A&P2- Lecture exam 2 review
1/162
Earn XP
Description and Tags
10/13/24- COMPLETED -X
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
163 Terms
List the functions of blood
Transport (nutrients, gases, waste, hormones)
Protection (clotting, white blood cells and platelets)
Regulation (body temp, blood pressure, salt concentration, blood volume)
What is the composition of blood?
Plasma (55% of blood volume.)
formed elements (45% of blood volume.)
What is blood?
A type of liquid connective tissue containing cells and cell fragments.
What does blood transport?
Nutrients
hormones
gases
wastes
metabolites
antibodies
How long do RBCs last in circulation?
110-120 days in circulation. they then rupture (hemolysis). The hemoglobin in plasma is broken down by macrophages.
What is the function of red blood cells?
To transport oxygen from lungs to tissues. 98.5% of oxygen is attached to hemoglobin; 1.5% is dissolved in plasma.
To transport carbon dioxide from tissues to lungs
7% is dissolved in plasma
23% combines with hemoglobin
70% is transported as bicarbonate ions produced as a result of combination of H20 and CO2. This is due to enzyme carbonic anhydrase found within RBCs.
What is the structure of RBCs?
Biconcave disc shape, 7.5 um in diameter
Mature RBCs are anucleate, meaning they don’t have a nucleus
Flexible and capable of bending/folding, allowing them to pass through small vessels and move with blood flow.
RBCs contain hemoglobin, lipids, ATP, and carbonic anhydrase.
Where do RBCs go specifically to hemolyze?
Spleen and liver. there they rupture and their contents are processed.
What is plasma and what is it mainly composed of?
Plasma is the liquid matrix of blood. It is a colloid. It is composed of:
91% water
remaining proteins, ions, nutrients, waste products, gases, and regulatory substances.
Composition remains relatively constant through various homeostatic mechanisms even though materials are constantly moving into and out of the blood.
plasma mainly moves what?
Hormones, wastes, nutrients, metabolites
Plasma controls
blood pressure and blood volume
What is the pH of blood?
7.35-7.45
What helps plasma function?
Proteins. they are:
Albumin (58% of proteins) (creates osmotic pressure, very important)
Globulin (38% of proteins) (binding protein for transport in blood)
Fibrinogen (4% of proteins) (inactive) (helps with clotting)
They are all made in liver hepatocytes
Name the three different types of specific globulins in plasma. Know their function.
Alpha globulin- protects tissues from inflammation damage. Also transports thyroid hormones, cortisol, testosterone, estrogen, and lipids (HDL). Transports hemoglobin released from damaged RBCs.
Beta globulin- transports iron, lipids (LDL), involved with complement in immunity and coagulation proteins.
Gamma globulin- involved in immunity with circulating antibodies.
What comprises the formed elements in blood?
Red blood cells (erythrocytes)- 95% of the volume of formed elements
White blood cells (leukocytes)
Platelets (thrombocytes)- cell fragment. form platelet plugs and release chemicals necessary for blood clotting.
What are the two types of generic white blood cells?
Granulocytes- Cytoplasm contains large granules and have multi-lobed nuclei. There are three distinctive types: neutrophils, eosinophils, and basophils. (HINT: all granulocytes have -phil at the end)
Agranulocytes- Cytoplasm contains small granules and nuclei that are not lobed. there are two distinctive types: lymphocytes and monocytes.
what are the 5 types of white blood cells?
Neutrophils (stereotypical leukocyte)
lymphocytes (produces antibodies and other chemicals to help destroy microorganisms)
monocytes (becomes macrophages once it leaves the blood, used for phagocytosis, the ingestion of other cells)
eosinophils (fights parasitic infection, eats parasites)
Basophils (create signals for inflammation, make histamines to warn other WBCs of infections)
Define Hematopoiesis (also known as hemopoiesis)
The process of blood cell formation. It occurs in red bone marrow and lymphatic tissue.
All formed elements are derived from a single population of?
