3.2- Transport in Animals (copy)
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
the need for transport systems in multicellular animals
larger organisms require mass transport systems due to:
large transport distances between exchange sites→ diffusion not fast enough to meet metabolic requirements of cells
SA:V ratio decreases as size of organism increases→ less SA for absorption and excretion, greater volume= longer diffusion distance
high metabolic rate→ higher demand for oxygen and nutrients, more waste produced
what is mass flow
the bulk movement of materials between exchange sites
what is the purpose of mass transport systems
move substances quickly between exchange site to another
maintain diffusion gradient at exchange sites and between cells and extracellular fluid
ensure effective cell activity by keeping immediate fluid environment within suitable metabolic range
single circulatory system
blood passes through heart once during one complete circuit of the body
single circulatory system in fish
deoxygenated blood pumped from heart to gills
oxygen and carbon dioxide exchanged at gills
oxygenated blood flows from gills to rest of body→ travels through capillaries in organs delivering oxygen and nutrients
blood returns to heart→ 1 atrium, 1 ventricle
double circulatory system
blood passes through heart twice during one complete circuit of the body
double circulatory system in mammals
heart has left and right side separated by septum:
left side→ oxygenated blood
right side→ deoxygenated blood
blood in right side leaves and travels to lungs
returns to left side and is pumped around the rest of the body
once body has passed through organs, it returns to right side of the heart again
advantages of double circulation
higher blood pressure and avg speed of flow→ blood only passes through one capillary network before returning to the heart
increased pressure and speed= steeper concentration gradient
open circulatory system
blood not contained in blood vessels→ pumped directly into body cavities
arthropods and molluscs have open circulatory systems
closed circulatory system
blood pumped around body and is always contained in a network of blood vessel
all vertebrates and invertebrates have closed circulatory systems
path of blood around the body
heart → arteries → arterioles → capillaries → venules → veins
insect circulatory systems
have one main blood vessel→ dorsal vessel
tubular heart in abdomen pumps haemolymph (insect blood) into dorsal vessel
haemolymph delivered into haemocoel (body cavity)→ surrounds organs and re-enters the heart via ostia (one way valves)
oxygen not transported in haemolymph→ tracheal system
arteries
transport blood away from heart
veins
transport blood to the heart
arterioles
narrower blood vessels that transport blood from arteries to capillaries
venules
narrower blood vessels that transport blood from capillaries to veins
