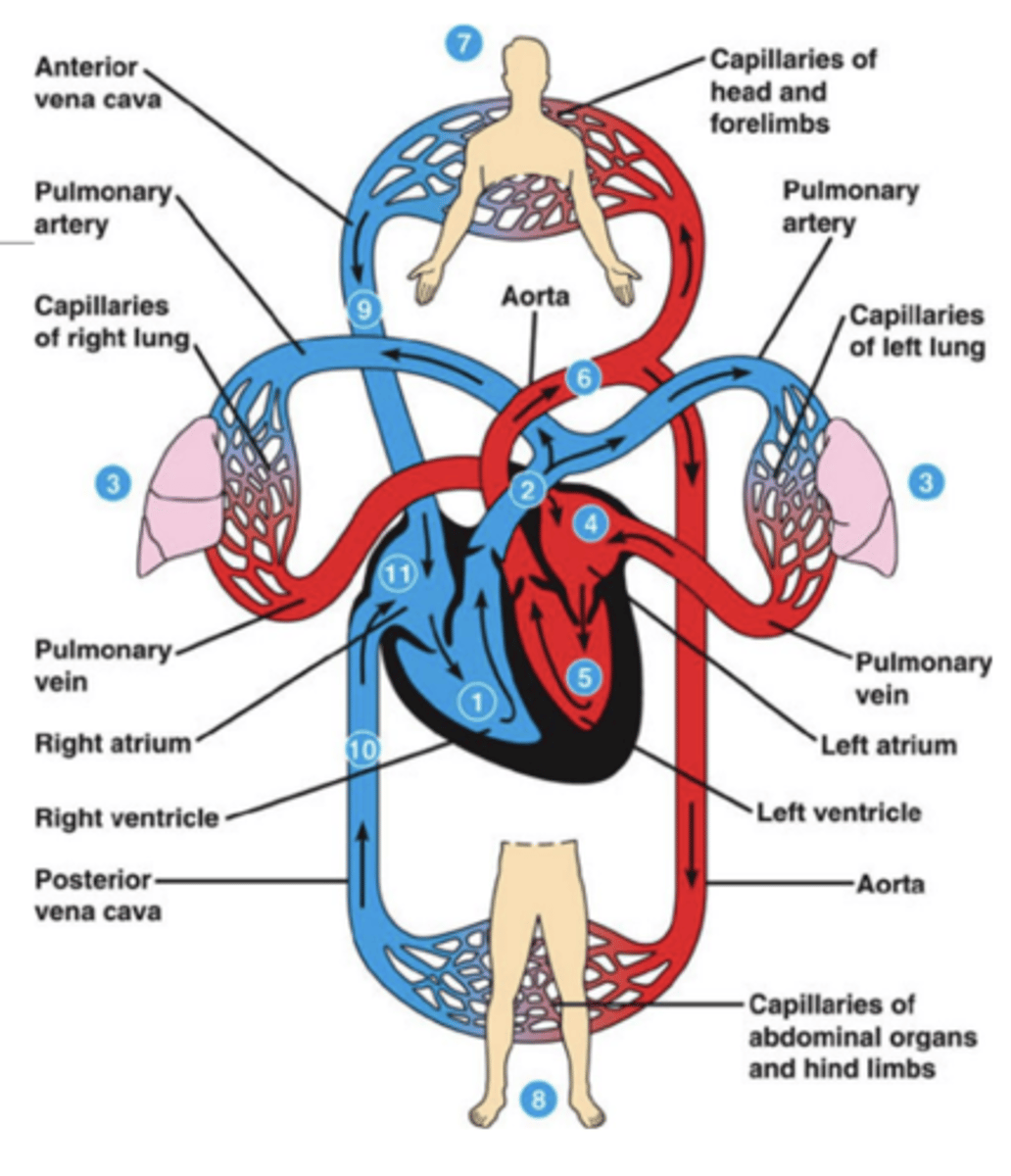
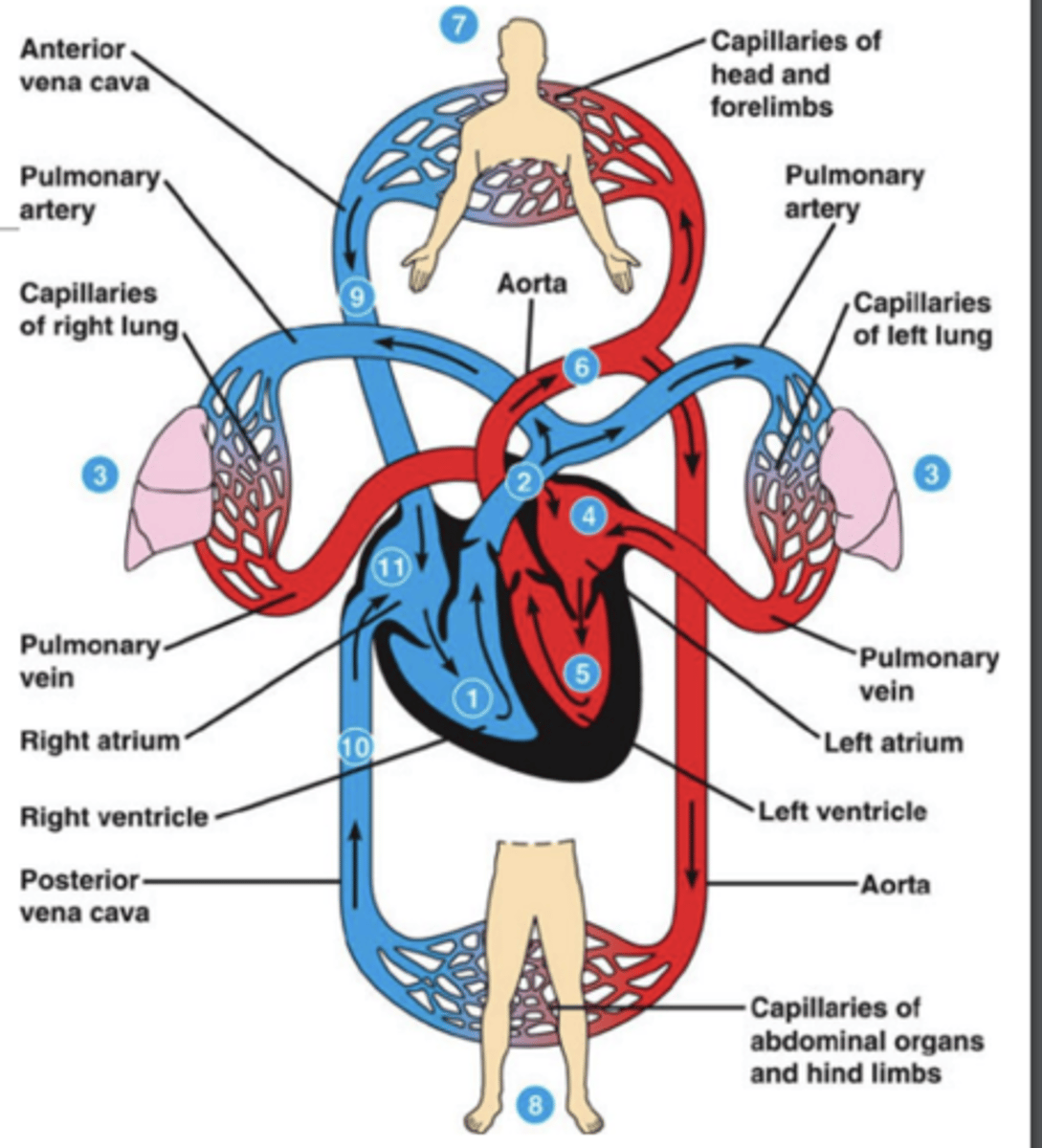
Airway:
• Is the airway protected, obstructed?
• Is the patient protecting their airway?
