The Circulatory System: The Heart
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
Main function of the heart.
Provide pressure for movement of blood through blood vessels by alternatively contracting (systole) and relaxing (diastole)
Location of the heart
-Within the pericardial cavity in Mediastinum of the thoracic cavity
-directly posterior to the sternum, 2/3 lies left of midline
Coverings of heart
1. Fibrous pericardium: Outermost layer of pericardial sac
2. Serous Pericardium: Parietal layer (outer) and visceral layer (stuck to organ) that surround liquid cavity.
3. Pericardial Cavity: fluid-filled cavity between the pericardial layers
-decreases friction during heart movement
-Very Small
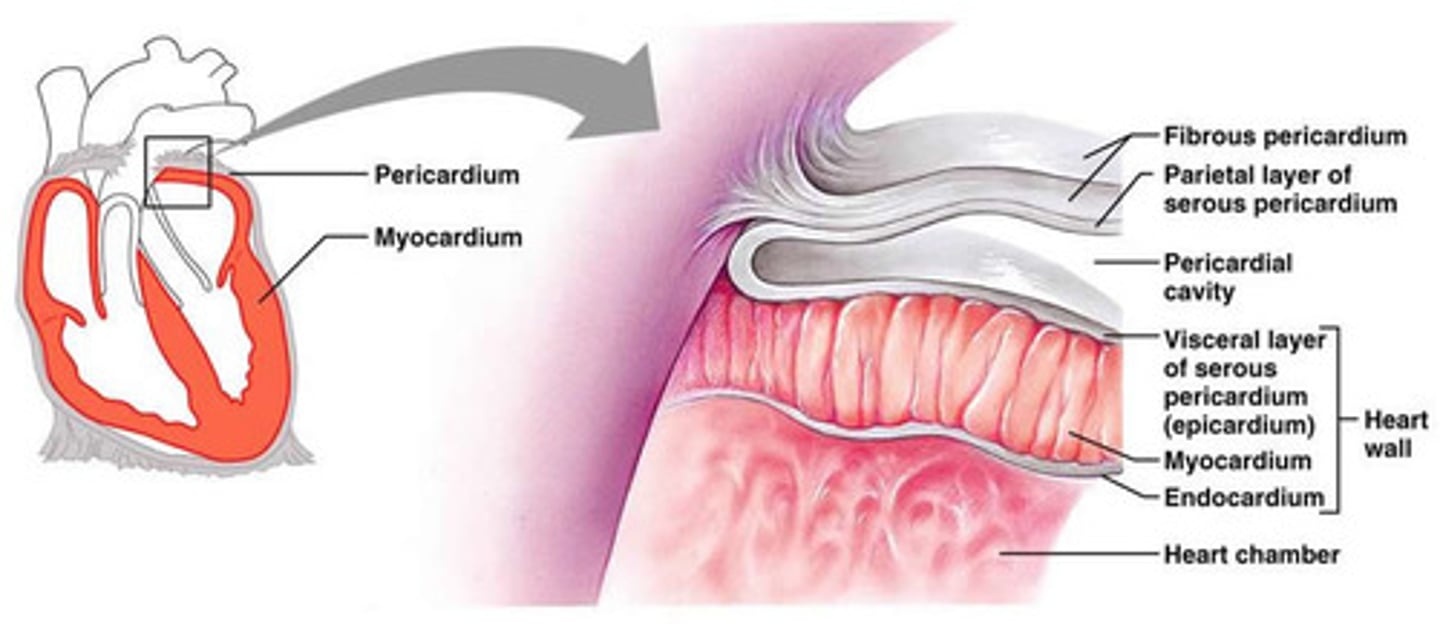
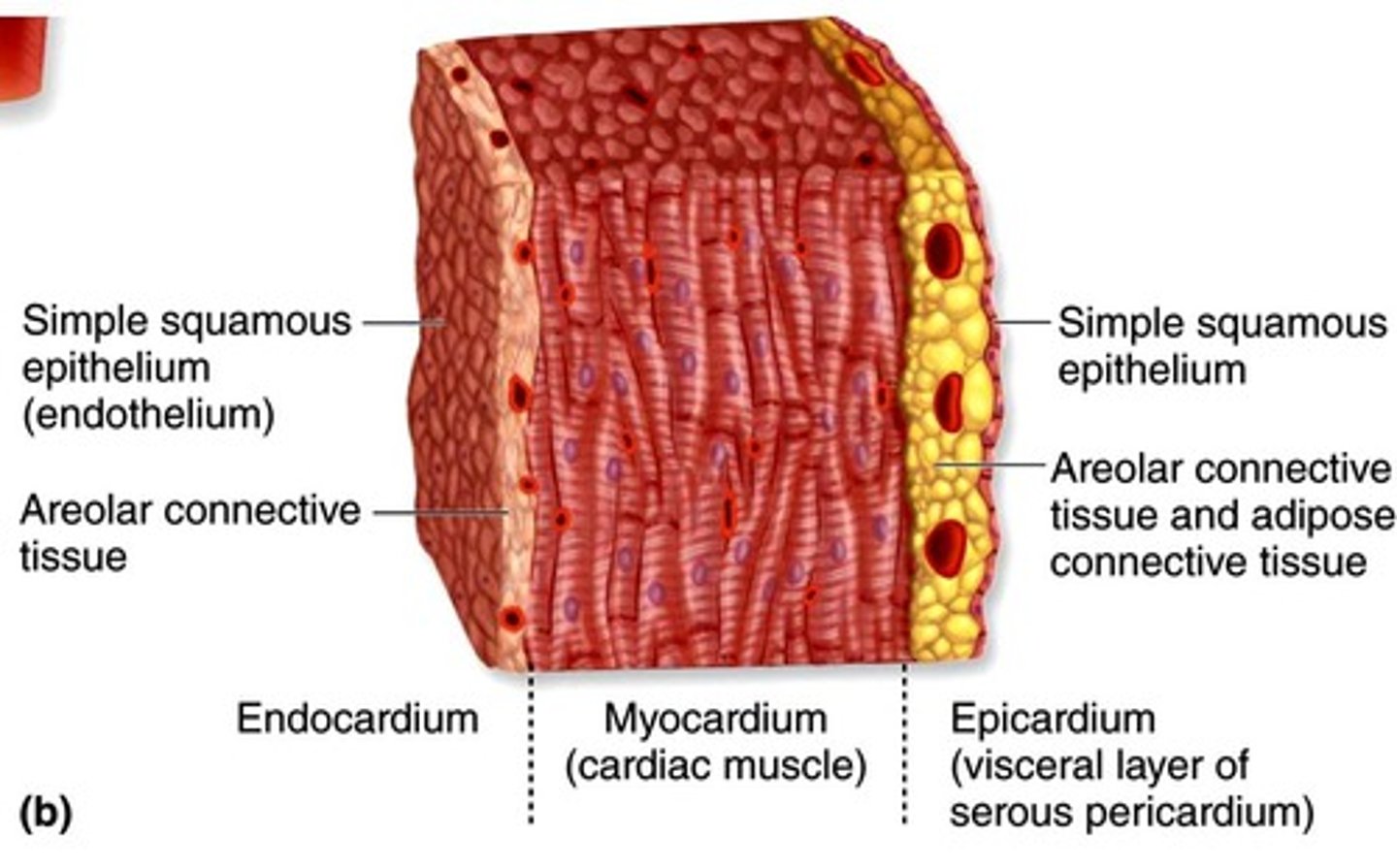
Layers of the heart wall
1. Epicardium: Visceral pericardium
-serous membrane
-most superficial layer
2. Myocardium: Middle layer of cardiac muscle
-muscles arranged in spiral or circular bundles
-fibrous skeleton supports and anchors cardiac muscle
3. Endocardium: deepest layer
-simple squamous epithelium
-one row of flat cells
Base and Apex
Base: Top of Heart
-where blood vessels are
Apex: Bottom of heart
-formed by left ventricle
Heart Chambers
1. Right Atrium
2. Right Ventricle
3. Left Atrium
4. Left Ventricle
