Adaptive Immunity
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
Immunity
The ability to resist damage or change from foreign substances such as microorganisms and harmful chemicals
Two important traits of Adaptive Immunity
Specificity & Memory
Specificity
Ability to recognize a particular substance
Memory
Ability to remember previous encounters with a particular substance and respond rapidly
Adaptive Immunity
Involves the ability to recognize, respond to, and remember a particular substance
Antigens
Large cell membrane bound molecules: self or non-self
Foreign Antigens (Non-self)
Not produced by body, introduced from outside. Bacteria, viruses, and other microorganisms that cause disease
Self-Antigens
Produced by body. Used as markers to allow adaptive immune response to differentiate self from non-self. Response to self-tumor antigens helpful. Response to self-antigens resulting in tissue destruction; auto immune diseases
MHC Molecules
Major Histocompatibility Complex Molecules
Antigens produced inside the cell. Proteins produced through genetic expression and protein synthesis
Endogenous antigens
Antigens processed from outside a cell. Substances obtained from the external environment, usually by phagocytosis and then broken down into cytoplasm
Exogenous antigens
MHC I Molecules
Display endogenous antigens; found on nucleated cells; function as a “red flag” to prompt immune cells to destroy the displaying cells
MHC II Molecules
Display exogenous antigens received from antigen-presenting cells such as B cells and macrophages
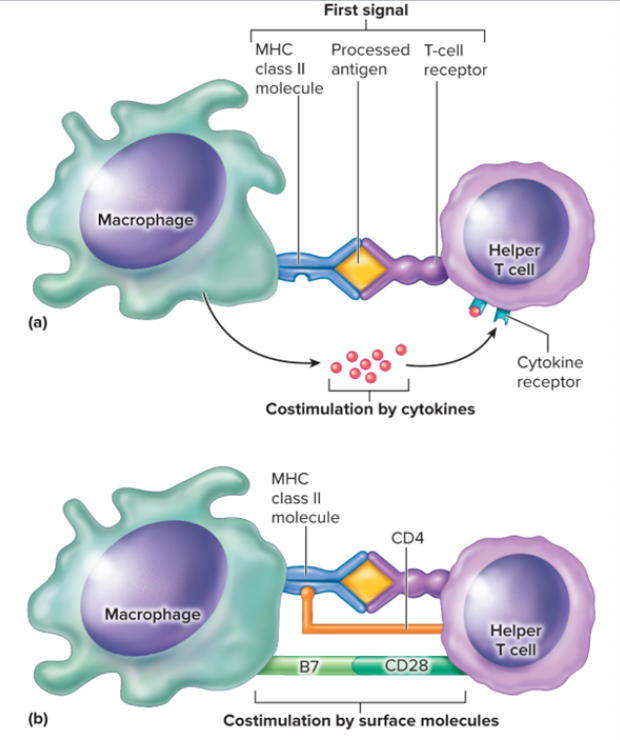
Costimulation
In order for B and T cells to produce a response there must be the binding of the MHC class complexes to an antigen and a T cell receptor and costimulation. Costimulation is the secondary signal besides the MHC’s that are necessary to activate lymphocytes
How is costimulation accomplished?