- cervical spine stabilization, if indicated
Breathing:
• Respiratory rate, oxygen saturation, work of breathing
Circulation:
• Blood pressure, heart rate, perfusion status
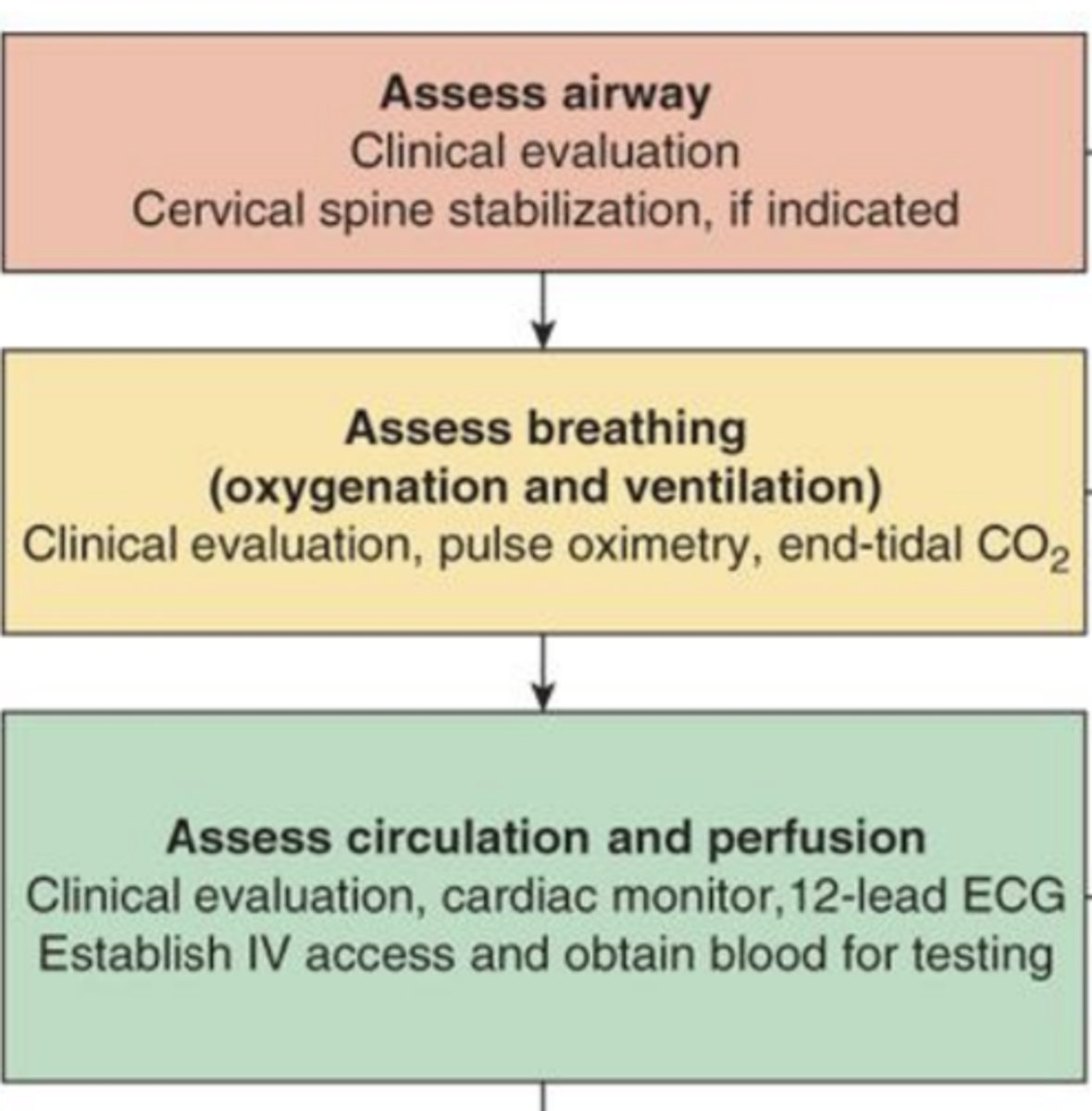
What to evaluate during the Initial Evaluation and Stabilization (ABCs)? (5)
Vital signs
• Temperature
• Heart Rate
• Respiratory Rate
• Blood Pressure
• Oxygen Saturation
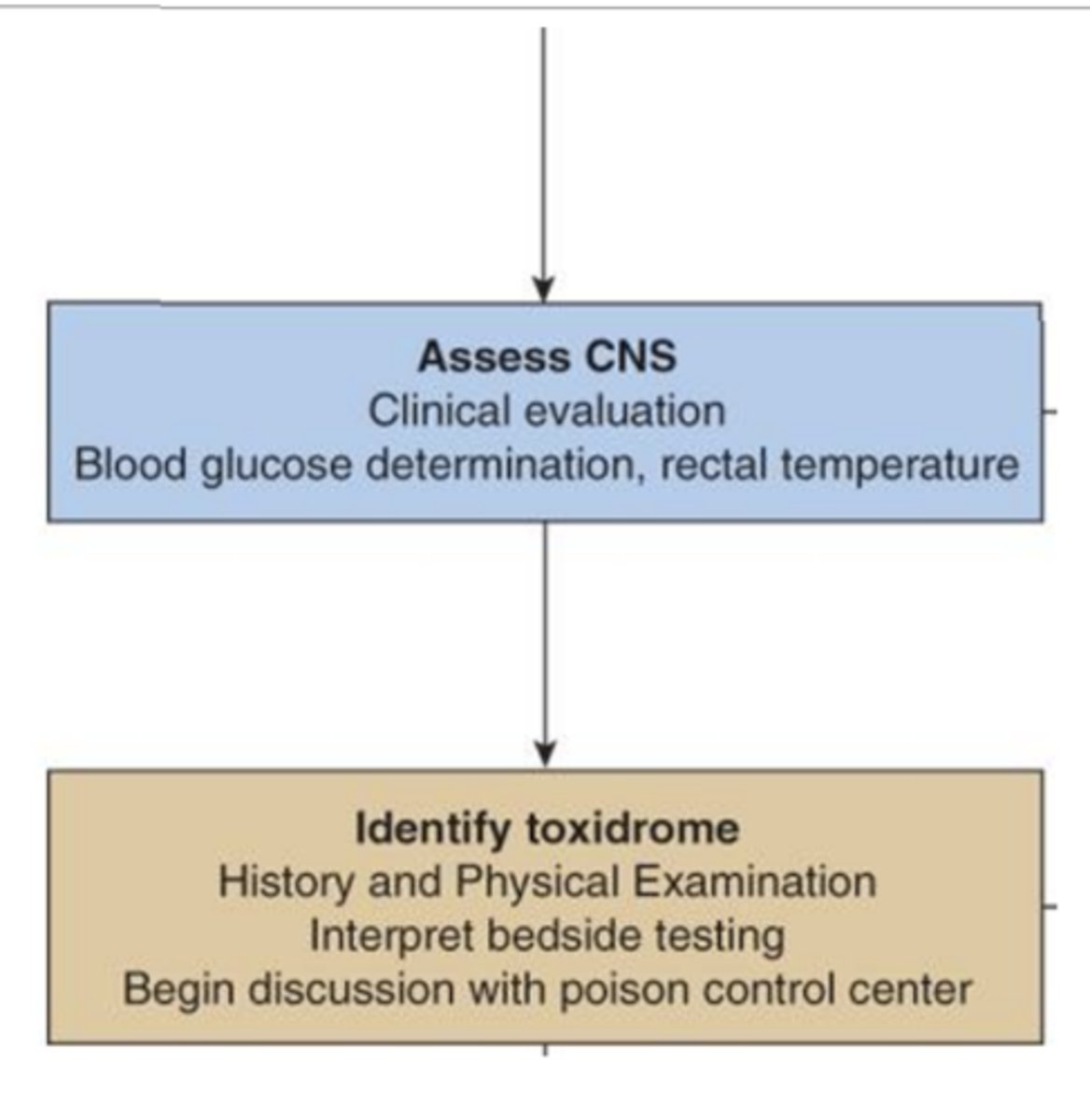
Basic Guide to the Management of Poisoned Patients (cont.): Asses CNS and Identify toxidrome
Assess CNS
• Blood glucose determination, rectal temp.