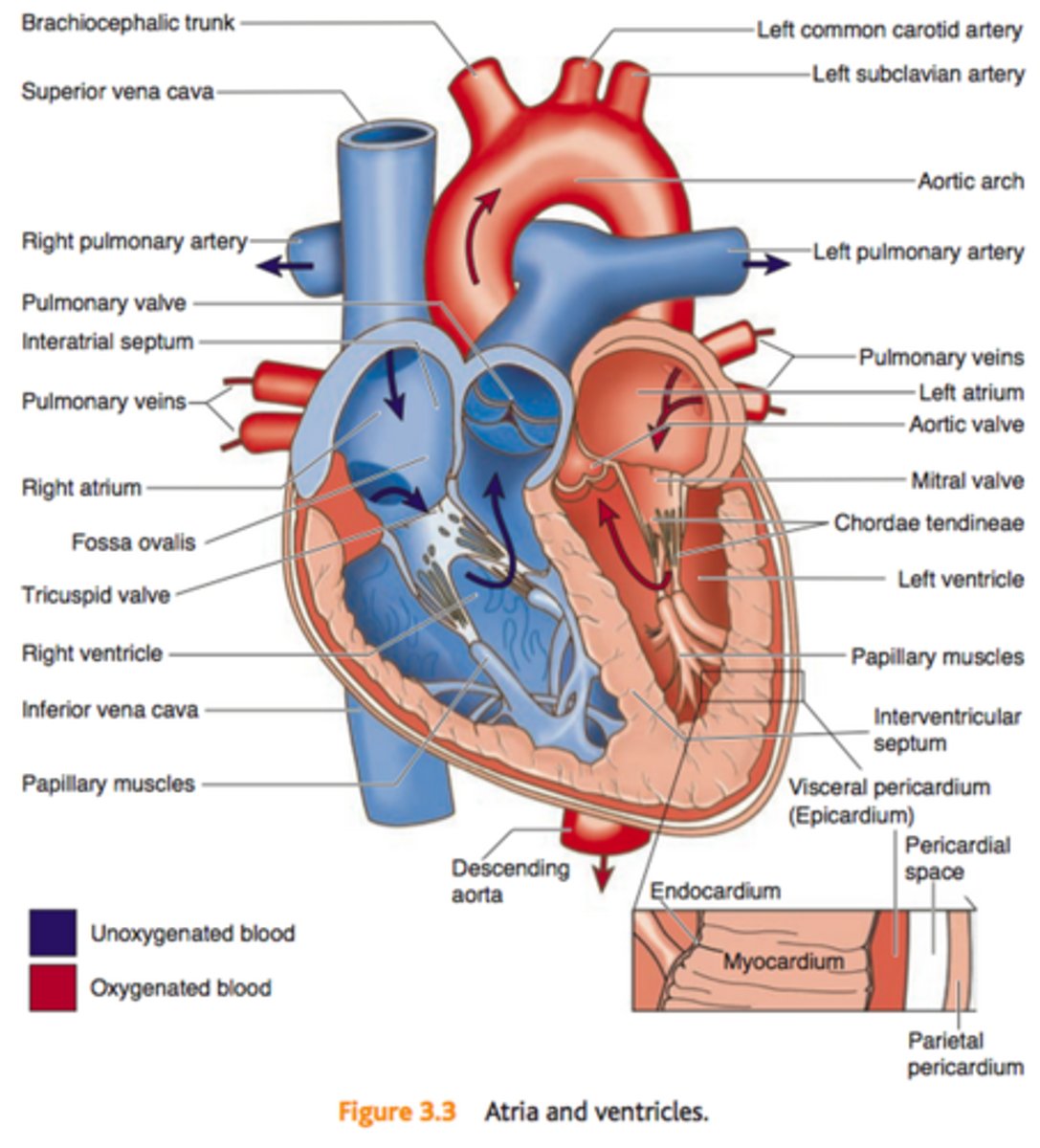
Right Atrium
-Receives blood from Vena Cava (vein)
-Pumps blood the to right ventricle -Preloads Right Ventricle
Left Atrium
-Receives blood from Pulmonary Veins
-Pumps blood to Left Ventricle
-Preloads Left Ventricle
-Passively fills with blood returning from the lungs
Right Ventricle
-Pumps blood to Pulmonary Trunk -Dysfunction of this chamber causes Systemic Edema
Left Ventricle
-Pumps Blood to Aorta
-Dysfunction of this chamber leads to Pulmonary Edema
-The strongest chamber
-Greatest contributor to systemic BP
Chamber Walls
Coronary sulcus: Atrioventricular groove
that separates the atria above from the ventricles below.