Accomplished by cytokines released from cells as well as molecules attached to the surface of cells. Cytokines produced by lymphocytes are often called lymphokines
Active Immunity
Immunity is provided by the individual’s own immune system
Natural Active Immunity
Antigens are introduced through natural exposure
Natural Artificial Immunity
Antigens are deliberately introduced in a vaccine
Passive Immunity
Immunity is transferred from another person or an animal
Natural Passive Immunity
Antibodies from the mother are transferred to her child across the placenta or in breast milk
Artificial passive immunity
Antibodies produced by another person or an animal are injected
MHC Class I molecules and Endogenous Antigen Processing
§ 1. When a virus reproduces inside a cell, viral proteins are produced within the cell
§ 2. Some of these viral proteins are broken down in the cytoplasm
§ 3. The protein fragments enter the rough ER and combine with MHC Class I molecules to form complexes
§ 4. The MHC Class I/antigen complex then move through the Golgi apparatus to be further transported to the plasma membrane
§ 5. MHC Class I/antigen complexes displayed on the cell’s plasma membrane can bind to T-cell receptors
§ 6. This combination is a signal that activates T cells. Activated T cells can destroy infected cells
MHC Class II Molecules and Exogenous Antigens
§ 1. Antigen-presenting cells can take in foreign antigens by endocytosis
§ 2. Within the cell, the antigen is broken down into fragments to form processed antigens
§ 3. Vesicles from the Golgi apparatus containing MHC class II molecules combine with the endocytotic vesicles. The MHC Class II molecules and processed antigens combine
§ 4. The MHC class II/antigen complexes are transported to the plasma membrane, where they are displayed to other immune cells
§ 5. The displayed MHC class II/antigen complex can stimulate immune cells
Cell-Mediated Immunity
§ Responds to intracellular antigens
§ Performed by immune cells: T-Lymphocytes
§ Ex: Cytotoxic T cells: destroy infected cells
§ Helper T cells and regulatory T cells – promote or inhibit both antibody-mediated and cell-mediated immunity
§ Most effective against cytoplasmic microbes through the action of cytotoxic T cells responding to endogenous antigens
Antibody Mediated Immunity
§ Responds to extracellular antigens
§ Performed by antibodies: produced by B – lymphocytes
§ Involves the production of antibodies in response to extracellular antigens. Exposure to the antigens can lead to activation of B cells and then the production of antibodies that destroy the antigen
§ Effective against extracellular antigens including bacteria, viruses, protozoans, fungi, parasites, and toxins when they are outside cells
§ Can also cause immediate hypersensitivity reaction i.e. Allergic reactions
Types of T cells
Cytotoxic T, Helper T, Regulatory T, Memory T cells
Cytotoxic T cells
Responsible for cellular immunity when activated, divide and differentiate into T cells that will participate in the immune response or into memory cells; destroy “bad” cells by releasing chemicals to trigger lysis
Helper T cell
Coordinates both T and B cells; releases chemicals to guide both immune cells and nonspecific defenses; activates B cells
Regulatory T cell
Inhibits B cells, helper T cells, and cytotoxic T cells
Memory T cell
Quick and effective response to an antigen against which the immune system has previously reacted; responsible for adaptive immunity
Cell-Mediated Immune Response: Helper T cells
§ 1. An antigen presenting cell, such as a macrophage, engulfs, processes, and displays an antigen on its plasma membrane by way of an MHC Class II molecule
§ 2. A helper T cell interacts with the macrophage through its T-cell receptor
§ 3. Costimulation occurs by a CD4 glycoprotein of the helper T cell or by cytokines
§ 4. Cytokines stimulates the helper T cell to secrete new cytokines (Interleukin-2) and produce more receptors
§ 5. The helper T cell stimulates itself to divide when these receptors are stimulated
§ 6. The “daughter” helper T cells can be stimulated to divide again if they are exposed to the same antigen that stimulated the “parent” cell. This greatly increases the number of helper T cells specific to this antigen
§ 7. The increased number of helper T cells can facilitate the activation of B cells or cytotoxic T cells
§ 8. Some daughter cells will become memory helper T cells, which become active in future encounters with the same antigen
Cell-Mediated Immune Response: Cytotoxic T cells
§ 1. When viruses infect cells, some viral proteins are broken down and become processed endogenous antigens that are combined with MHC class I molecules and displayed on the surface of the infected cells
§ 2. T cells can distinguish between virally infected cells and noninfected cells because MHC class I/antigen complexes are on the surface of infected cells, but not on the surface of uninfected cells