Disability
• Neurologic status (GCS score), seizure activity, agitation
Toxidrome recognition
• Help identify a class of toxin based on physical signs/symptoms
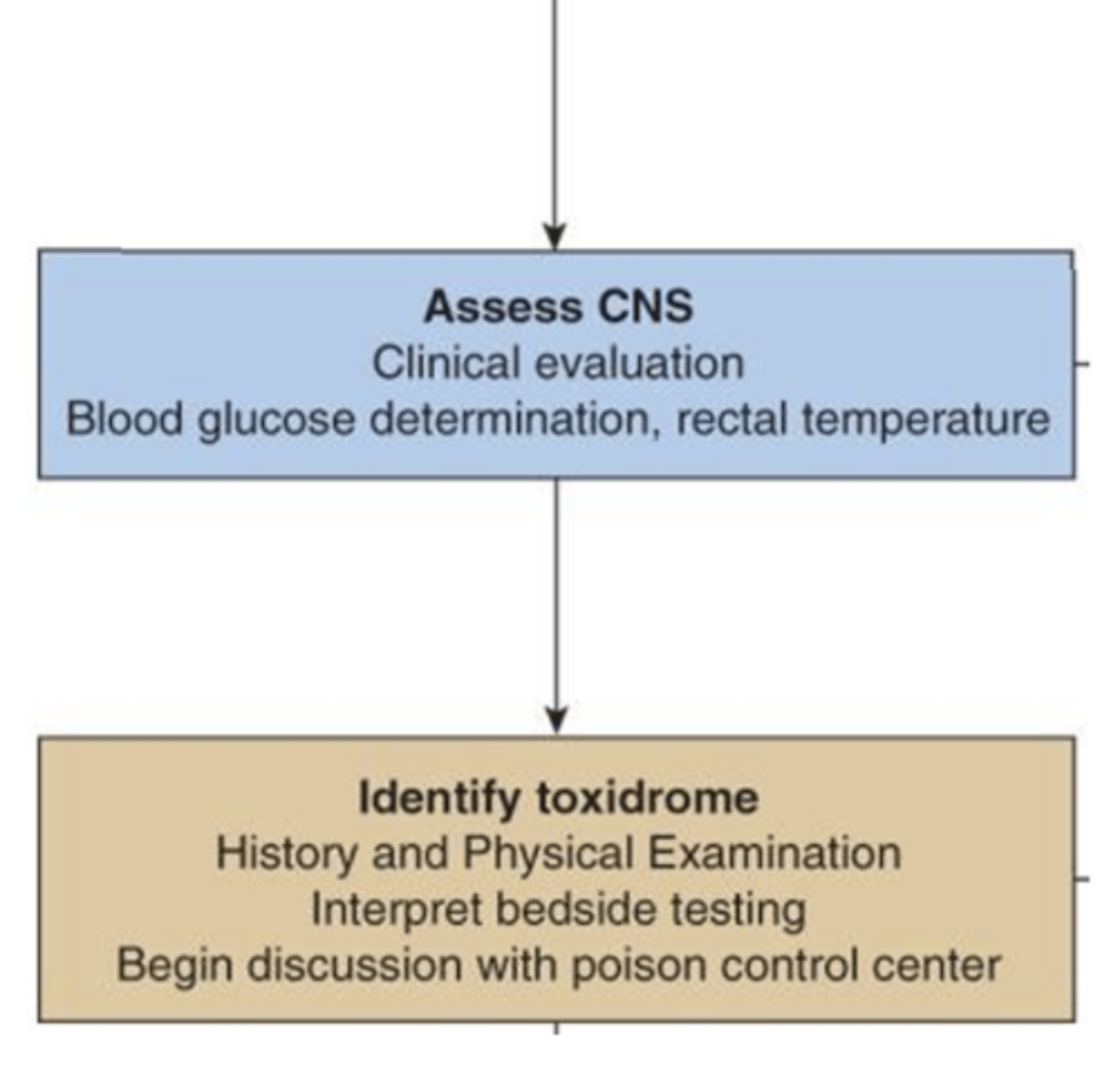
Toxidrome Recognition:
• Anticholinergic:
• Cholinergic:
• Opioid:
• Sympathomimetic:
• Sedative-hypnotic:
• Serotonin syndrome:
• Anticholinergic: dry skin, mydriasis, hyperthermia
• Cholinergic: salivation, lacrimation, urination, diarrhea
• Opioid: miosis, respiratory depression, CNS depression
• Sympathomimetic: tachycardia, hypertension, agitation)
• Sedative-hypnotic: CNS depression, bradypnea
• Serotonin syndrome: clonus, agitation, hyperreflexia
Basic Guide to the Management of Poisoned Patients (cont.): Diagnostic Investigation/Work-Up (7)
• Blood glucose (hypoglycemia is a common reversible cause of altered mental status)
• Electrolytes, renal function, liver function
• Serum osmolality & osmolar gap
• Anion gap: helps identify toxic alcohols or metabolic acidosis
• Drug levels (ex: acetaminophen, salicylates, lithium, digoxin, valproic acid)
• Urine drug screen
• ECG: look for QRS widening, QT prolongation, arrhythmias
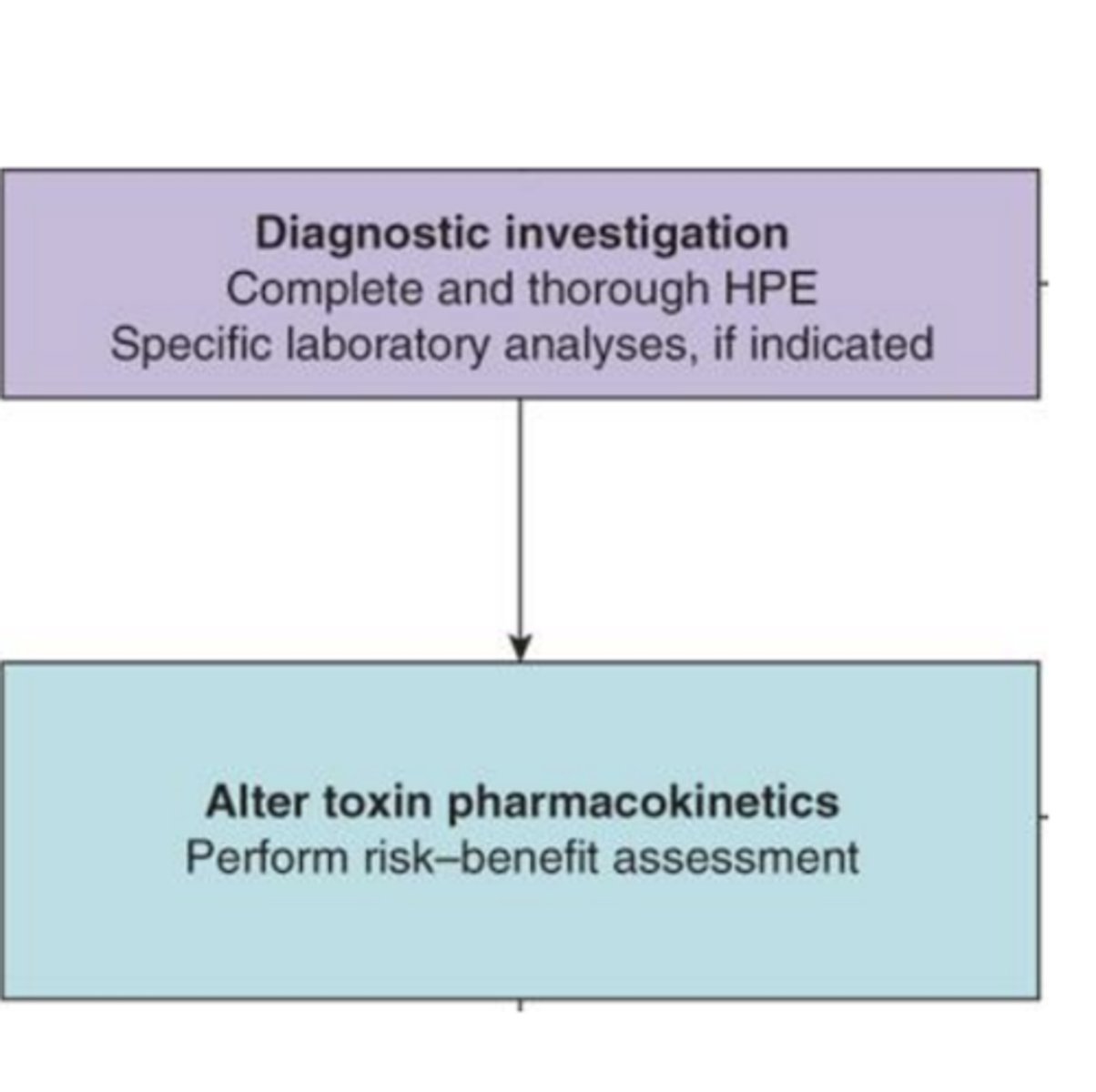
Basic Guide to the Management of Poisoned Patients (cont.): Alter toxin pharmacokinetics:
Absorption and distripution Considerations
- Perform risk-benefit assessment
Absorption & Distribution Considerations:
• Formulation of drug (e.g., extended-release, enteric-coated)
• Time since ingestion (early hours = higher chance for decontamination)
• Co-ingestants (can alter absorption and metabolism)
Basic Guide to the Management of Poisoned Patients (cont.): Determine disposition
GI decontamination (3)
• Activated charcoal (if within 1–2 hours and no contraindications)