structure of arteries
consist of three layers:
tunica externa, tunica media, tunica intima
tunica externa→ made of collagen to provide rigidity and overprotection
tunica media→ layer of muscle cells strengthening arteries so they can withstand high pressure. elastic tissue maintains blood pressure
tunica intima→ endothelial layer- one cell thick
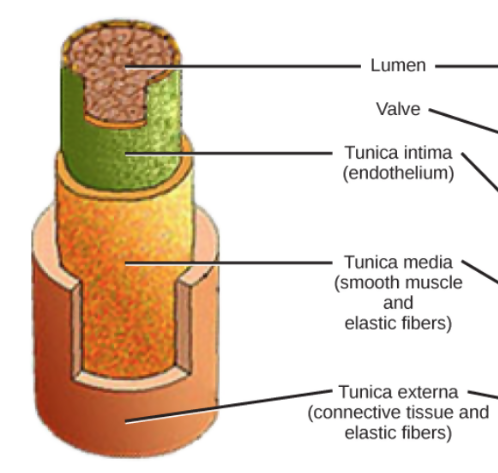
structure of arterioles
have muscular layer→ can contract to partially cut off blood flow to specific organs
lower proportion of elastic fibres and large number of muscle cells
structure of veins
thinner tunica media due to lower blood pressure
larger lumen than in artery→ ensures blood returns to heart at adequate speed
have valves→ prevent backflow
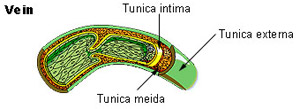
structure of venules
connect capillaries to veins
few/ no elastic fibres and a large lumen
no need for muscular layer→ blood is at low pressure
structure of capillaries
very small lumen→ blood travels slower so more diffusion can occur
large number of capillaries→ short diffusion distance
wall of capillary is one cell thick→ reduced diffusion distance
cells of walls have gaps→ allow blood plasma to leak out and form tissue fluid
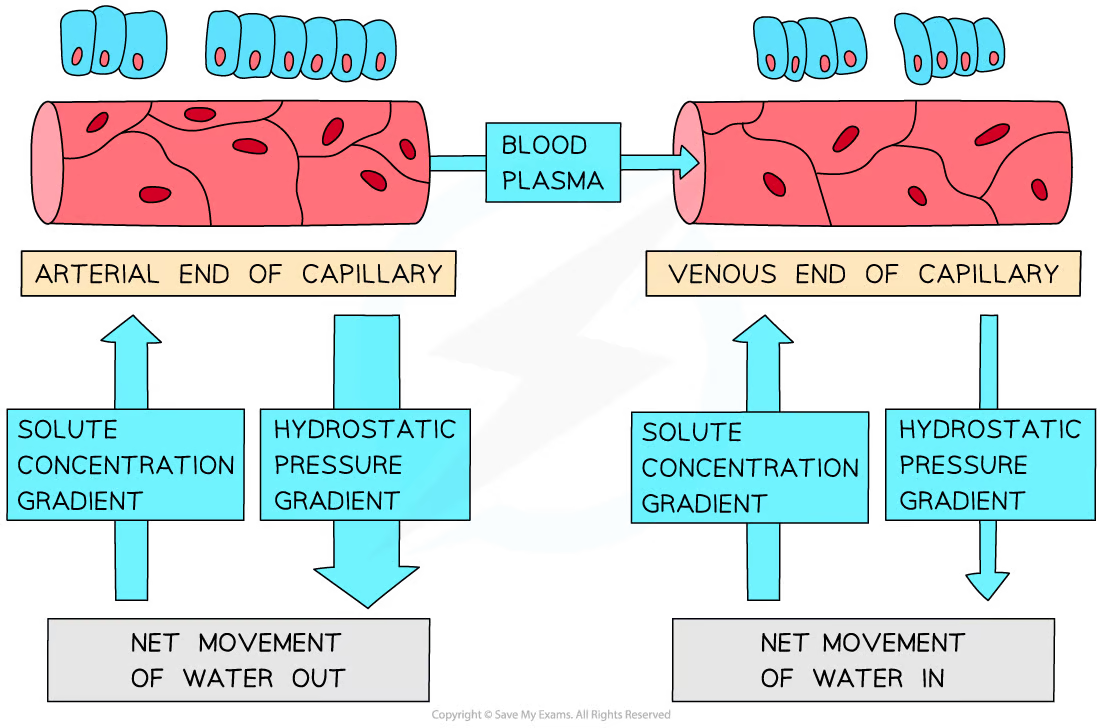
what is tissue fluid
a liquid that has substances dissolved in it→ similar to plasma but with fewer proteins
exchange of substances between cells and blood occurs via tissue fluid→ surrounds all cells of the body not in circulatory system
hydrostatic pressure
pressure exerted by a fluid e.g. blood
e.g. blood pressure
oncotic pressure
osmotic pressure exerted by plasma proteins within a blood vessel
lower WP within blood vessel→ water moves into vessel by osmosis
tissue fluid formation
at arterial end of capillary:
hydrostatic pressure forces fluid out of capillary
proteins remain in blood→ too large
WP gradient created due to increased protein content
hydrostatic pressure>oncotic pressure→ water moves out of capillaries into tissue fluid
at venous end:
hydrostatic pressure reduced due to greater distance from heart
WP gradient stays same as at arterial end
osmotic pressure>HS pressure→ water flows back into capillary from tissue fluid
formation of lymph
not all tissue fluid re-enters capillaries→ enters lymph vessels
vessels separate to circulatory system
larger molecules that can’t pass through capillary wall enter lymphatic system as lymph
liquid moves along larger vessels in system by compression caused by body movement→ backflow prevented by valves
lymph re-enters bloodstream through veins located close to the heart→ plasma proteins are returned to blood via lymph capillaries to maintain WP gradient
lipids transported from intestines to bloodstream by lymph system
structure of the heart
divided into 4 chambers
left and right sides of the heart separated by septum
atria and ventricles separated by valves
When are valves open/ closed?
