module 2
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
cleaning agent
An agent, usually containing a surfactant, used for the removal of substances (e.g., dirt, debris, microbes, and residual drugs or chemicals) from surfaces.
aseptic
free from contamination with harmful micro-organisms
technique
the methods or procedures used to manipulate products
aseptic technique
a set of methods used to keep objects and areas free of microorganisms and thereby minimize infection
usp
describes the minimum standards
facillities
develops SOPs (standard operation procedure)
disinfectant
a chemical or physical agent used on inanimate surfaces an objects to destroy fungi, viruses and bacteria
sporicidal agents
a chemical or physical agent that destroys bacterial and fungal spores when used at a sufficient concentration for a specified contact time. It is expected to kill al vegetative microorganisms
why is entry-angle of the needle into the vial stopper important (what are we trying to prevent?)
trying to prevent “coring”
or creating a hole in the vial that will later lead into leakage from the vials
when is a visual inspection of a compounded CSP performed
after compounding
the day when it will be sent out before releasing and dispensing it to the patient
swfit
in lab what is our cleaning agent
sterile 70% IPA
in lab what is our disinfecting agent
daily
when to clean and disinfect pass through chamber, work surfaces, and floors in classified areas
monthly (CSP1/CSP2), weekly (CSP 3)
when to use sporicidal agents on pass through chamber, work surfaces and flors in classified areas
monthly
when to clean/disinfect/apply sporicidal to walls/doors/door frames, ceilings, storage shelving and equipment outside PEC
not in compounding area
should not be completed during the same time someone is garbing
where should doffing occur per USP 797 guidelines
dirty side of ante room
where should doffing occur per ACPHS guidelines
gloves, gown, haircover, mask, shoe covers, wash hands
order of doffing per ACPHS guidelines
inspect
hold up to light, look through unlabeled side, rotate bag slowly at least once
compounding record
documents the compounding process
all category 1/2/3 and immediate use CSPs for 1+ patient
per USP 797 when is a compounding record required
after compounding
when does the compounder sign the compounding record
particles, leaks, cracks, label doesnt match, discoloration, improper seal
examples of when a CSP would not pass a final check (5)
first air
air that flows into hood via HEPA filter
injection port, vial stopper, ampule necks
critical sites to be wiped down with 70% IPA when making a single additive CSP (3)
bevel up
what direction should needle bevel be facing when entering rubber stopper of vial
different filters in the hood
HEPA filter
Pre-filter (on top of the hood always the air in the room to go through the hood and get cleaned and come out the HEPA filter)
prevent leaks
why is entry angle of needle into vial stopper important
aseptic technique
set of methods used to keep objects and areas free of microorganisms and thereby minimize infection
tacky mats
remove debris from the bottom of your shoes, located outside the ante room door
must, should
cleaning agents used in the PEC ____ be sterile, outside the PEC agents ____ be sterile
before compounding, after compounding
when to use IPA on the horizontal work surface in PEC
wipe with 70% IPA
what should be done to items before they are introduced to the PEC
should
conventionally manufactured sterile products ____ be used when available
1+ nonsterile comp, non sterile supplies/devices
when is sterilization required (2)
terminal, steam filter with 0.22 micron
methods of sterilization (3)
order of use
how should items be placed in the DCA
DCA
critical area within the ISO class 5 PEC where critical sites are exposed to unidirectional HEPA= filtered air, also known as first air
2-3 in, 6 in, 6in
DCA is ___ from the back screen ___ from each side and ____ inside the front of hood
zone of turbulence
the area behind any item (e.g., vial, IV bag, syringe) on the hood where sterile airflow from the HEPA filter is interrupted
spray with IPA
correction if hands are taken out of the DCA
12 hours
28 days
After a single-dose vial is punctured in a PEC, how long can it be used if it is stored appropriately?