• Gastric lavage (rarely used, only in severe/life-threatening cases)
• Whole bowel irrigation (e.g. sustained-release meds)
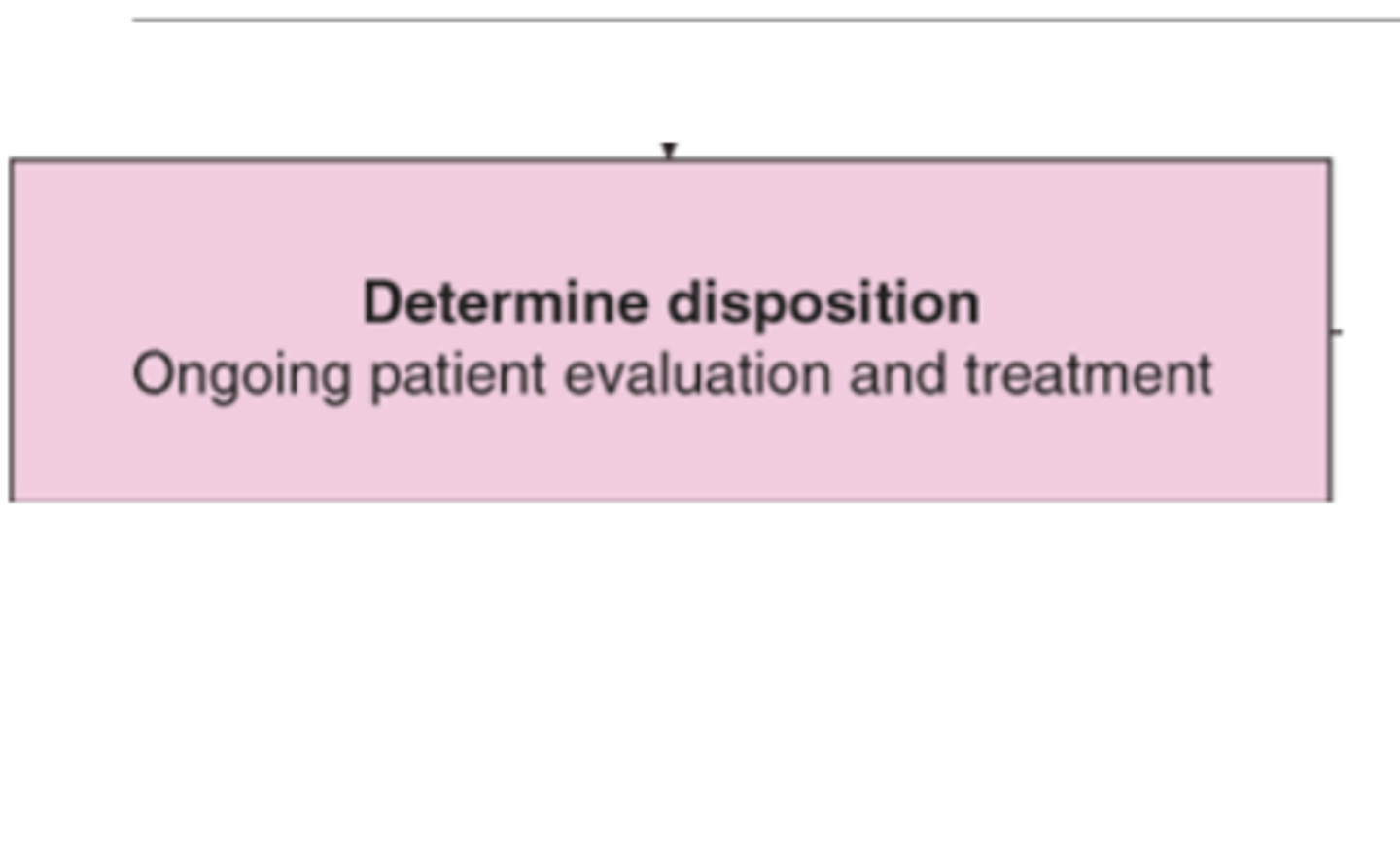
Basic Guide to the Management of Poisoned Patients (cont.): Determine disposition
Metabolism and Elimination (3)
• Hepatic or renal impairment (can alter drug clearance)
• Zero-order vs. first-order kinetics
• Enterohepatic recirculation
Basic Guide to the Management of Poisoned Patients (cont.): Determine disposition
Enhanced Elimination (3)
• Urinary alkalinization (e.g., for salicylates)
• Hemodialysis (e.g., for lithium, methanol, ethylene glycol)
• Multi-dose activated charcoal (for some drugs with enterohepatic recirculation)
Basic Guide to the Management of Poisoned Patients (cont.): Determine disposition
Withdrawal Risk: Asses for potential withdrawal syndromes if chronic use of.....(4)
• Opioids
• Benzodiazepines
• Alcohol
• Barbiturates
Basic Guide to the Management of Poisoned Patients (cont.): Determine disposition
Psychiatric and Social Evaluation: (3)
• Suicide risk assessment
• Psychiatric referral once medically stable
• Substance use history/support needs
In the practice of medical toxicology, _________________ play an important role
vital signs

Vital signs are a valuable parameter used to assess and monitor a pt's response to.....
treatment and antidotal

T/F: Some patients should be considered too agitated, too young, or too gravely ill to obtain a complete set of vitals
FALSE
no pt should be considered to young, ill, etc.

T/F: The difficulty in defining what constitutes "normal" vital sigs in an emergency setting is inadequately addressed
TRUE
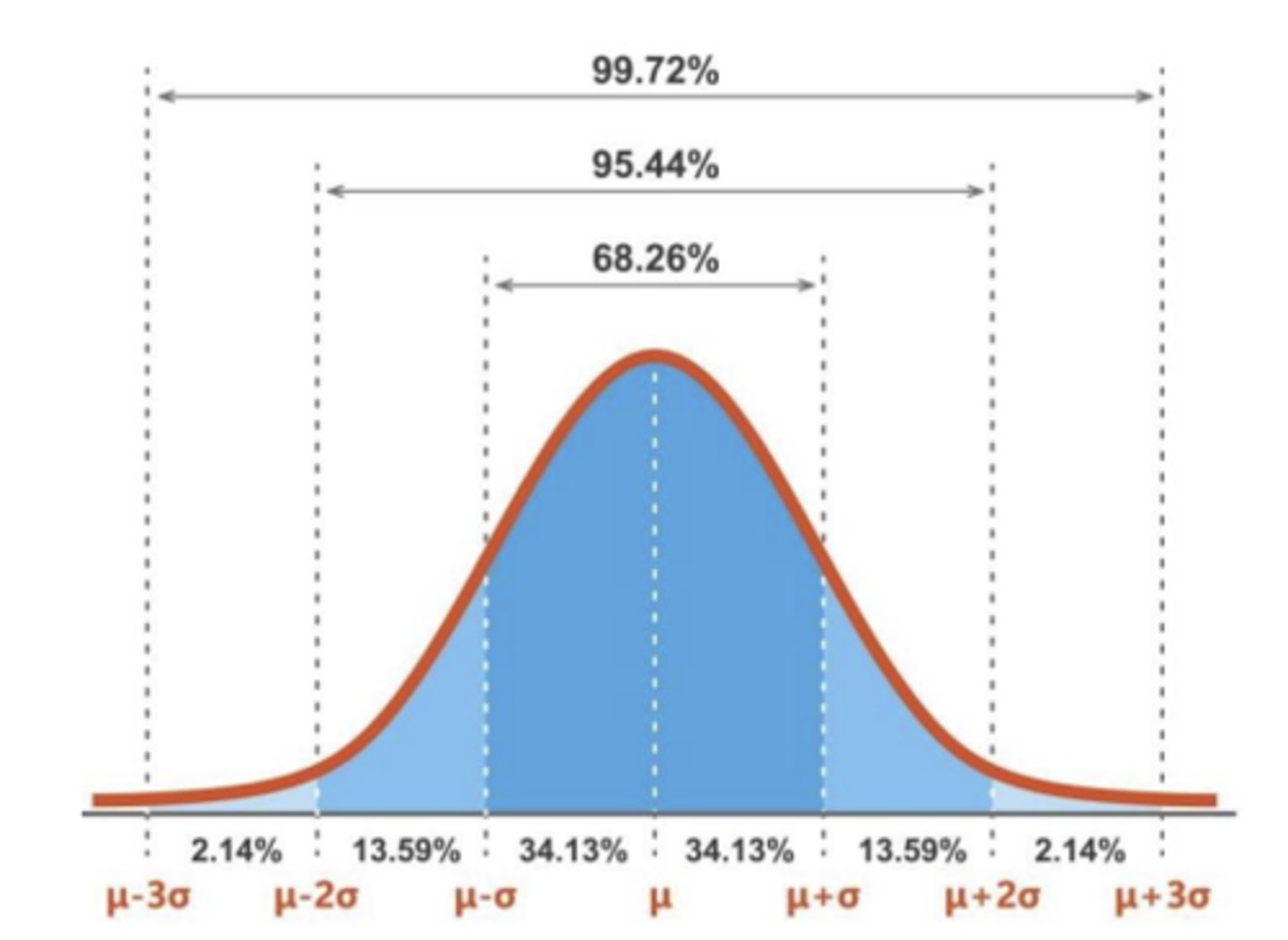
•Even in nonemergent situations, "normalcy" of vital signs depends on the....
