FSC 451 Chapter 4 (Blunt Trauma Wounds)
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
What factors determine the severity and appearance of blunt trauma injuries?
Severity depends on (1) the amount of force, (2) the duration of force, (3) the region struck, (4) the area over which the force was applied, and (5) nature of the weapon
How does energy dispersion affect blunt trauma severity?
Greater surface area —> less severe injury; concentrated force over a small surface area —> more severe injury
How does weapon deformation affect injury severity?
If a weapon deforms or breaks, some energy is absorbed by the weapon, reducing injury severity.
What are the four categories of blunt force injuries?
Abrasions, contusions, lacerations, and fractures of the skeletal system.
What is an abrasion?
Removal of the superficial epithelial layer of skin due to friction or compression
How do antemortem and postmortem abrasions differ in appearance?
Antemortem abrasions are reddish-brown; postmortem abrasions appear yellow, translucent, and parchment-like.
What are the three types of abrasions?
Scrape (brush) abrasions, impact abrasions, and patterned abrasions.
What causes scrape abrasions?
Blunt force is applied perpendicular to the skin, crushing the epidermis; commonly over bony prominences.
What characterizes impact abrasions?
A blunt object scraping the skin, crushing the epidermis, commonly over bony prominences.
What is a patterned abrasion?
An abrasion that reproduces the pattern of the impacting object or intermediary material (eg clothing)
Can abrasions be historically dated?
Yes, to a degree, histology can estimate age based on healing stages.
What are the 4 stages of abrasion healing?
(1) scab formation, (2) epithelial regeneration, (3) subepidermal granulation, (4) regression/ remodeling
What is a contusion?
Hemorrhage into soft tissue due to ruptured blood vessels from blunt force.
What is a Hematoma?
A localized collection of blood within a contusion.
How can a contusion be distinguished from livor mortis?
In contusions, blood escaped into tissue and cannot be wiped away; livor mortis blood remains in vessels and may blanch.
What causes patterned contusions?
When the shape of the impacting object is reflected in the bruise pattern.
Cab contusions exist without visible skin bruising?
Yes—deep contusions may not be externally visible.
Why is dating contusions unreliable?
Color changes vary by individual, location, depth, and vascularity; timelines are inconsistent.
What causes color changes in bruises?
Hemoglobin breakdown causes progression from red/purple → blue → green → yellow.
Can contusions occur after death?
Rarely, but severe blunt force shortly after death can cause postmortem contusion-like hemorrhage.
What is a laceration?
A tear in tissue caused by shearing or crushing blunt force.
What do laceration margins typically look like?
Irregular, abraded, and contused margins.
What is tissue bridging, and why is it important?
Remaining blood vessels or nerves crossing the wound indicate a laceration, not an incised wound.
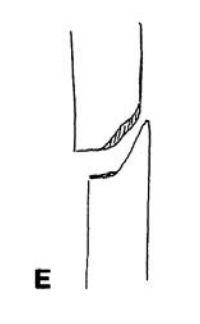
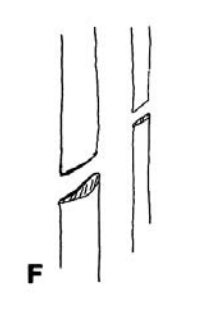
How does weapon shape influence laceration appearance?
Long, narrow objects cause linear lacerations; flat objects cause irregular or Y-shaped wounds.
How can direction of force be determined in lacerations?
Undermining occurs on the side opposite the direction of impact; beveled edges indicate force direction.
What is an avulsion injury?
A severe laceration where skin and soft tissue are forcibly torn away, sometimes exposing bone.
What are blunt-force defense wounds?
Abrasions, contusions, or fractures on hands, wrists, forearms from attempts to block blows.
How is antemortem vs postmortem injury determined?
Antemortem injuries may show bleeding into tissues, indicating circulation at the time of injury, but postmortem trauma can sometimes also cause bleeding (e.g., vitreous aspiration). Microscopic examination for inflammatory response is another method, though inflammation requires survival time after injury.
What biochemical markers suggest an antemortem wound?
Antemortem wounds may show increased enzyme activity at the wound periphery, decreased activity at the center, and elevated histamine, serotonin, DNA, and C3 complement. Enzyme activity can persist up to 5 days after death.