Interatrial Septum: Wall between Atria
Interventricular septum:
Cardiac Ridges
Pectinate muscles: internal ridges on the Right Atrium
Tendinae cordae: internal ridges on both Ventricles
Great Vessels of the Heart
Vessels: conduits for blood movement
-Arteries: Pulmonary Artery and Aorta, carry blood away from heart
-Veins: Pulmonary Vein, Vena Cava, and Coronary Sinus, carry blood to heart
Pulmonary Artery
caries deoxygenated blood away from heart to lungs (Pulmonary Circuit)
Aorta
carries oxygenated blood away from heart to rest of body (Systemic Circuit)
auricles
expanded areas of atria that can fill with blood from vena cava
Superior and Inferior Vena Cava
-Major Vein of Heart
-Largest vein in body
-carries deoxygenated blood from body to heart
Pulmonary Veins
carry oxygenated blood from lungs to heart
Fossa Ovalis
-remant of foramen ovale
-circle that encloses when born
-leaves only a dent
Heart Valves
Atriventricular valves: allow blood to flow from atria to ventricles when latter relaxing; prevent backflow from ventricles to atria when they contract
1.Tricuspid Valve: Right AV valve
btwn Right Atria and Ventricle
2.Bicuspid (mitral) Valve: Left AV
valve btwb Left Atria and Ventricle