clinical condition of the patient
ex: a sleeping or comatose pt may have physiologic bradycardia
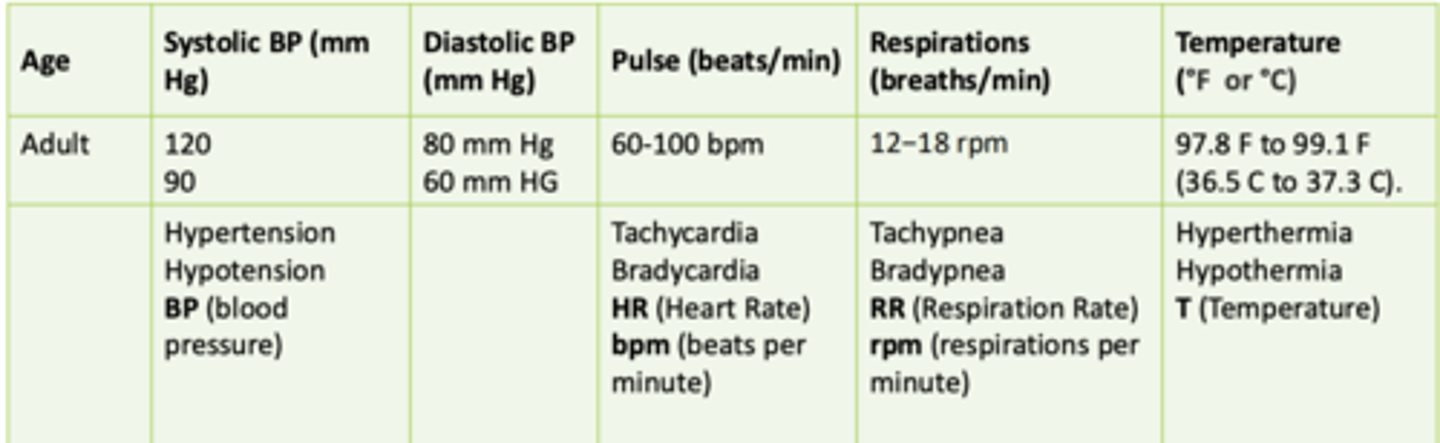
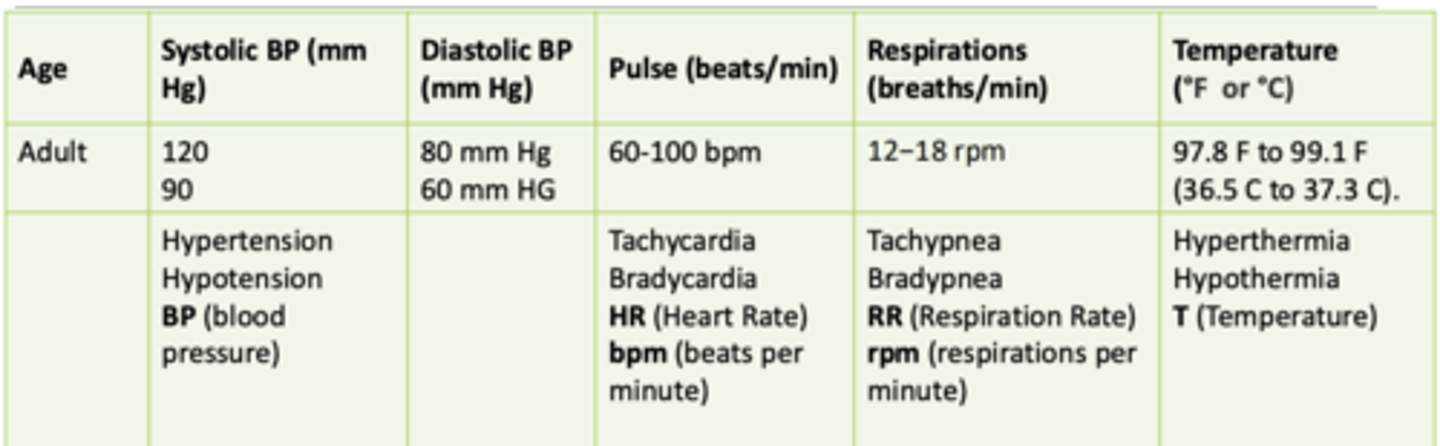
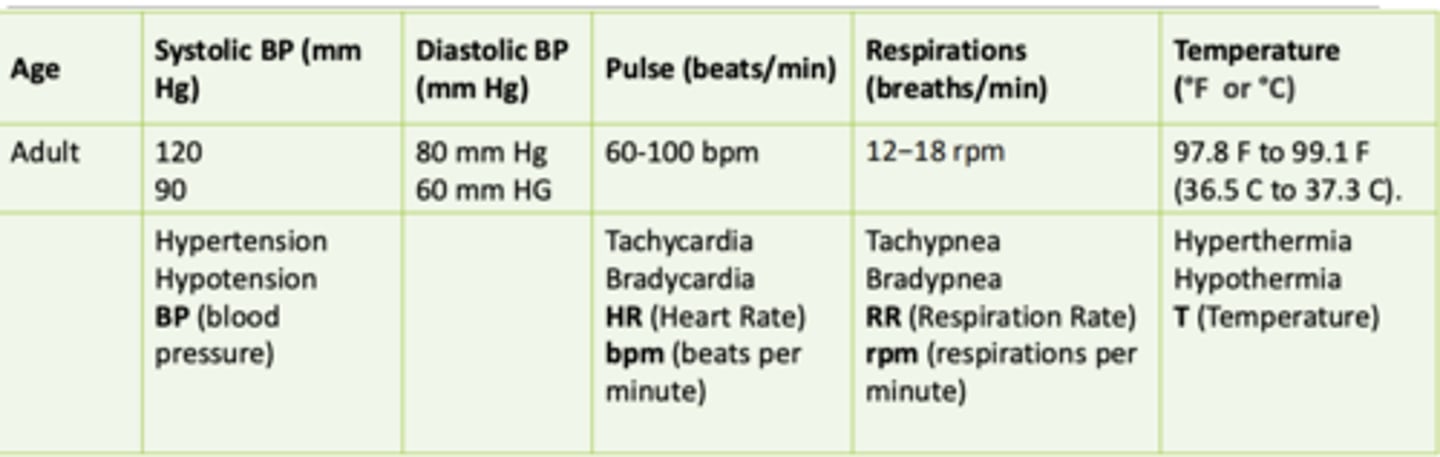
Normal BP for an adult; systolic/diastolic
120 mmHg/80 mmHg
90 mmHg/60 mmHg
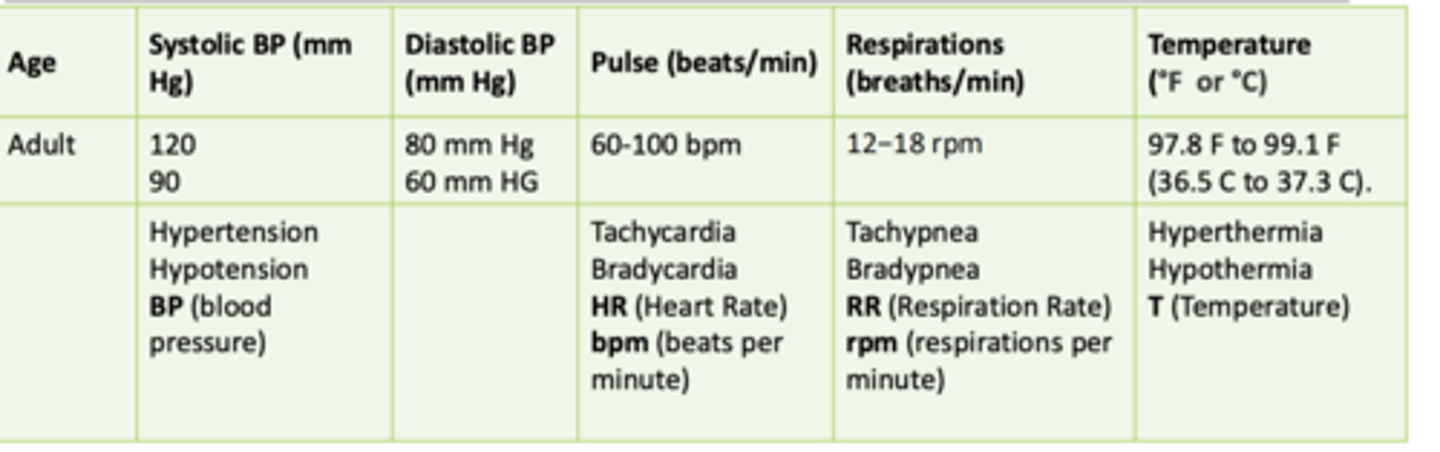
Normal heart rate for adults; pulse (beats/min)
60-100 bpm
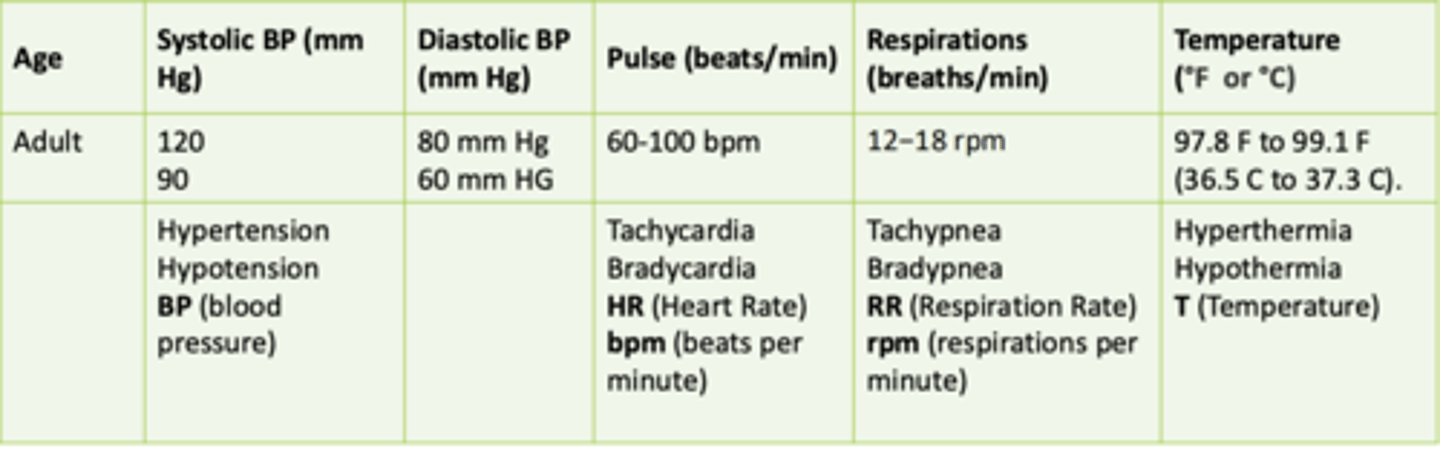