What are the 5 categories of maxillary fractures?
Dentoalveolar
Le Fort I
Le Fort II
Le Fort III
Sagittal
What characterizes Le Fort I, II, and III fractures?
Le Fort I: Horizontal fracture above the teeth apices
Le Fort II: Pyramidal fracture through the nasal bridge and orbits
Le Fort III: Craniofacial separation involving zygomatic arches and orbits
What causes fractures from direct application of force?
A blunt object impacts the bone, causing tension-side cracking opposite the impact and compression at the same impact site. Severe force may produce crushing and fragmentation into multiple pieces.
What are penetrating, focal, and crush fractures?
Penetrating: High force over a small area (e.g. gunshot wounds)
Focal: Small Force over small area; usually transverse
Crush: large force over large area with extensive soft tissue damage.
What are “Bumper fractures”?
Fractures of the lower extremities, especially the legs, caused by motor vehicle-pedestrian collisions, are commonly involving crush mechanisms.
How are indirect fractures different from direct fractures?
Indirect fractures occur away from the impact site due to transmitted forces. Bone is weaker under tension than compression, making indirect fractures common.
What are the six types of indirect fractures?
Traction
angulation
rotational
vertical compression
Angulation+ compression
Angulation +rotation+ compression
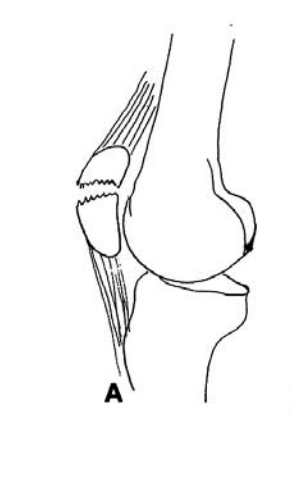
Indirect fractures Traction
the bone is pulled apart by traction. An example would be violent contraction of the quadriceps muscle with resultant transverse fracture of the patella.
Indirect fractures Angulation
In angulation fractures, the bone is bent until it snaps. The concave surface is compressed, and the convex surface is put under traction. This usually results in a transverse fracture
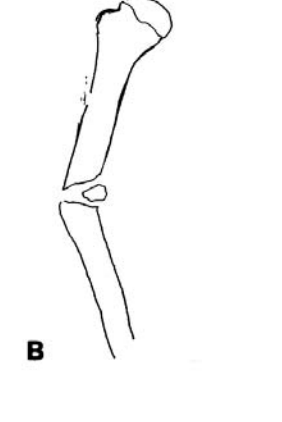
indirect fractures Rotational
In rotational fractures, the bone is twisted and a spiral fracture is produced. Spiral fractures occur only when the bone is subjected to torsional force. In the femur, most spiral fractures occur in the proximal third. The proximal and distant ends of a spiral fracture are connected by what Porta et al. call a “hinge.”8 The hinge distinguishes it from an oblique fracture. To determine in which direction a bone was twisted, ascertain the direction the spiral runs from the end twisted. This indicates the direction of torque.
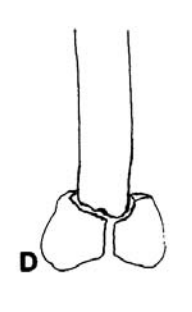
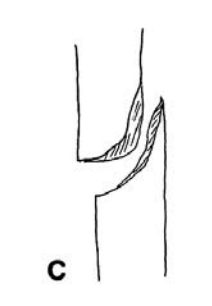
Indirect fractures Vertical compression
Vertical compression fractures produce an oblique fracture of the body of long bones, with the hard shaft of the long bone driven into the cancellous end. In femurs, a T- or Y-shaped fracture is typically seen at the distal end of the femur. Such fractures may occur following impaction of the end of the femur into the instrument panel in motor vehicle crashes.
Indirect fractures Angulation + compression
In angulation and compression fractures, the fracture line is curved, with an oblique component due to compression, and a transverse component due to angulation.
Indirect fractures Agulation + rotation + compression
The angulation plus rotation produces an oblique fracture, with the compression increasing the tendency toward fracture.
What produces spiral fractures?
Rotational (torsional) force twisting the bone, commonly seen in femurs. Direction of the spiral indicates direction of applied torque.