After a multiple-dose vial is punctured in a PEC, how long can it be used if it is stored appropriately?
mL/hour
Which of the following units will you most commonly use in the Rate of Administration field of the Patient SpecificLabel
8
You are adding 8 mL of diluent to a drug vial for reconstitution. How many milliliters of air should you remove fromthe drug vial?
false
True or False: After preparing a CSP, you will label the CSP in the PEC.
environment, aseptic processing, starting components, sterility testing, storage
5 factors that affect sterility
Category 1 CSP
must be prepared in an ISO class 5 or better PEC
PEC may be located in an unclassified SCA or within cleanroom suite
Category 2 CSP
must be prepared in an ISO class 5 or better PEC, PEC must be located within clean room suite
category 3 CSP
must be prepared in an ISO class 5 or better PEC
PEC must be located within cleanroom suite
enhanced personnel competency
additional garbing
increased environmental monitoring
increased frequency of sporadical
sterility testing
bacterial endotoxin (one or more nonsterile components)
immediate use CSP
direct and immediate administration to a patient
Aseptic processes
physical and chemical compatibility
no more than 3 different sterile products
single dose containers discarded after use
admin begins 4 hours following start of prep
<12 hours
BUD for a category 1 CSP at room temperature
<24 hours
BUD for a category 1 CSP that is refrigerated
1 day
BUD for a category 2 CSP that was aseptically processed had no sterility testing performed, not prepared from only sterile starting components at CRT
4 days
BUD for a category 2 CSP that was aseptically processed had no sterility testing performed, not prepared from only sterile starting components that is refrigerated
45 days
BUD for a category 2 CSP that was aseptically processed, had no sterility testing performed, not prepared from only sterile starting components that is stored in the freezer
4 days
BUD for a category 2 CSP that was aseptically processed, had no sterility testing performed, was prepared from only sterile starting components that is stored at CRT
10 days
BUD for a category 2 CSP that was aseptically processed, had no sterility testing performed, was prepared from only sterile starting components that is stored in the refrigerator
45 days
BUD for a category 2 CSP that was aseptically processed, had no sterility testing performed, was prepared from only sterile starting components that is store in the freezer
30 days
BUD for a category 2 CSP that was aseptically processed and had sterility testing performed and passed, that is stored at CRT
45 days
BUD for a category 2 CSP that was aseptically processed and had sterility testing performed and passed, that is stored in the refrigerator
60 days
BUD for a category 2 CSP that was aseptically processed and had sterility testing performed and passed, that is stored in the freezer
14 days
BUD for a category 2 CSP that was terminally sterilized and had no sterility testing performed, that is stored at CRT
28 days
BUD for a category 2 CSP that was terminally sterilized and had no sterility testing performed, that is stored in the refrigerator
45 days
BUD for a category 2 CSP that was terminally sterilized and had no sterility testing performed, that is stored in the freezer
45 days
BUD for a category 2 CSP that was terminally sterilized and had sterility testing performed and passed, that is stored at CRT
60 days
BUD for a category 2 CSP that was terminally sterilized and had sterility testing performed and passed, that is stored in the refrigerator
90 days
BUD for a category 2 CSP that was terminally sterilized and had sterility testing performed and passed, that is stored in the freezer
60 days
BUD for a category 3 CSP that was aseptically processed, sterility tested, and passing all applicable test stored at CRT
90 days
BUD for a category 3 CSP that was aseptically processed, sterility tested, and passing all applicable test stored in the refrigerator
120 days
BUD for a category 3 CSP that was aseptically processed, sterility tested, and passing all applicable test stored in the freezer
90 days
BUD for a category 3 CSP that was terminally sterilized, sterility tested, and passing all applicable test stored at CRT
120 days
BUD for a category 3 CSP that was terminally sterilized, sterility tested, and passing all applicable test stored in the refrigerator
180 days
BUD for a category 3 CSP that was terminally sterilized, sterility tested, and passing all applicable test stored in the freezer
chemical/physical properties of drug, material of container, compatibility of container with CSP
factors that affect stability (3)
USP 797, expiration dates, manufacturer
3 factors to consider when determining BUD (more stringent applies)
regular needle
when filtering is required and a filter needle is used which needle is used first?
will change from regular needle to filter needle after fluid is drawn up and before priming
when filtering is required and a filter needle is used when is needle change made?
upright position
in what position is the filter needle/syringe held during priming
filter straw
when filtering is required and a filter straw is used which is used first?
use straw first to put liquid in syringe, then change to regular needle
when filtering is required and a filter straw is used when is the change of straw to needle made?
prime with the filter needle
with the filter needle procedure, will you prime to regular or filter needle?
no
do you need to prime a filter straw?
2
how many needles are required when using a filter disc
upright
what position is the filter disc held in during priming?
