DMN 2 Final Review
1/399
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
400 Terms
What is the orad?
Proximal segment of the intestine (intussusceptum) that telescopes into another section
What is the aborad?
The distal segment of the intestine (intussuscipiens) that receives the telescoping segment
Most common site for intussusception in dogs and cats?
Ileocecal or ileocolic
Intussusception is associated with ______ in young animals
Enteritis
These breeds are predisposed to intussusception
German shepherds and Siamese cats
What is the main concern when mesenteric drag occurs?
Blood vessels are compressed → edema, hemorrhage, hypoxia, necrosis
Acute intussusception is what kind of obstruction?
Complete
Signs of acute intussusception:
Severe vomiting, melena/frank blood in feces, straining
Signs of chronic/partial intussusception:
Intermittent vomiting, weight loss, soft/ribbon like stool
Significance of palpating a “sausage shaped” mass
Indicates intussusception
The gold standard for diagnosing intussusception
Ultrasound of bulls-eye or target pattern
Torsion is less than a ____ degree twist whereas volvulus is a at least _____ degrees and up to _____ degrees with GDV
180
180
270
Gastric dilation volvulus is most common in what types of dogs?
Deep chested
Obstruction due to volvulus/torsion can cause:
elevated lactic acid (vascular compromise)
metabolic acidosis (anaerobic metabolism)
dehydration (fluid sequestration/reduced renal perfusion)
How does simple gastric dilation differ from GDV
Only includes distension of the stomach (no rotation) and can resolve on its own
What is a factor that makes dogs more susceptible to GDV
Middle to older age
What part of the stomach is most susceptible to decreased perfusion and eventually ischemic necrosis
Fundus
Why does tachycardia occur with GDV
Congestion of gastric/splenic vasculature causes decreased venous return (hypotension) so catecholamines are released to increase HR and therefore BP
What is the effect of reperfusion injury following surgical repositioning of stomach/spleen
Endothelial damage by ROS, DIC, and SIRs (systemic inflammatory response = widespread inflammation)
How is gastric volvulus differentiated from torsion using radiography?
Location of pylorus in volvulus is dorsal and left
What does a “reverse C” or “double bubble” of the stomach indicate on a radiograph?
GDV from pylorus moving dorsal and left
Most common type of colic is?
Spasmodic
Both _____ colic and ______ colic have increased borborygmi but differ in treatment (on farm vs in clinic)
spasmodic colic(treat on farm)
Enteritis colic (treat in clinic)
How should obstruction/impaction colic be treated?
On farm via nasogastric intubation of water or IV if severe
A horse is found rolling and looking at abdomen, is BAR, HR is 64bpm, RR WRI, increased borborygmi, no reflux, and good response to pain relief. What type of colic?
Spasmodic colic
A horse is anorexic, depressed, pawing at ground, HR of 52 bpm, tacky MM, increased borborygmi upper quadrants and lower right but decreased borborygmi lower left quadrant. Good response to pain relief with no reflux. What type of colic?
Impaction, likely at pelvic flexure
What does palpation of “doughy” intestines in left ventral quadrant of a horse indicate?
Impaction at pelvic flexure
If a horse has reflux and you suspect some type of strangulating colic, where is the issue likely occurring?
Small intestine
If a horse has no reflux but you suspect strangulating colic, where is the issue likely occurring?
Large intestine
Why is it important to give pain relief to horses with any type of colic?
Otherwise they are at risk of developing ileus (pain = more sympathetic and less parasympathetic activity = gastric stasis)
What do you do if you palpate small intestinal loops (no taeniae) in horses?
Straight to surgery (strangulating colic)
What are the 3 responses to hepatic necrosis?