What are pelvic fracture categories?
anterior-posterior compression
lateral compression
shear
complex fractures
pelvic fracture anterior-posterior compression
In fractures due to antero-posterior compression, there is a direct blow to either the pubic symphysis or the posterior iliac spines, or violent external rotational forces applied to the femurs. Anteriorly, there is separation of the pubic symphysis. Posteriorly, there is bilateral separation of the sacroiliac joints anteriorly, with the posterior iliac ligaments generally intact
pelvic fracture lateral compression
In lateral compression, the force is applied either to the iliac crest directly or to the greater trochanter by the femoral head’s being propelled into the acetabulum. Anteriorly, the pubic rami on the side of impact are usually fractured. However, there may be contralateral fracture of the pubic rami or, less commonly, fracture of all four pubic rami or even disruption of the pubic symphysis. Posteriorly, there is ipsilateral impaction of the sacroiliac joints with the posterior ligaments generally intact. If the femoral head produces lateral compression by being propelled into the acetabulum, there are usually ipsilateral fractures of the pelvic rami, disruption of the sacroiliac joints with impaction, and fractures of the acetabulum.
Pelvic fractures shear
Shearing injuries of the pelvis are due to extremely severe force. There is application of a shearing force to one or both of the sacroiliac joints. The force is perpendicular to the trabecular pattern of the posterior pelvic complex, which results in disruption of both the anterior and superior sacroiliac ligaments with gross disruption of the joints. With massive forces, the hemipelvis can be avulsed from the body. Anteriorly, there may be disruption of the pubic symphysis, two pubic rami, or all four pubic rami.
Pelvic fractures complex
In complex fractures, multiple forces from different angles have been exerted at the pelvis and one cannot simply classify the injuries as being due to the three aforementioned modes.
Why are pelvic fractures considered especially severe?
The pelvis is a ring structure, so disruption in one area usually means disruption elsewhere, and a very high force is required to cause fractures.
What factors influence fracture healing?
Healing depends on age (Important in children) and nutritional status. After adulthood, age plays a similar role.
Outline the early stages of fracture healing
Hemorrhage and hematoma formation
Inflammatory response (24-48 hours)
Fibroblast and macrophage infiltration
granulation tissue formation
Hemorrhage and hematoma formation (early stages of fracture healing)
Initially, there is hemorrhage at the point of fracture secondary to rupture of vessels, with production of a fusiform hematoma surrounding and joining the ends of the bone. The periosteum is torn from the outer surface of the bone; the endosteum from the marrow. Fibrin is deposited in the hematoma.
Inflammatory response (24-48 hours) (early stages of fracture healing)
This is followed in 24 to 48 hours by an inflammatory response with edema, continuing deposit of fibrin and the accumulation of large numbers of polymorphonuclear cells. As time passes, increasing numbers of machrophages appear.
Fibroblast and macrophage infiltration (early stages of fracture healing)
The next stage begins 48 hours after injury and is characterized by the appearance of fibroblast and mesenchymal cells with gradual development of granulation tissue. Necrosis of the bone adjacent to the fracture becomes evident, with empty lacunar spaces due to death of osteocytes. The line of demarcation between dead bone, with its empty lacunae, and live bone is evident. There is marked proliferation of the cells of the deep layer of the periosteum and, to a lesser degree, of the cells of the endosteum.
granulation tissue formation (early stages of fracture healing)
As the days pass, the periostial proliferation results in formation of a collar around what is becoming the callus. At the same time the periosteal cells are proliferating, capillaries begin to grow out into the hematoma. Osteoblasts begin to appear and form new trabeculae. Approximately a week after injury, granulation tissue, fibroblasts, osteoblasts, chondroblasts and small islets of cartilage in the fibrous stroma appear. Osteoblasts produce a matrix of collagen and polysaccharide, which becomes impregnated with calcium to produce immature “woven” bone. The callus reaches its maximum size in 2–3 weeks. The next stage appears in 3–4 weeks and is marked by a hard bony callus, with the bone forming from periostial and endochondrial ossification. In the last stage, there is remodeling of the new bone from a woven appearance to mature bone.
What is a callus and when does it appear?
A callus is a new bone formation bridging the fracture.
Children: visible in ~2 weeks
Adults: Consolidation ~3 months (Femur may take 4-5 months)