Hemocytoblasts
What do hemocytoblasts differentiate into?
either a myeloid stem cell or a lymphoid stem cell.
When hemoglobin breaks down, what can heme be broken down into?
Heme can be broken down into bile and bilirubin. In bile, stercobilin give feces its brown color. In urine, urochrome gives urine its yellow color.
When hemoglobin breaks down, what can the globin chains be broken down into?
Amino acids used to make other proteins for reuse.
What transports iron in the blood?
Ferritin
Define anemia
Lack of oxygenated blood. Meaning low oxygen.
Define hemostasis
The fast series of reactions for stoppage of bleeding to maintain homeostasis.
how much blood is in the human body?
Male average= 5-6L
Female average= 4-5L
what is the buffer of blood?
Bicarbonate
leukocytosis
An increase of white blood cells in the blood. Could indicate the body is fighting an infection or inflammation.
Erythropoiesis
formation of red blood cells. It takes approx. 4 days and uses EPO.
Diapedesis
Cells leave the blood stream by becoming thin, elongating and move either between or through endothelial cells of capillaries. This applies to white blood cells only.
Chemotaxis
attraction to and movement toward foreign materials or damaged cells. Accumulation of dead white cells and bacteria is pus.
Ameboid movement
How WBCs move through tissues. similar to amoeba.
leukocytopenia
A reduction of white blood cells in the blood.
What are the three types of adult hemoglobin?
Oxyhemoglobin- Iron in hemoglobin bound to oxygen; 4 per molecule of hemoglobin; bright red in color.
Deoxyhemoglobin- Hemoglobin not bound to oxygen; dark red.
Carbaminohemoglobin- globin of hemoglobin is bound to carbon dioxide.
What is the function of nitric oxide in the blood?
NO causes the relaxation of smooth muscles in blood vessels to decrease blood pressure.
What does carbon monoxide do to RBCs’ hemoglobin?
CO binds very strongly to the iron of hemoglobin to form carboxyhemoglobin, which means less oxygen is being transported.
Define platelets
The smallest of all the formed elements. they are cell fragments pinched off from megakaryocytes in red bone marrow. In inactive forms, they look like plates. In active forms, they look spiky. They stick to collagen.
What is the lifespan of a platelet?
5-9 days
What is the function of a platelet?
Prevents blood loss by formation of platelet plugs
promotes formation and contraction of clots
Clotting factors
a substance released by platelets and injured tissues. They are mostly enzymes and are made in their inactive form in the liver.
Vitamin K and calcium are important for what?
The clotting of blood.
Which blood vessels can white blood cells pass through only?
capillaries
What are the three steps involved in hemostasis?
Vascular spasm
platelet plug formation
Coagulation (blood clotting)
Failure of any of these steps will result in hemorrhage- excessive bleeding.
Define vascular spasm
The first step of hemostasis. occurs when a wall of a vessel is damaged, hence constricting the vessel. This stops or slows blood flow. This response is triggered by chemicals called endothelin which is released by damaged endothelial cells.
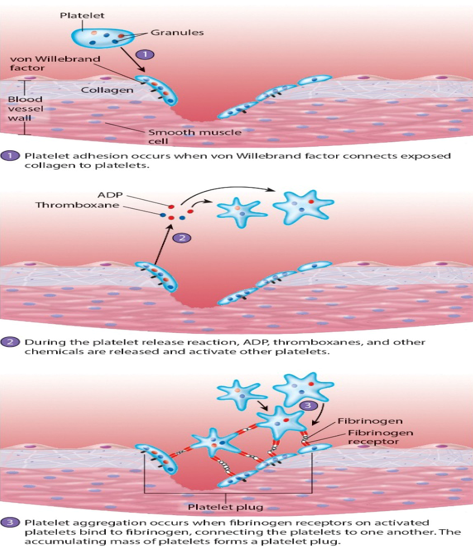
Define Platelet plug formation
The second step of hemostasis. The steps of this formation is as follows:
The freely floating platelets encounter the area of vessel rupture with exposed connective tissue – collagenous fibers
Platelet adhesion: Platelets begin to clump and become spiky and sticky - bind to collagen from damaged vessel (process mediated largely by von Willebrand factor secreted by endothelial cells.)