Normal respiration rate for adults (breaths/min)
12-18 rpm
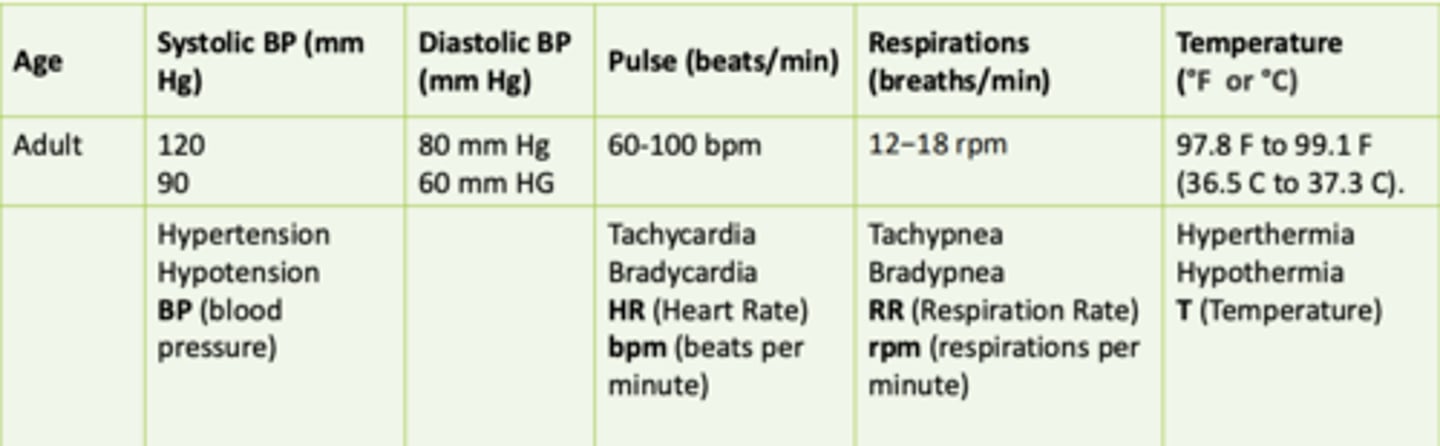
Normal temperature for adults in F and C
• 95°F- 100.4°F
• 36.5°−37.3°C
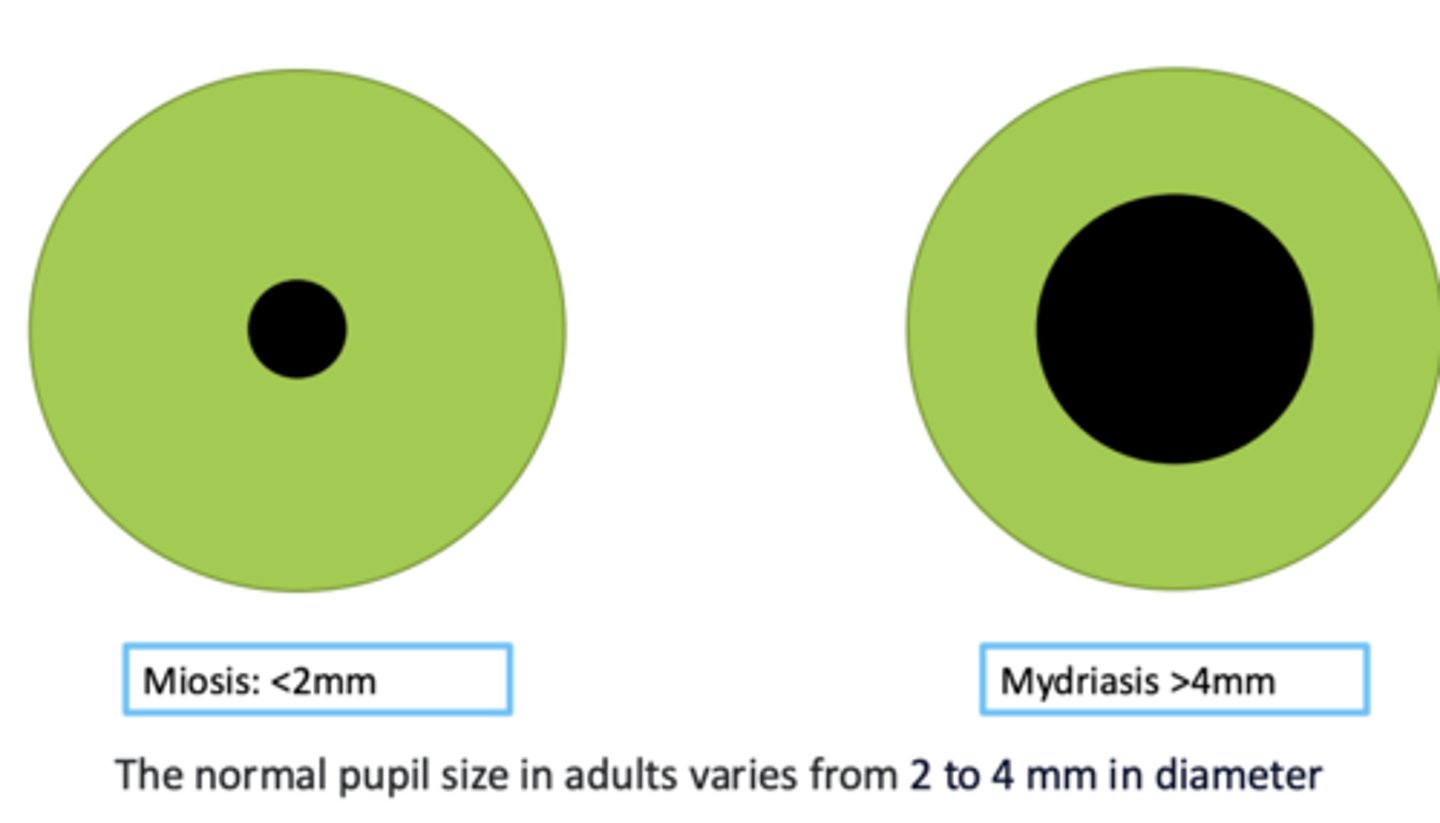
Normal adult pupil size (2-4 mm) miosis vs. mydriasis
Miosis: <2mm
Mydriasis: >4mm
- the normal pupil size in adults varies from 2-4 mm in diameter
A person with a heart rate of 90 bpm is experiencing...