What valves are found in the heart
open when BP behind is greater than BP in front of them
closed when BP in front of them is greater than BP behind them
RA and RV separated by tricuspid valve
RV and PA separated pulmonary valve
LA and LV separated by bicuspid valve
LV and aorta separated by aortic valve
blood vessels going into and coming from heart
Pulmonary artery:
heart→ lungs
from right ventricle
Pulmonary vein:
lungs→ heart
into left atrium
Vena Cava:
body→ heart
to right atrium
Aorta:
heart→ body
from left ventricle
coronary arteries
Arteries that provide blood to the heart for its own aerobic respiration for muscle contraction
stages of the cardiac cycle
atrial systole
ventricular systole
diastole
atrial systole
atrial walls contract:
volume in atrium decreases, pressure increases
atrial pressure rises→ AV valves open
blood forced into ventricles
ventricular systole
walls of ventricles contract:
volume decreases, pressure increases
pressure in ventricles rises above atrial pressure:
AV valves forced close
pressure in ventricles rises above that in aorta and PA:
semilunar valves forces open→ blood forced into arteries
diastole
atria and ventricles both relaxed
pressure in ventricles drop below that in arteries→ SL valves forced close
atria continue to fill with blood
pressure in atria rises above that in ventricles→ AV valves forced open
blood passively flows into ventricles
cycle begins again
cardiac output
the volume of blood pumped by the heart per unit time
factors affecting cardiac output
fitness→ fitter=higher cardiac output due to thicker ventricular muscles in the heart