Activation of platelets: occurs after platelets have adhered, platelets initiate platelet release reaction. (Release of ADP and thromboxanes, which activate the platelets and allow for adhesion.)
Platelet aggregation: platelets adhere to fibrinogen and to one another, creating platelet plug
Define coagulation
The third step of hemostasis. the process reinforces platelet plug with fibrin threads with cells and cell fragments trapped. Blood is then transformed from liquid to gel during clotting. This process requires many substances like calcium, platelets, vitamin K, and clotting factors. This process occurs in three phases.
What are the three phases of coagulation?
Initiation can occur in two ways; Extrinsic pathway and intrinsic pathway
Extrinsic pathway: which normally is triggered by outside trauma on the wall of a vessel.
Intrinsic pathway: which begins in the bloodstream and is triggered by internal damage to the wall of the vessel.
Pathway to thrombin: Once factor X is activated the enzyme prothrombinase converts prothrombin (factor II) to activate enzyme thrombin.
Common pathway to the fibrin mesh:
Thrombin converts soluble fibrinogen (factor I) to fibrin.
Fibrin strands form structural basis of clot
Plasma becomes a gel-like trap, catching formed elements
Thrombin (along with calcium ions) activates factor XIII (fibrin stabilizing factor which cross links fibrin and strengthens/stabilizes clot)
What is a thrombus?
A clot stationed in one spot. It does not travel.
How do anticoagulants work?
prevent coagulation factors from initiating clot formation.
What are some examples of anticoagulants?
Antithrombin: produced by liver and slowly inactivates thrombin.
Prostacyclin: Causes vasodilation and inhibits release of coagulating factors from platelets.
Outside sources: heparin, EDTA, and sodium citrate.
What is the importance of reticulocytes in the blood stream?
Reticulocytes in the blood stream show that red bone marrow is working correctly and that healthy blood can be maintained.
Define Erythropoietin (EPO)
A hormone released by the kidneys that stimulates red blood cell development. It is released in larger quantities during hypoxia.
Where is the iron that is used in heme found in?
Found and stored in the liver.
Thrombopoiesis
The generation of platelets from Megakaryocytes
Hemorrhagic anemia
Results from blood loss due to trauma, ulcers, or excessive menstrual bleeding.
Iron-deficiency anemia
Caused by insufficient intake or absorption of iron or by excessive iron loss; leads to reduced hemoglobin production.
Pernicious anemia
Secondary folate-deficiency anemia caused by inadequate amount of vitamin B12, which is important for folate synthesis. (Folate ensures RBCs are produced and mature correctly)
Renal anemia
Usually occurs in those with Chronic kidney disease. An unhealthy kidney cannot make enough EPO to maintain healthy production of RBCs. This leads to decreased RBC production and anemia.
Aplastic anemia
Caused by an inability of the red bone marrow to produce RBCs, usually as a result of damage to stem cells after exposure to certain drugs, chemicals, or radiation.
Sickle cell anemia
A genetic blood disorder which causes RBCs to become stiff and crescent shaped. RBCs with this disorder cannot efficiently deliver oxygen to the body’s tissues.
Polycythemia
a condition characterized by an abnormally high number of red blood cells (RBCs) in the bloodstream. This increase in RBCs thickens the blood, making it more viscous, which can slow blood flow and increase the risk of complications such as blood clots, strokes, and heart attacks.
Leukemia
Cancers of the red bone marrow in which one or more white blood cell types is produced; cells are usually immature or abnormal and lack normal immunological functions.
A thrombus that breaks away from a vessel wall is called?
An embolus. it may become dislodged in a small diameter vessel, also restricting blood flow.