Semilunar valves: allow blood to flow from ventricles to arteries when ventricles contract
3.Pulmonary Semilunar valve: Right
valve btwn Right Ventricle and
Pulmonary Artery
4.Aortic Semilunar Valve: Left Valve
btwn Left Ventricle and Aorta
papillary muscles
Responsible for pulling the atrioventricular valves closed by means of the chordae tendineae,
-small bunches of cardiac muscle.
Tendinous cords
Tighten to prevent AV from turning inside out
-prevent back flow
Flow of Blood through Valves - Pressure Gradient
1. Atrial Pressure rises above Ventricular Pressure, Atrium is in systole so AV valve opens.
2. Ventricular pressure rises above Atrial pressure, Atrium is in Diastole so papillary muscles pull and tighten tendinous cords to close AV valve, preventing backflow
3. Ventricular pressure rises above arterial pressure, Ventricles are in Systole so SL valves open
4. Ventricular pressure drops bellow arterial pressure, Ventricles are in Diastole so SL Valves close
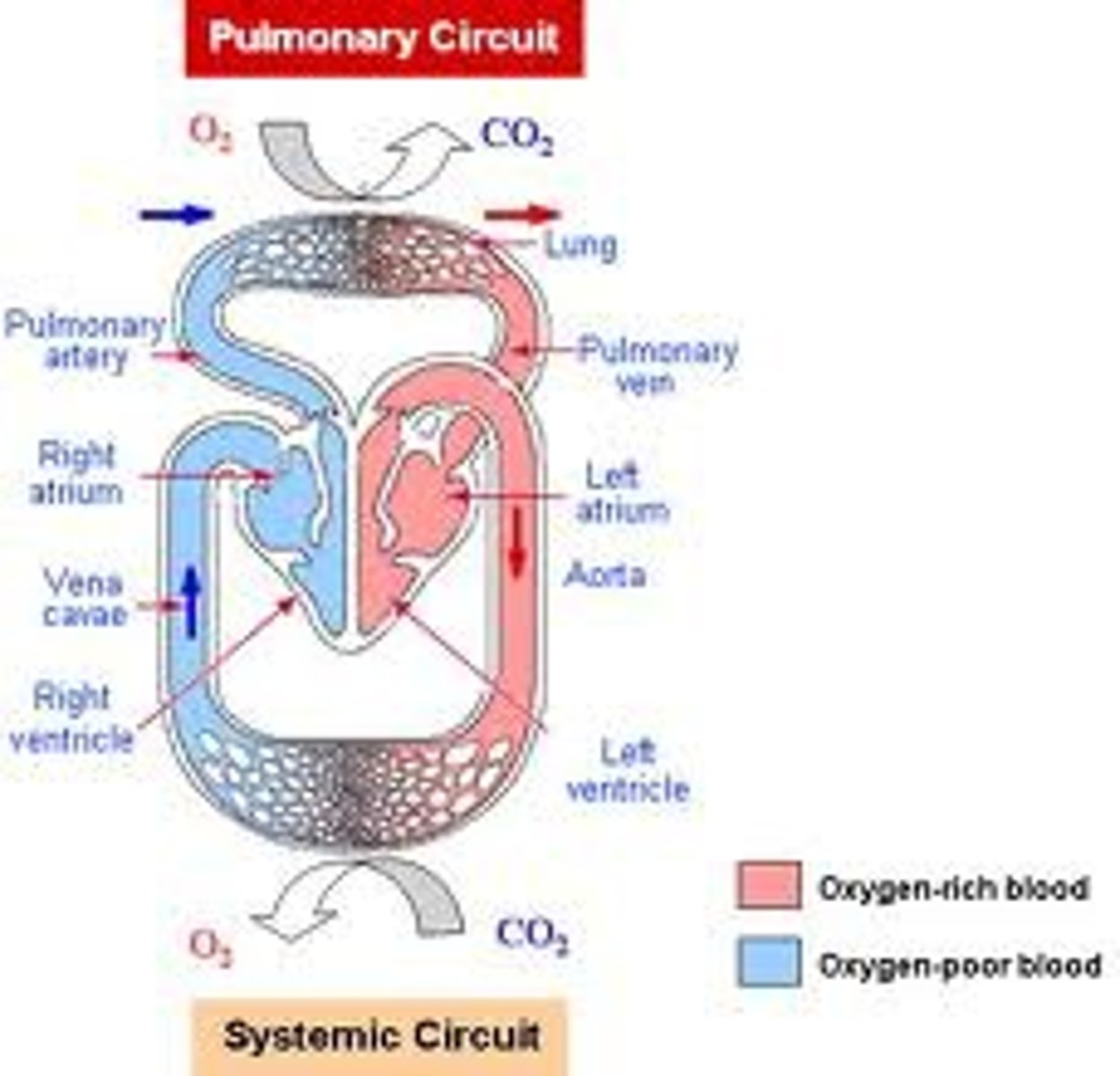
Flow of Blood in Pulmonary and Systemic Circuits
1. Superior Vena Cava
2. Right Atrium
3. Tricuspid Valve
4. Right Ventricle