§ 3. Binding of the T-cell receptor to the MHC class I/antigen complex is a signal for activating cytotoxic T cells
§ 4. Costimulation by other surface molecules also occurs
§ 5. Helper T cells provide costimulation by releasing cytokines, such as interleukin-2, which activates cytotoxic T cells
§ 6. The activated cytotoxic T cell divides, the resulting daughter cells divide and so on, eventually producing many cytotoxic T cells
Stimulation and Effects of T cells - Memory T cells
§ After T cells are activated by an antigen on the surface of a target cell, they undergo a series of divisions to produce cytotoxic T cells and memory T cells
§ Memory T cells can provide a secondary response and long-lasting immunity in the same fashion as memory B cells
§ One effect of cytotoxic T cells is the destruction of target cells. Cytotoxic T cells can come into contact with other cells and cause them to lyse
Antibody Mediated Immunity: B-Cell Production
§ 1. Before a B cell can be activated by a helper T cell, the B cell must take in and process the same antigen that activated the helper T cell. The antigen binds to a B-cell receptor, and both the receptor and the antigen are taken into the cell by endocytosis
§ 2. The B cell uses an MHC class II molecule to present the processed antigen to the helper T cell
§ 3. Costimulation of the B cell occurs through surface molecules, such as CD4, as well as through the release of interleukins (cytokines) by the helper T cell
§ 4. The B cell divides, and the resulting “daughter” B cells divide, and so on, eventually producing many B cells that recognize the same antigen
§ 5. Many of the daughter cells differentiate to become plasma cells, which produce antibodies. Antibodies are part of the immune response that eliminates the antigen
§ 6. Daughter cells that do not differentiate to become plasma cells reduce in size and become memory B cells. Memory B cells may become active in future encounters with same antigen
Antibody
Proteins produced by B cells that became plasma cells in response to an antigen. Sometimes called gamma globulins or immunoglobulins (Ig)
Structure of antibody
Y-shaped consisting of four polypeptide chains – two identical heavy chains and two identical light chains
Variable Region of Antibody
Part that combines with antigenic determinant of antigen
Constant Region of Antibody
Responsible for activities of antibodies like activating complement or attaching to various kinds of WBCs
Direct Effects of Antibodies
§ The antibody can bind to the antigen and interfere with the antigen’s ability to function
§ The antibody can combine with an antigen on two different antigens, rendering the antigens ineffective
§ The ability of antibodies to join antigens together is the basis for many clinical tests such as blood typing, because, when enough antigens are bound together, they become visible as a clump or a precipitate (Agglutination)
Indirect Effects of Antibodies
§ When an antibody combines with an antigen, it can activate the complement cascade through the classical pathway
· Activated complement stimulates inflammation; attracts neutrophils, monocytes, macrophages, and eosinophils to sites of infection and kills bacteria by lysis
§ Antibodies can initiate an inflammatory response. The antibodies attach to mast cells or basophils, which then release chemicals, and inflammation results
· Ex: Hay fever; You inhale antigens (usually plant pollen), which are then absorbed through the mucous membrane. The combination stimulates mast cells to release inflammatory chemical (histamine)
§ Opsonins are substances that make an antigen more susceptible to phagocytosis. An antibody acts as an opsonin by connecting to an antigen and to a macrophage. The macrophage then phagocytizes the antigen and the antibody
Opsonins
substances that make an antigen more susceptible to phagocytosis. An antibody acts as an opsonin by connecting to an antigen and to a macrophage. The macrophage then phagocytizes the antigen and the antibody
Antibody Production: Primary Response
§ Primary Response: The primary response occurs when a B cell is first activated by its specific antigen.
§ The B cell proliferates to form plasma cells and memory cells. The plasma cells produce antibodies
§ The primary response normally takes 3-14 days to produce enough antibodies to be effective. Disease symptoms generally develop.
Antibody Production: Secondary Response
§ Secondary response: The secondary response or memory response, occurs when another exposure to the same antigen causes the memory cells to rapidly form plasma cells and additional memory cells
§ The secondary response is faster and produces more antibodies than the primary response
§ Generally, the person does not get sick. Memory B cells can persist for many years, even a lifetime