(Fill in the blank) __________ such as aspirin, heparin, and warfarin, are clinically important to prevent undesirable clotting.
anti-coagulants
Thrombocytopenia
A reduction in the number of platelets that leads to chronic bleeding through small vessels and capillaries. Usually caused by genetics, autoimmune disease, infections, and decreased platelet production resulting from pernicious anemia, drug therapy, radiation therapy, or leukemias.
Hemophilia
A genetic disorder in which clotting is abnormal or absent; each of the several types results from deficiency or dysfunction of a clotting factor; most often a sex-linked trait that occurs almost exclusively in males.
Antigens
Large proteins that can trigger an immune response
Antibodies (also known as agglutinins)
produced by B lymphocytes. They attach to the antigens on the membrane of RBCs and cause them to clump, resulting in agglutination (clumping) or hemolysis (rupture) of RBCs.
ABO blood groups are designated based on the presence or absence of?
two antigens- A and B. EX. People with A antigen on the erythrocyte means they are type A. They also have anti-B antibodies for B antigen.
What are the types of Rh?
Rh-positive: rhesus antigen present on surface of RBCs
Rh-negative: do not have these antigens present.
Hemolytic disease of the newborn (HDN)
Rh-positive fetus, Rh-negative mother
This occurs late in pregnancy. Rh antigens of fetus cross placenta and the mother creates anti-Rh antibodies.
The second Rh-positive pregnancy might initiate secondary response and HDN (could be fatal to fetal RBCs)
Injection of RhoGAM is necessary to ensure any antibodies that attach to fetal RBCs are destroyed.
What does a CBC check? (Complete blood count)
Red blood count: # of RBCs/microliter of blood
Hemoglobin measurement: grams of hemoglobin/100mL of blood. for males, 14 to 17 g/100mL. For females, 12 to 15 g/100mL.
Hematocrit measurement: precent of blood that is RBCs; checks for normocytes, microcytes, and macrocytes.
White blood cell count: 4,500 to 11,000/mL of blood.
What does a differential white blood count measure?
the percentage of each of the five types of WBC. the normal values are:
Neutrophils: 55%-70%
Lymphocytes: 20%-40%
Monocytes: 2%-8%
Eosinophils: 1%-4%
Basophils: 0.5%-1%
What does a clotting assessment measure?
Platelet count: 150,000 to 400,000/mL of blood.
Prothrombin time measurement: measures how long it takes for blood to start clotting. typically 9-12 seconds. To test, thromboplastin is added to whole plasma.
What is blood chemistry?
The composition of materials dissolved or suspended in the plasma. Used to assess functioning of many body systems.
Which blood group is the universal recipient
AB+
Which blood group is the universal donor
O-
Ringer’s solution
a multiple-electrolyte solution that mimics plasma electrolyte composition.
What composes the heart?
it is composed of two pumps. Right side of the heart pumps blood through pulmonary circulation to lungs. Left side of the heart pumps blood through systemic circulation to remaining tissues of the body.
What are the functions of the heart?
Generating blood pressure by way of heart contractions.
Routing blood: separates pulmonary and systemic circulations.
Ensuring one-way blood flow by way of valves.
Regulating blood supply by changing heart rate and force of contraction depending on the metabolic needs of the tissues.
What is the size, average mass and location of the heart?
The heart is the size of a closed fist
Average mass: 250g in females and 300g in males
location: in the thoracic cavity in the mediastinum. 2/3rd of the heart’s mass lies to the left of the midline of the sternum.
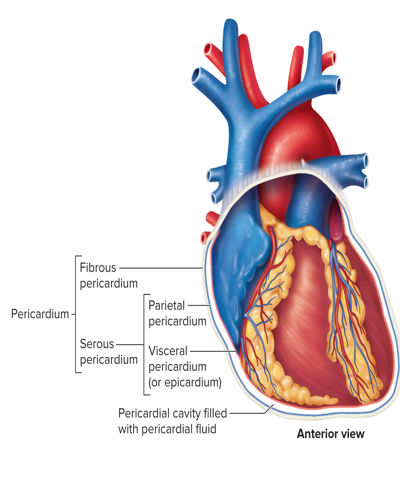
What is the location and structures of the pericardium?