Pulmonary Circuit - to and from capillary beds associated with alveoli of Lungs where gas exchange of blood takes place
5. Pulmonary valve
6. Pulmonary Trunk
7. Pulmonary Artery
8. Lungs
9. Pulmonary Vein
10. Left Atrium
11. Bicuspid (Mitral) Valve
12. Left Ventricle
Systemic Circuit- to and from capillary beds of the rest of the body - gas exchange btwn blood and tissues
13. Aortic Valve
14. Ascending Aorta
15. Coronary arteries
16. Left subclavian artery
17. Systemic capillaries
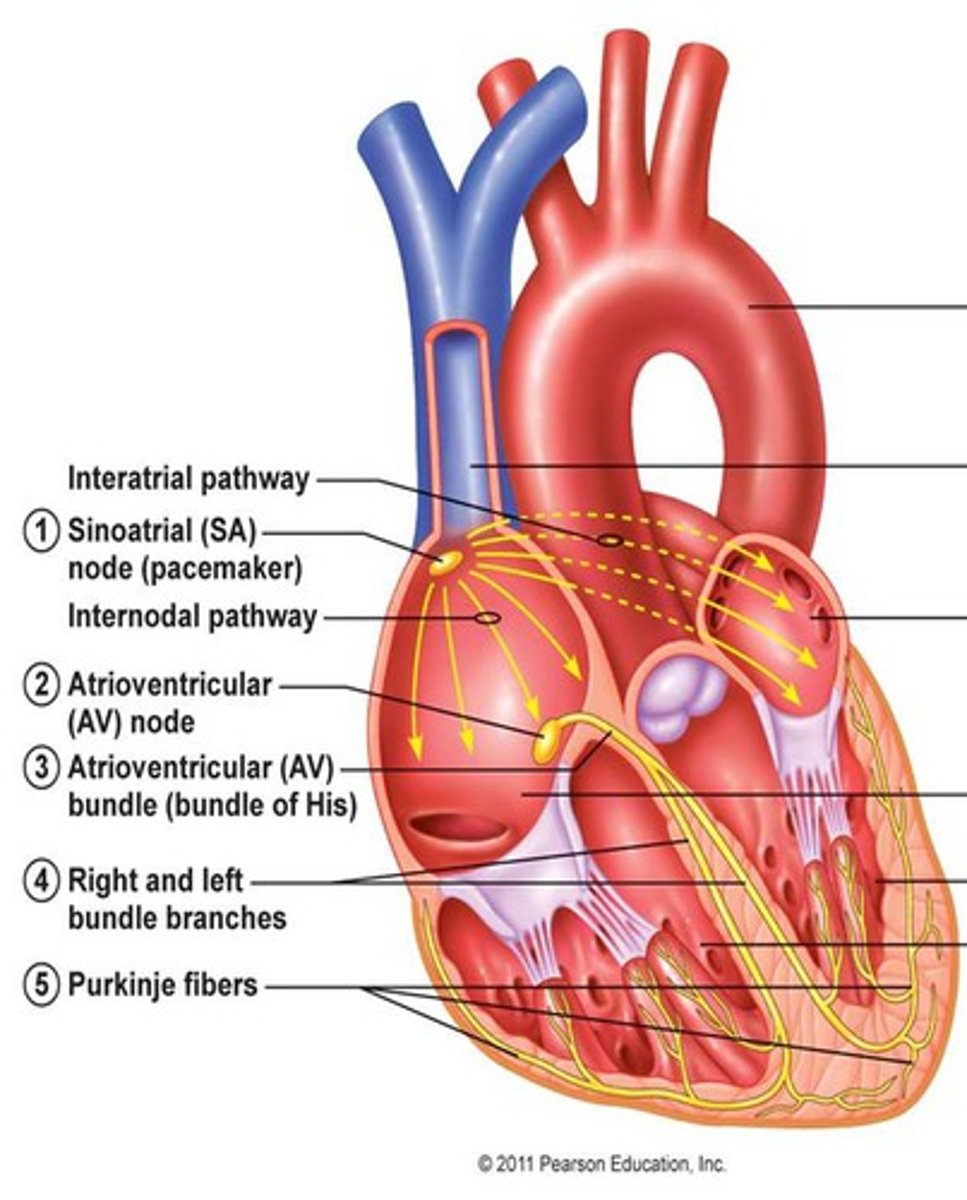
Types of Cardiac Muscle Cells (Cardiocytes)
1. Autrorhythmic :
-Spontaneously Repolarize
-SA node, AV node, AV bundle,
Purkinje Fibers
2. Contractile:
-Action Potential leads to contraction
-responsible for altering contraction
and relaxation that creates BP
-Ventricle and Atria
Cardiac muscle v. Skeletal muscle
Skeletal muscle
-applies to motor units
-only contracts in response to stimulation by neuron neurotransmitter ACh
Cardiac Muscle
-applies to entire organ
-certain cells are self-excitatory, depolarize spontaneously (Autorhythmic)
-Also autonomic stimulation (Parasympathetic and Sympathetic NS)
Purkinje Fibers
distribute(s) the electrical excitation to the cardiocytes of the ventricles.