A. Bradycardia
B. Tachycardia
C. Normal heart rate
D. Hypotension
C. Normal heart rate
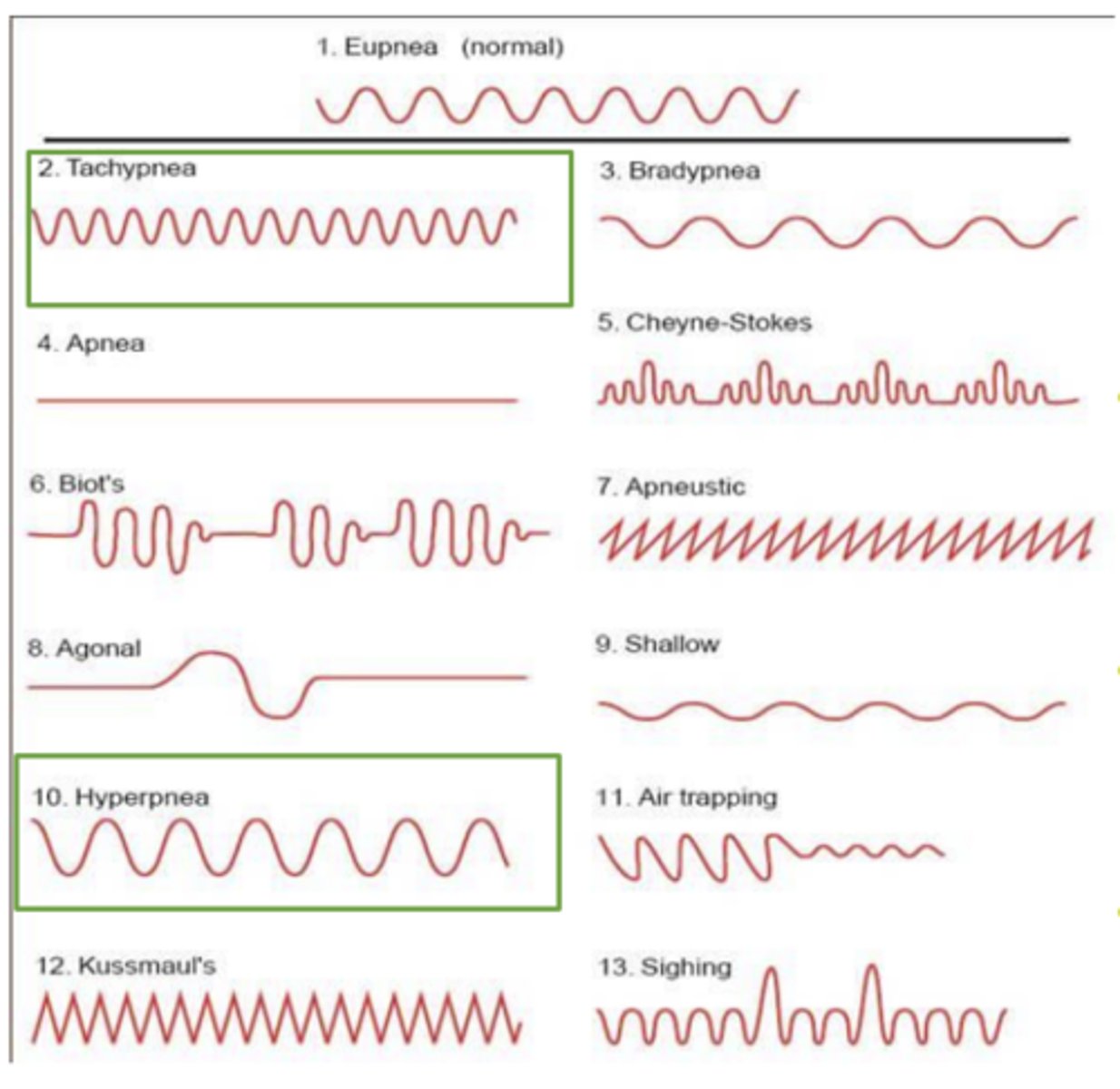
If a chart indicates the patient has bradypnea, what vital sign would you expect to find altered in this patient?
A. Heart rate
B. Blood pressure
C. Respirations
D. Temperature
C. Respirations
If a chart indicates the patient has bradypnea, what would you expect to find in this patient? (Select all that apply)
A. Respirations: 10 rpm
B. Respirations: 11 rpm
C. Respirations: 12 rpm
D. Respirations: 24 rpm
A. Respirations: 10 rpm
B. Respirations: 11 rpm
Hypotension
• Decreased _____________ resistance
• Decreased myocardial ______________
• Dys________
• Depletion of ________________________
• Decreased peripheral vascular resistance
• Decreased myocardial contractility
• Dysrhythmias
• Depletion of intravascular volume (hypovolemia)
Hypertension
• CNS sympathetic _____________
• Increased myocardial __________________
• Increased _________________________ resistance
• A combination
• CNS sympathetic overactivity
• Increased myocardial contractility
• Increased peripheral vascular resistance
• A combination
A pressure of 110/70 mm Hg would usually be normal but could also indicate hypotension if........
past pressures have been high
What is pulse rate the net result of?
net result of a balance between sympathetic (adrenergic) and parasympathetic (muscarinic and nicotinic) tone
There is a direct correlation between pulse rate and temperature, in the pulse rate increases approx. ________________ for each _________ elevation in temperature
- 8 beats/min
- 1.8°F (1°C)
T/F: The pulse rate is the result of a balance between sympathetic and parasympathetic systems
TRUE
Although respirations are typically assessed initially for _______ alone, careful observation of the ________ and ____________ is essential for establishing the _________________________
- rate
- depth and pattern
- etiology of toxicity
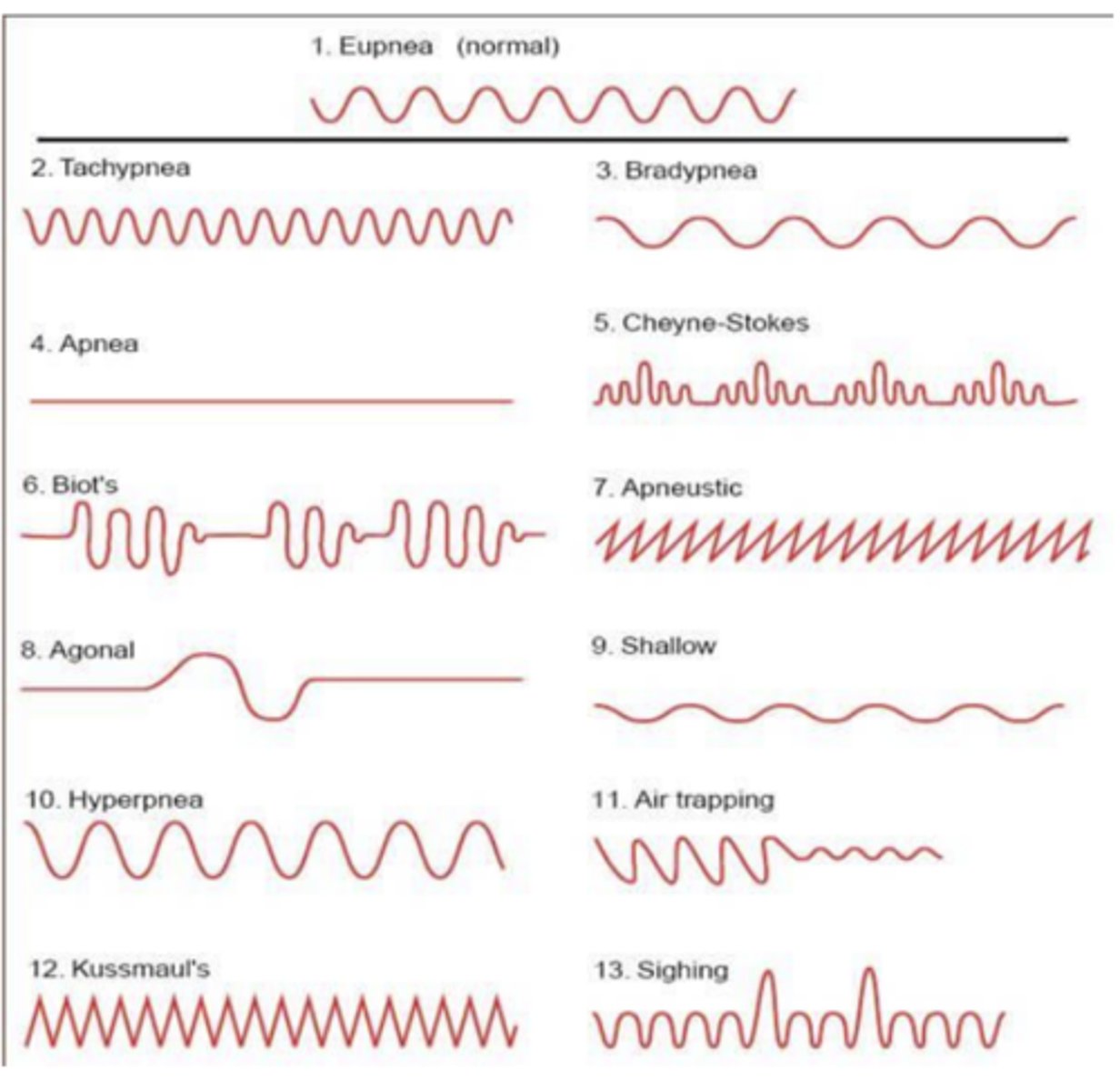
Hyperventilation may mean....