Located around the heart and consists of two layers:
Fibrous pericardium- A tough fibrous outer layer. it prevents overdistention (excessive swelling/friction) and acts as an anchor.
serous pericardium- A thin, transparent, inner layer of simple squamous epithelium. it is further divided into:
Parietal pericardium: lines the fibrous outer layer
Visceral pericardium (epicardium): covers the heart surface.
These two layers are continuous and have a pericardial cavity between them filled with pericardial fluid.
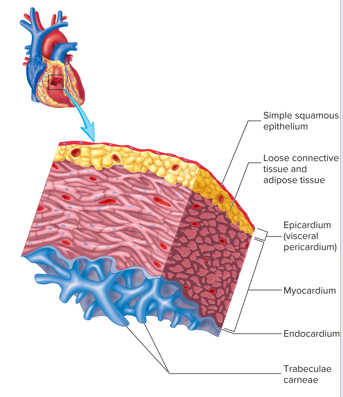
What are the three layers of the heart wall?
Epicardium- consists of the visceral pericardium, serous membrane, and simple squamous epithelium. It is the smooth outer surface of the heart.
Myocardium- Middle layer composed of cardiac muscle cells and is responsible for heart contraction.
Endocardium- smoother inner surface of the heart chambers. also consists of simple squamous epithelium.
Pectinate muscles
muscular ridges in auricles and right atrial wall
Trabeculae carneae
Muscular ridges and columns on the insides walls of ventricles.
The heart is composed of four chambers. What are they?
Two atria and two ventricles
Atria
The thin-walled chambers that forms the superior and posterior parts of the heart. It contains a flap like auricles that are considered extensions of this chamber. Their primary function is to receive blood from veins and expel the blood into the ventricles.
Interatrial septum
The wall between the atria. It contains a depression, the fossa ovalis, a remnant of the fetal opening between the atria. (foramen ovale)
Ventricles
The thick-walled chambers that from the anterior and inferior portions of the heart.
Anastomoses
connections between blood vessels to provide better blood flow.
Atrioventricular valves (AV valves)
Consists of two valves, each valve has leaf-like cusps that are attached to cone-shaped papillary muscles by chordae tendineae.
Tricuspid valve- Atrioventricular value between right atrium and right ventricle. Allows blood flow into the right ventricle.
Bicuspid valve (also known as Mitral valve)- Atrioventricular valve between left atrium and left ventricle. Allows blood flow into the left ventricle.
When valve is open, it creates a canal called atrioventricular canal.
Semilunar valves
Consists of two valves, each valve contains three picket like semilunar cusps
Pulmonary semilunar valve- Between right ventricle and pulmonary trunk. Allows blood flow into the pulmonary trunk.
Aortic semilunar valve- between left ventricle and aorta. Allows blood flow into the ascending aorta.
List the blood flow through the heart
Superior vena cava, inferior vena cava, and coronary sinus
Right atrium
Tricuspid valve
Right ventricle
Pulmonary semilunar valve
Pulmonary trunk
Pulmonary arteries (to the lungs)
pulmonary veins (back from lungs)
Left atrium
Bicuspid valve
Left ventricle
Aortic semilunar valve
aorta
Rest of the body
The cycle then repeats.
Where do coronary arteries originate from?
The ascending aorta
What are the structural characteristics and function of cardiac muscle?
striated, has intercalated discs and multiple nuclei. Functions in unison with one another, especially during contraction.
What are the two types of cardiac muscle cells?
Myocardial contractile cells (99% of the cells). These cells follow conducting cells to achieve systole.
Myocardial conducting cells (1% of the cells). These cells initiate systole.
They have a property known as auto-rhythmicity.
What is the cardiovascular system’s control center?
The Medulla Oblongata.
List the components of the conducting system of the heart in order.