Regeneration, fibrosis, biliary hyperplasia
Portals of entry into liver:
Penetrating trauma
Hematogenous spread (portal circulation)
Retrograde biliary infection (ascending)
Kupffer cells are _______ of the liver and pit cells are _____ of the liver; both are found in ______
macrophages
lymphocytes
sinusoids
Blood-borne infectious agents cause a _____ pattern of hepatocellular necrosis
random/embolic/multifocal
Hepatotoxicities and hypoxic injury cause a _____ pattern of hepatocellular necrosis
zonal
Zonal hepatocellular necrosis causes a _____ pattern that can be viewed grossly
enhanced lobular
Approx ____ of hepatic parenchyma can be removed before function is impaired and regeneration can occur within ______
75%
days to weeks
What determines if healing in the liver occurs by regeneration or by scarring?
If some hepatocytes in the lobule survive the lobule will regenerate, if the whole lobule is destroyed then scarring will occur
Stellate/Ito cells are found within ________ and produce _____, which is significant when fibrosis occurs
the space of Disse (between hepatocyte and sinusoid)
collagen/ECM
What is the significance of nodular regeneration in the liver?
Occurs with chronic/repeated injury and indicated cirrhosis/end-stage liver failure
What is the most common cause of nonspecific reactive hepatitis?
gastrointestinal disease (infiltration of portal tracts by mononuclear infiltrates)
Lymphocytic cholangitis is ________ and occurs mostly in _____
immune mediated
cats
What are the steps of neoplasia progression?
Initiation
Promotion
Progression
Presentation of a solitary well demarcated mass involving the entire hepatic lobule could be diagnosed as?
Hepatocellular carcinoma
Cholangiocellular adenomas are most common in?
cats
What is the gross presentation of a metastatic malignant melanoma on the liver?
Multifocal black masses
Hepatic lipidosis occurs from accumulation of _______
triglycerides
Low-density lipoproteins are formed from a complex of _____ with ______
triglycerides
apoproteins
The gross pathology of a liver undergoing hepatic lipidosis is:
swollen, yellow, and greasy with an enhanced lobular pattern
What animals does hepatosis dietetica occur in?
Young, rapidly growin pigs
What causes hepatosis dietetica and what is it characterized by?
Vitamin E or selenium deficiency
acute hepatic necrosis
White liver occurs due to a deficiency in _____ and is common in ____
cobalt
sheep
Why does cobalt deficiency lead to white liver disease?
Cobalt is needed to make B12 and B12 is needed to make RBCs
No cobalt = anemia = hypoxia and centrilobular hepatocellular necrosis
What is the histopathology of the liver with intrahepatic cholestasis?
Liver has diffuse yellow tracks (canaliculi have bilirubin build up)
Which protozoa cause embolic necrosis of the liver (hematogenous spread)?
toxoplasmosis and neosporosis
Intralesional tachyzoites are ______ shaped and bradyzoites are _____ shaped. Together they are indicative of a ______ infection of the liver
banana
round
protozoa
This nematode causes multifocal hepatic fibrosis and is referred to as “milk-spotted liver”
ascaris suum
Ascaris suum larvae infect the liver of which animal?
pigs
How can dirofilaria immitis effect the liver?
Block the vena cava, preventing venous return, engorging the liver with blood (congestion)
Fasciola hepatica is a liver fluke that infects:
cattle and sheep
Fasciola hepatica adults inhabit the _____ and release eggs into ____
biliary system
bile
Fasciola hepatica can allow for the proliferation of clostridium ____ and ____
haemolyticum
novyi
Clostridium haemolyticum causes _____ in ______
bacillary hemoglobinuria (intravascular hemolysis)
cattle
Clostridium novyi causes ________
infectious necrotic hepatitis
Echinococcus is a ______ that is ______ and infects the liver
cestode
zoonotic
______ is the most widespread zoonotic infection in the world
leptospirosis
Leptospirosis replicates in the ______ and is excreted in ______
liver (also kidney and spleen)
urine
Leptospirosis has toxins that cause ________ which leads to _____ necrosis in the liver and ______ icterus
intravascular hemolytic anemia
centrilobular ischemic
prehepatic
Tyzzer’s disease is caused by which bacteria?
Clostridium piliforme
Clostridium piliforme infects via the _____ route and spreads through the body via _____
oral
entero-hepatic circulation
Tyzzers disease is common in which animals?