◦ tachypnea- an increase in ventilatory rate
◦ hyperpnea- an increase in tidal volume
Pulmonary injury from any source, including _____________ of gastric contents, may lead to __________ with a resultant __________________
- aspiration
- hypoxemia
- tachycardia
A patient with 28 respirations per minute is experiencing....
A. Hyperpnea
B. Tachypnea
C. Tachycardia
D. Hypopnea
A. Hyperpnea
B. Tachypnea
Temperature evaluation and control are....
critical
The core temperature or deep internal temperature (T) is relatively stable under _________________________________
normal physiologic circumstances
Normal temperature
• 97.8° F to 99.1° F
• 36.5° C to 37.3° C
Hypothermia temperature
• T <95° F
• T <35° C
Hyperthermia temperature
• T >100.4° F
• T >38° C
Life-threatening hyperthermia range****
• T >106° F
• T >41.1° C
What can life-threatening hyperthermia be associated with? (3)
- malignant hyperthermia
- serotonin toxicity
- neuroleptic malignant syndrome
Life threatening hyperthermia can further progress to....
- extreme rhabdomyolysis
- myoglobinuric kidney failure
- direct liver and brain injury
Fever
A regulated rise in body temperature due to a reset of the hypothalamic set point, usually in response to infection or inflammation
Causes of fever (3)
- infection
- autoimmune disease
- malignancy
Mechanism of fever
Immune system triggers prostaglandins → hypothalamus increases set point → body raises temp
Do fevers respond to antipyretics
Responsive (e.g., acetaminophen lowers temp)
Clinical clues of fever (3)
- gradual onset
- chills
- sweating
Hyperthermia
An uncontrolled rise in body temperature due to failed heat regulation, the hypothalamic set point stays normal
Causes of hyperthermia (2)
- heat stroke
- drug toxicity (NMDA, NMS, serotonin syndrome, anticholinergic toxicity)
Mechanism of hyperthermia
Body produces or retains more heat than it can dissipate; loss of thermoregulatory control
Is hyperthermia responsive to antipyretics?
Not responsive
Clinical cues of hyperthermia
Sudden and extreme temperature rise; altered mental status
T/F: Hypothermia is probably less of an immediate threat to life than hyperthermia
TRUE
Hypothermia is probably less of an immediate threat to life than hyperthermia, but it requires _______________, ________________, and ____________________
- rapid appreciation
- accurate diagnosis
- skilled management
What does hypothermia impair the metabolism of?
What does this lead to?
- impairs the metabolism of many xenobiotics
- leads to unpredictable delayed and/or prolonged toxicologic effects when the pt is warmed
What do many xenobiotics lead to?
What does this put patients at great risk for?
- lead to an alteration of mental status
- great risk for becoming hypothermic from exposure to cold climates
A 43-year-old man was brought to the ED, after being found on the ground next to a vegetable patch. He has white powder on his face and clothing. During the physical exam, he began vomiting
- Vital signs: T: 34.9°C, HR: 53 bpm, R: 25 rpm, BP: 110/75 mm Hg, SPO2: 85%
- He exhibits gurgling respirations with pooled secretions in the oropharynx
- Pupils 2mm Skin cool and diaphoretic
Which one of the following can you identify in this patient?
A. Hypotension & hyperthermia
B. Tachycardia & hypotension
C. Hypothermia & bradycardia
D. Hypotension & bradypnea
C. Hypothermia & bradycardia
hypothermia: <35° C
bradycardia: less than 60-100 bpm
A 21-year-old-woman was found unresponsive in her dorm by her roommate. Empty pill bottles standing next to her bed.
- Vital signs: T: 36.7 °C, HR: 72 bpm, RR: 4 rpm, BP: 60/50 mm Hg, SPO2: 81%
- Pupils 1mm
- Skin cyanotic but dry
Which one of the following can you identify in this patient?
A. Hypotension & hyperthermia
B. Tachycardia & hypotension
C. Hypothermia & bradycardia
D. Hypotension & bradypnea
D. Hypotension & bradypnea
hypotension: less than 90/60
bradypnea: less than 12-18 rpm
A 35-year-old man with depression was found altered at home by his spouse. Over-the-counter-pill bottles were found in the trash. Patient is alert but agitated and combative
- Vital signs: T: 38.6 °C, HR: 127 bpm, RR: 17, BP: 156/98, SPO2: 99%
- Pupils: 8mm
- Skin flushed and dry
- Dry mucous membranes
Which of the following is not true about this patient?
A. He has hyperthermia
B. He is experiencing tachycardia
C. He has hypertension
D. He is experiencing tachypnea
D. He is experiencing tachypnea
tachypnea: he is within 12-18 rpm, so he is not experiencing this
Many xenobiotics affect the autonomic nervous system, which affects the vital signs via....
sympathetic pathway, parasympathetic pathway, or both
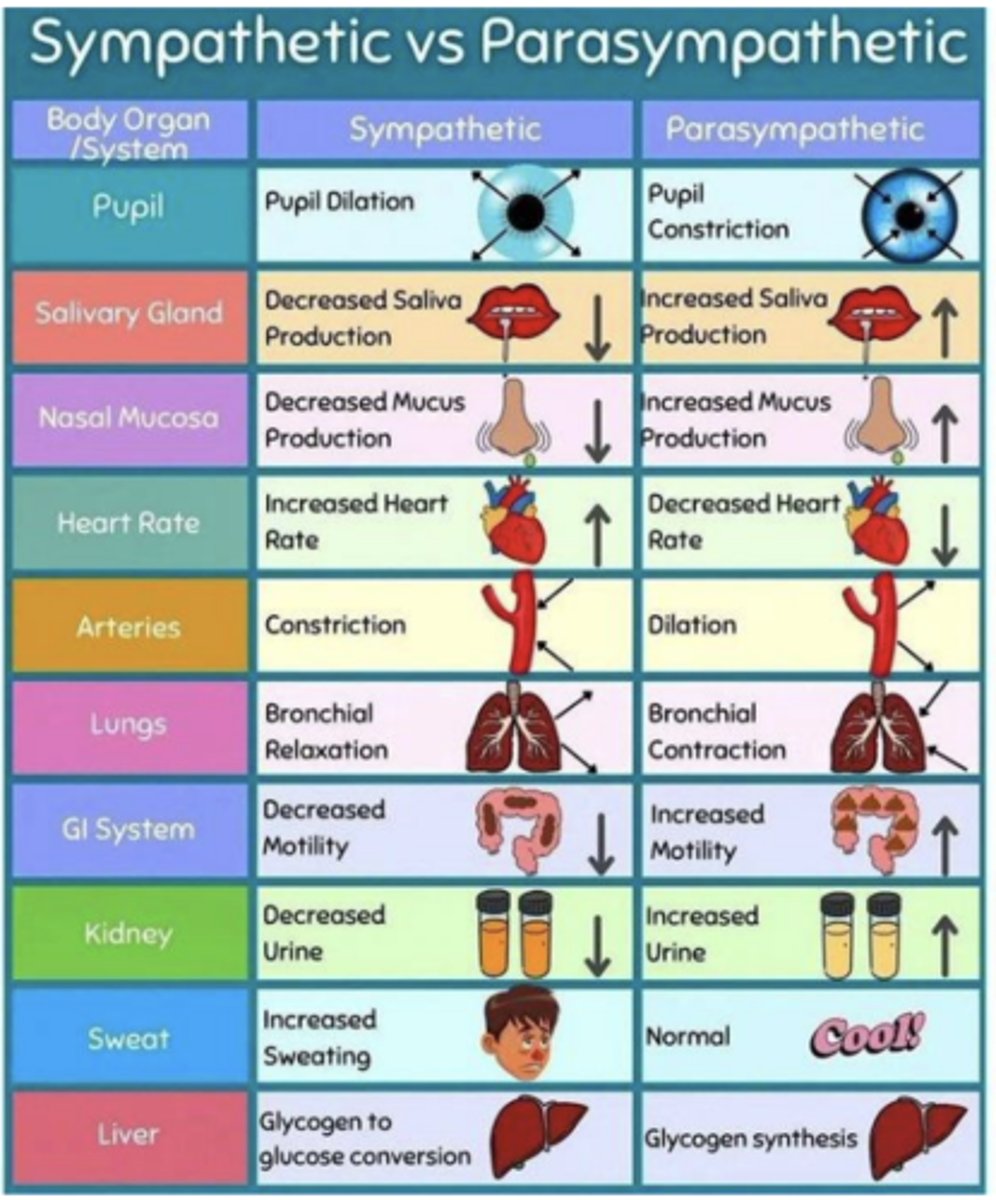
T/F: Meticulous attention to both the initial and repeated determinations of vital signs is of extreme importance in identifying a pattern of changes suggesting a particular xenobiotic or group of xenobiotics
TRUE