5 micron
what is the filter size for a filter needle
5 micron
what is the filter size for a filter straw
0.2 micron
what is the filter size for a filter disc
filter needle/straw
what filtering devices are appropriate to filter glass or paint from an ampule?
disc
what filtering devices are appropriate sterilize a product
docking
connecting the proprietary bag to the vial
activation
breaking the seal between the proprietary bag and vial so that fluid mixes with drug powder for reconstitution for drug to be given
ADD-vantage
proprietary bag system requiring a specific drug vial to twist in
Minibag plus
proprietary bag system that can use any vial and snaps on (better then ADD-vantage)
multiple dose container
a drug container that is penetrated multiple times and usually contains a preservative to inhibit growth of microorganisms and minimize risk of contamination
28 days
BUD for multi dose vials per USP 797
master formulation
required for all CSPs prepared from:
non-sterile ingredients
or
CSPs prepared for more than one patient
always, dont always
you ____ need a CR (compounding record) , you __ ____ need a MR (master formulation)
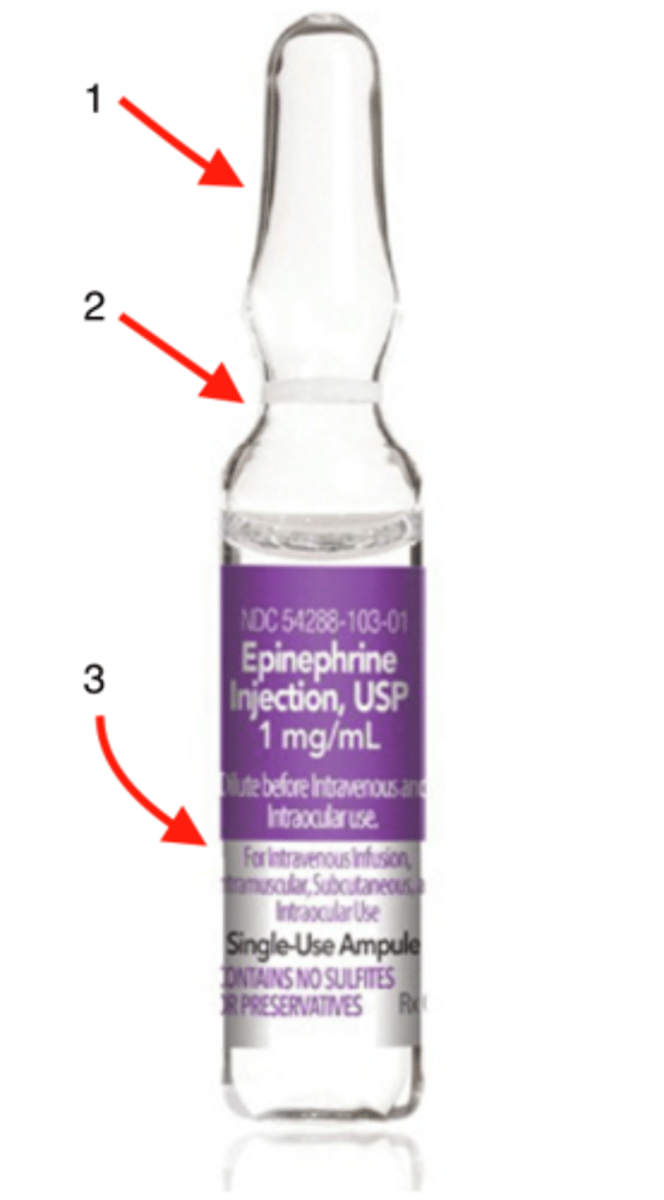
head
1
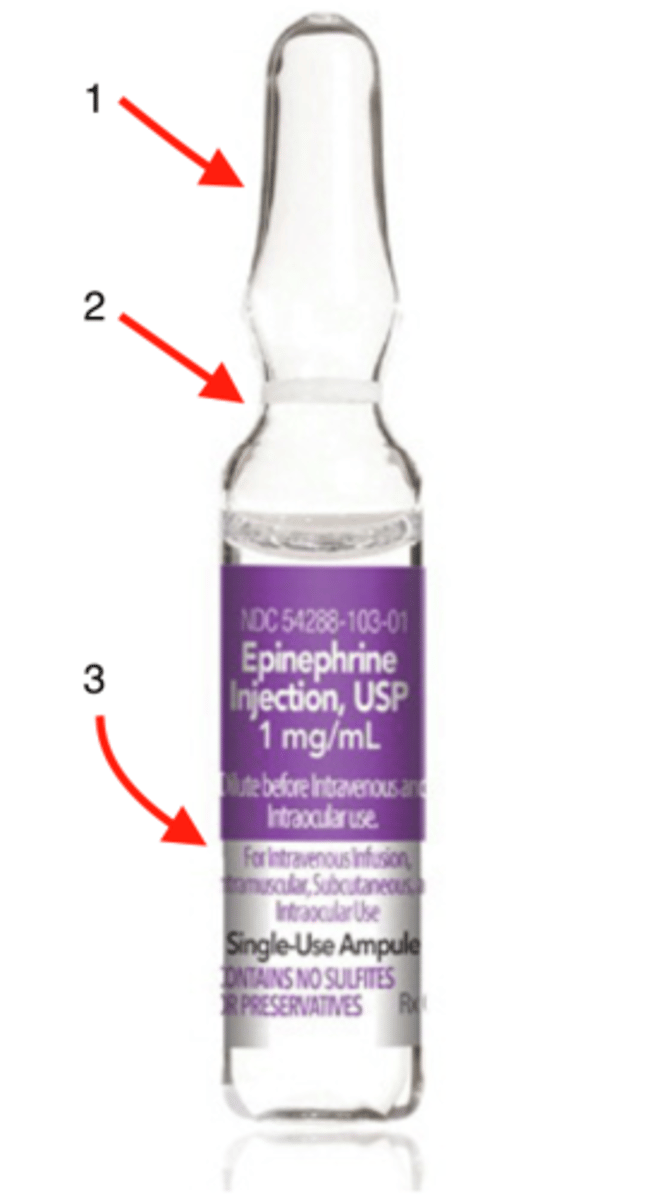
neck
2
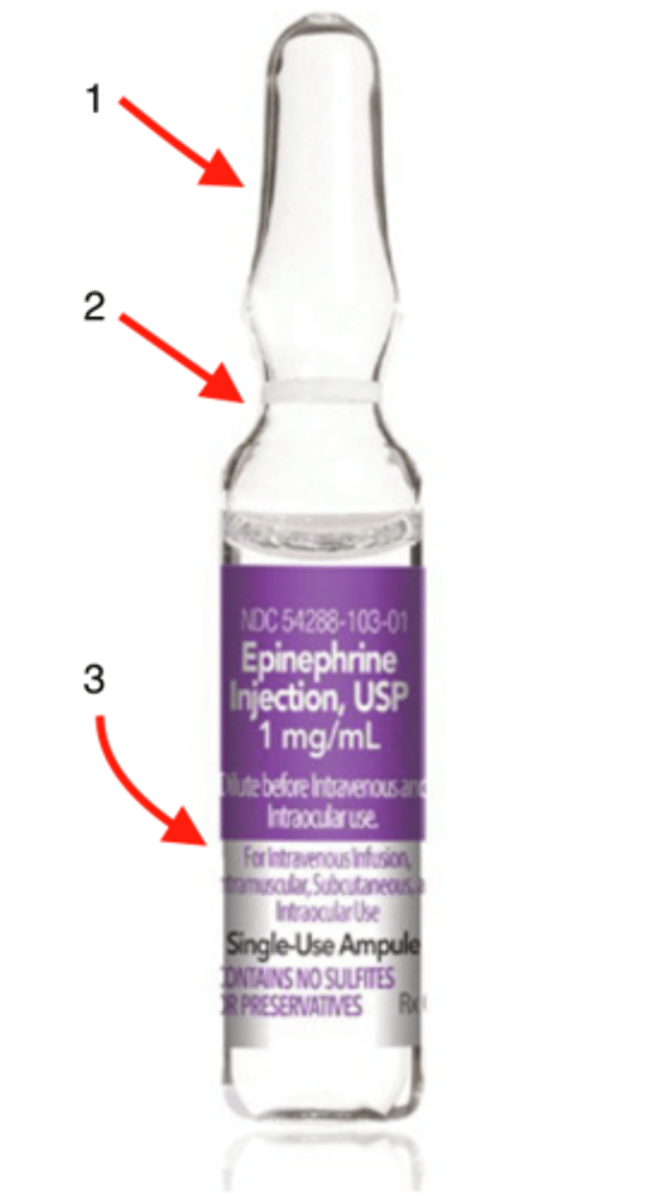
body
3