Foals (1-6 weeks)
Clostiridium piliforme causes ______ necrosis surrounded by ______ and ______ cells in the liver
multifocal
neutrophil and mononuclear
Tyzzer’s disease causes embolic necrosis of the liver but it may also cause _____ and _____
colitis
myocarditis
Liver abscesses are ______ infections that are common in ______
polymicrobial
foals, neonate ruminants, feedlot cattle
Any type of damage to the _____ allows for translocation of bacteria into portal circulation, leading to _____ pattern of infection in liver (abcesses)
GIT
embolic
Polymicrobial infections are usually by _______ microbes and in cattle the most common type is _______
anaerobic
fusobacterium necrophorum
What are 2 predisposing factors for liver abscesses in feedlot cattle?
rumenitis and ruminal acidosis
Canine adenovirus -1 causes ________ in puppies
infectious canine hepatitis (ICH)
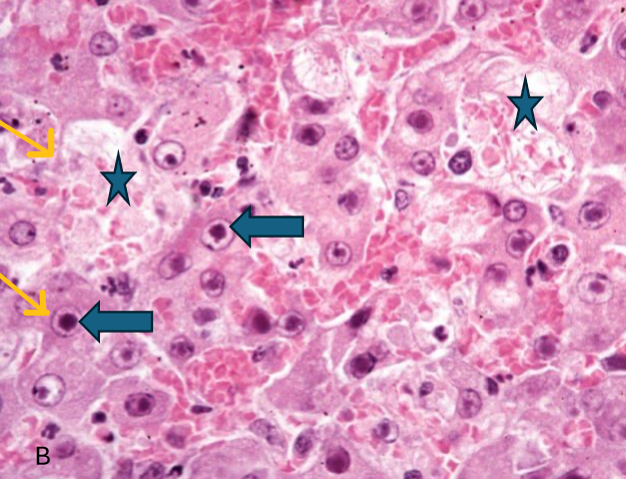
Canine adenovirus-1 can be diagnosed with visualization of ______ in hepatocytes or kupffer cells
large basophilic intranuclear viral inclusions (blue arrows)
Dogs with canine adenovirus-1 may develop ______ which is clinically referred to as ______
immune-complex uveitis
Blue eye
What is rift valley fever
vector borne zoonotic disease of ruminants that causes high mortality and hepatomegaly +embolic necrosis
These substances can accumulate inside hepatocytes
Copper, iron, glycogen, lipids
These substances can accumulate outside hepatocytes
Amyloid and bilirubin
Right-sided heart failure causes ______ in the caudal vena cava leading to ______ of the liver
elevated pressure
passive congestion
Passive congestion leads to hypoxia of ________ which results in enhanced lobular pattern (also called ______)
centrilobular zone
nutmeg liver
Congenital portosystemic shunts cause animals to be _______ and develop signs of ______ (neuro issues)
stunted
hepatic encephalopathy (hyperammonemia)
Animals with congenital PSSs will have ______ livers
small
Large breed dogs have ______ shunts
intrahepatic
Small breed dogs and cats have _____ shunts
extrahepatic
Animals with congenital PSS have abnormal ammonia metabolism leading to _____ deposition in the urinary bladder
ammonium biurate crystalluria
Congenital portal vein hypoplasia occurs in _____ and is also called ______
small breed dogs
hepatic microvascular dysplasia
Dogs with portal vein hypoplasia will have _____ and _____
microhepatica
ascites (portal vein hypertension)
Persistent portal hypertension can cause _____ and development of _______
ascites
acquired portosystemic shunts
The most common type of amyloidosis is _______ which is secondary to chronic inflammation
amyloid associated protein (AA)
Where does amyloid deposition occur in the liver?
Starts in space of Disse and extends into sinusoids
Amyloid is stained with ______
congo red
Hepatocellular copper accumulation leads to production of ______ which causes _____ necrosis
reactive oxygen species
centrilobular
Copper metabolism disorders are common in _______ due to a mutation in the _____ gene
Bedlington terriers
COMMD1
Copper is stained with
rhodanine