exercise→ cardiac output increases during exercise
heart rate
number of times a heart beats per minute
stroke volume
volume of blood pumped out of left ventricle in one cardiac cycle
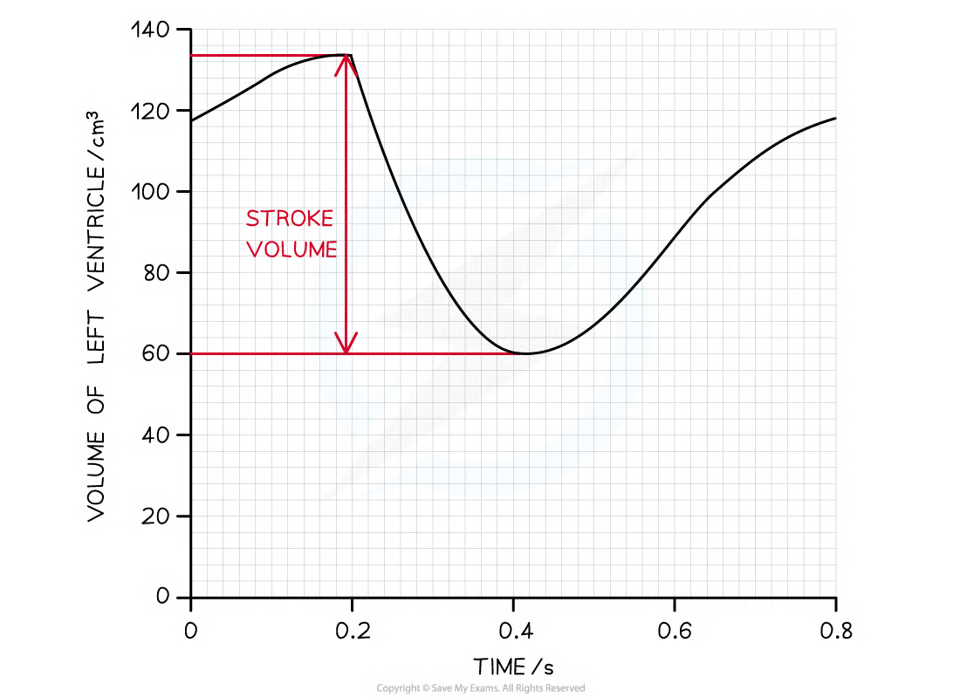
calculating cardiac output
cardiac output= heart rate*stroke volume
myogenic
heart beats without external stimulus
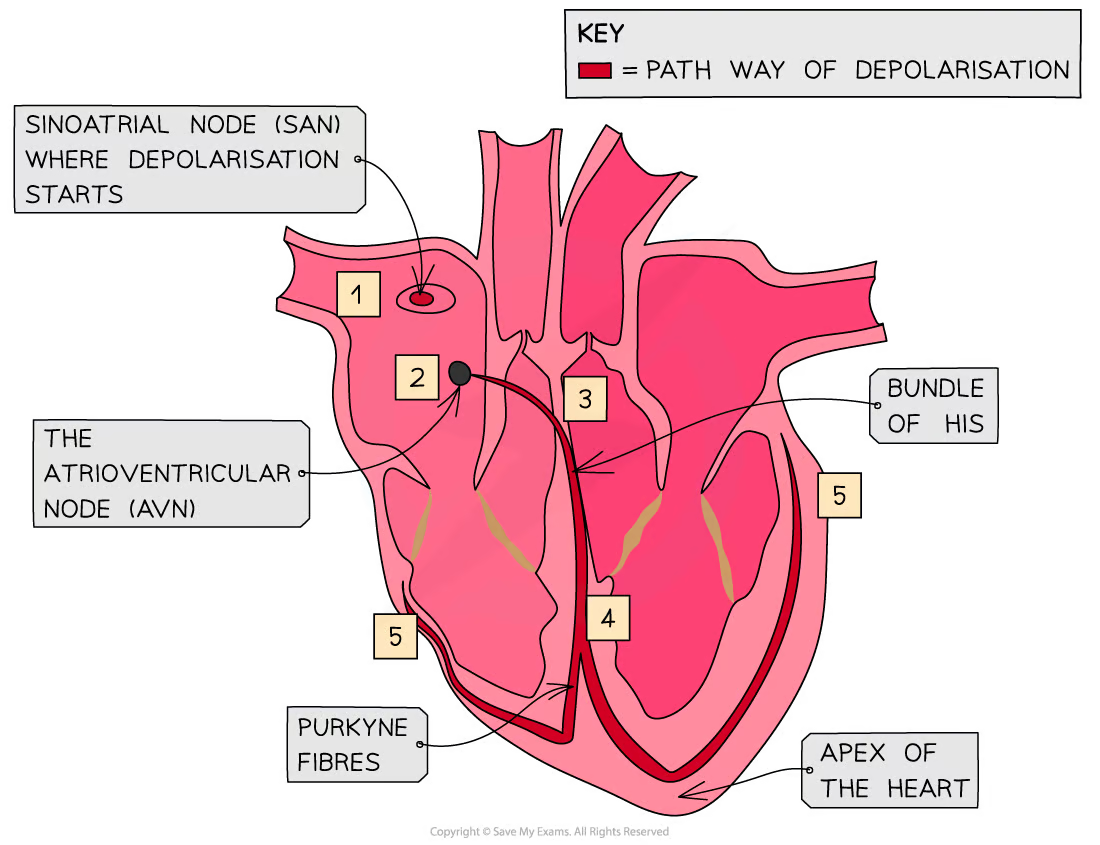
sinoatrial node
group of cells in right atrial wall
initiates wave of depolarisation→ causes atrial contraction
myogenic contraction
SAN creates wave of depolarisation→ causes atrial contraction
Annulus Fibrosus→ non-conducting so prevents depolarisation spreading straight to ventricles
depolarisation carried to atrioventricular node (AVN)→ conducting tissue between atria and ventricles
After delay, AVN is stimulated→ stimulation passed along bundle of His (in septum):
delay= ventricles contract after atria
bundle of His divides into two conducting fibres→ Purkyne tissue- carries wave of excitation along them
Purkyne fibres spread around ventricles and initiate depolarisation of ventricles from bottom of heart→ causes ventricular contraction
ECG
electrocardiogram
electrodes that detect electrical signals are placed on skin→ produce electrocardiogram
shows distinctive electrical waves produced by activity of heart
used to detect heart problems
reading ECG traces
P wave:
depolarisation of atria, resulting in atrial systole
QRS complex:
depolarisation of ventricles, resulting in ventricular systole
largest→ ventricles have largest muscle mass
T wave:
repolarisation of ventricles→ ventricular diastole
U wave:
uncertainty→ repolarisation of Purkyne fibres?