Atrioventricular (AV) Node
-Located near the right AV valve at the lower end of the interatrial septum
-Acts as an electrical gateway to the ventricles.
Atrioventricular (AV) Bundle
-a pathway
-signals leave the AV node
-enter the interventricular septum -descend toward the apex.
Sinoatrial (SA) Node
-A patch of modified cardiocytes in the right atrium
-the pacemaker that initiates each heartbeat and determines the heart rate.
Heart's intrinsic conduction system.
1. SA node fires
2. Excitation spreads through Atrial myocardium
3. AV node fires
4. Excitation spreads down AV Bundle
5. Purkinje Fibers distribute excitation through Ventricular myocardium
Coronary circulation: Arteries
The arteries of the heart wall
-left coronary artery (LCA) divides into
-anterior interventricular branch
-circumflex branch gives off a
-left marginal branch
-Right coronary artery (RCA) divides into
-right marginal branch
-posterior interventricular branch
Coronary Circulation: Veins
The veins of the heart wall
-Great Cardiac Vein
-Posterior interventricular (middle cardiac) vein
-Left marginal vein
-Coronary Sinus
Occlusion
Common coronary circulation disorder
-clogging/blockage of an artery
-tissue downstream is deprived of nutrients
-may cause Ischemia
Ischemia
Common coronary circulation disorder
-inadequate blood supply to organ or part of body
-leads to changes in cell structure or function
-can be caused by Occlusion and may cause Infarction
Infarction
Common coronary circulation disorder
-Area of dead tissue (necrotic)
-leads to disruption of arterial circulation
-can be caused by Ischemia
The Nervous System and Heart Beat.
Explain the relationship between
Preload
The precontraction pressure in the heart as the volume of blood builds up.
-Volume Ventricles must eject
afterload
resistance ventricles contract against
Diastole
Relaxation of Heart (Repolarization)
Systole
Contraction of Heart (Depolarization)
Depolarization
Chamber is about to contract (Systole)
-related to P-wave and QRS complex
Repolarization
Chamber goes back to relaxation (Diastole)
-Related to T-wave
The principal deflections that are observed in a normal ECG
and explain what is happening in the heart during each of these events
"electrocardiogram" (ECG).
-pattern of electrical activity recorded at the body surface
-Composed of P- and T-wave and QRS complex
QRS Complex
Ventrical Depolarization (Ventricles go into systome- they are about to contract)
T-wave
ventricle repolarization
P-wave
Atrial Depolarization (atria go into systole- they are about to contract)
cardiac cycle
and be able to discuss sequential and concurrent changes in blood pressure (atria, ventricles, aorta), blood volume (ventricles), heart sounds, the ECG and mechanical events. You should study and be able to reproduce Figure 19.20.
Ventricular Filling
Isovolumetric Contraction
Ventricular Ejection
Isovolumetric Relaxation
"cardiac output".
CO = HR X SV.
you can see that there are only two ways to change it: change the heart rate or change the stroke volume.
Stroke Volume
The amount of blood ejected from the heart in one contraction.
SV = EDV - ESV.
Factors that influence stroke volume.
Heart Rate
Factors that influence heart rate.
Factors ) that influence Contractility.
How the brain regulates cardiac output.
How cardiac output can vary within and between individuals.
congestive heart failure.
The difference between left and right heart failure.
Explain how you can tell
Place the labels in order denoting the sequence of events of the cardiac cycle beginning with passive ventricular filling.
1. The entire heart exhibits resting
membrane potential
2. Cells of the SA node reach autorhythmic threshold
3. Voltage-regulated, fast-calcium and and sodium channels open in the SA node
4. Cations flow from the SA node to the adjacent cardiocytes through gap junctions
5. The P-wave appears on an EKG
6. AV node depolarization occurs and transmits the signal to the bundle branches
7. The downward deflection (Q) is seen on the EKG tracing
8. End diastolic volume is achieved
9. The AV valves close
10. The semilunar valves open
11. Blood exits the ventricles
12. Voltage-regulated potassium channels open in the myocytes of the ventricles
13. The T-wave appears on the EKG tracing
14. End systolic volume is achieved as the heart enters relaxation