Sinoatrial node (SA node)
Atrioventricular node (AV node)
AV bundle (also known as bundle of his)
Right and left bundle branches
Purkinje fibers
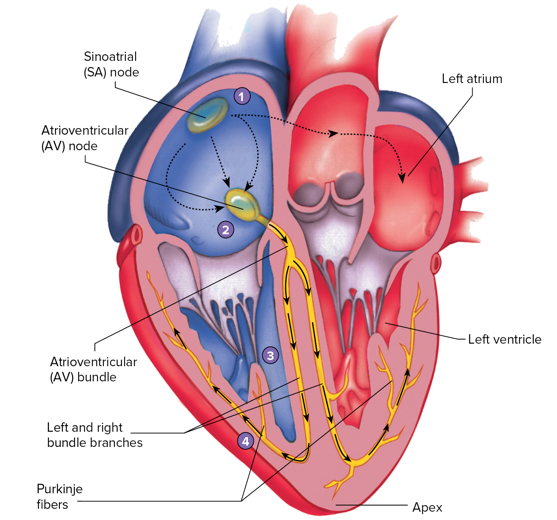
What is the pacemaker of the heart?
The SA node. it establishes normal cardiac rhythm known as sinus rhythm. Note that in sinus rhythm, beats per minute must be 60-100bpm with no skipped, early, or late beats.
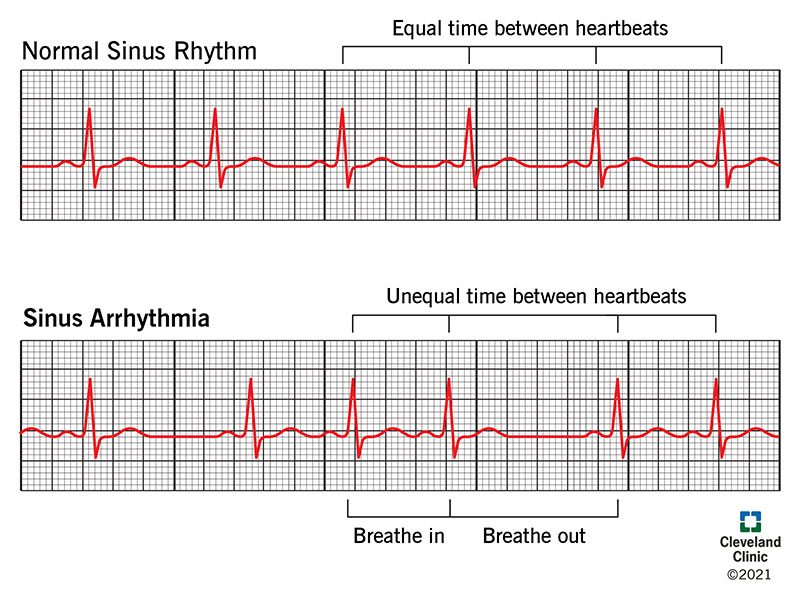
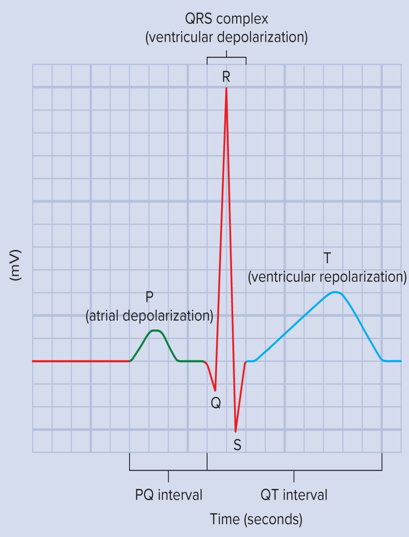
Define electrocardiogram (ECG or EKG)
A graphic recording of electrical activity in the heart. Sticky sticker-like electrodes are placed at various points on the body for the reading. It specifically records the electrical events in the myocardium which can be correlated with mechanical events in the heart.