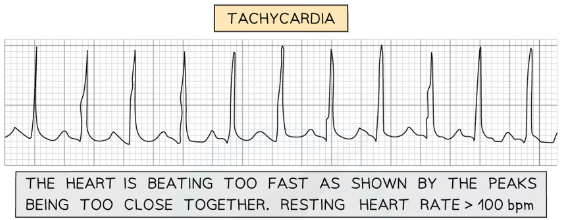
tachycardia
heart beat too fast
peaks of ECG too close together
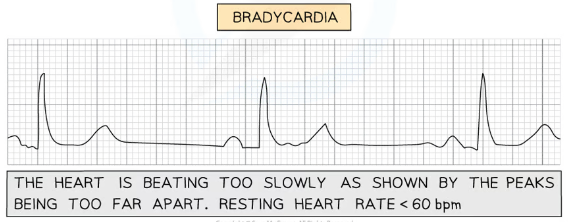
bradycardia
heart beat too slow
peaks of ECG too far apart
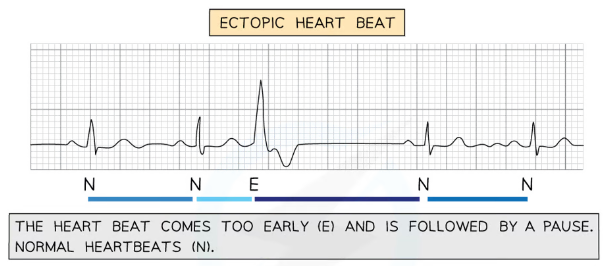
ectopic heartbeat
early heartbeat followed by a pause
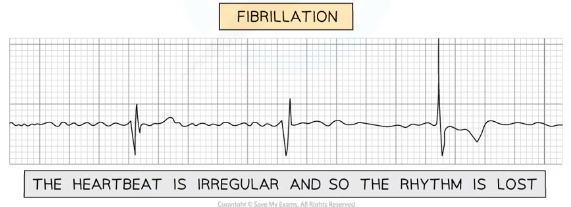
fibrillation
irregular heartbeat→ rhythm is lost
role of haemoglobin
allows for transport of oxygen around body
each haemoglobin molecule contains 4 haem groups- each able to bond to one O2 molecule
equation of fomation of oxyhaemoglobin
Oxygen + Haemoglobin ⇌ Oxyhaemoglobin
4O2 + Hb ⇌ Hb4O2
cooperative binding
binding of first oxygen molecule results in conformational change in structure of haemoglobin molecule→ easier for each successive oxygen molecule to bind
How is carbon dioxide transported around the body
dissolves directly in blood plasma
binds to haemoglobin→ forms carbaminohaemoglobin
most transported as hydrogen carbonate (HCO3-)
formation of HCO3- ions
CO2 diffuses into RBC from plasma
In RBC, carbon dioxide combines with water to make carbonic acid:
CO2 + H2O ⇌ H2CO3
carbonic anhydrase catalyses reaction
Carbonic acid readily dissociates into H+ and HCO3- ions:
H2CO3⇌ HCO3– + H+
H+ ions combine with haemoglobin→ forms haemoglobinic acid:
acts as a pH buffer
Hydrogen carbonate ions diffuse out of RBC into plasma
The chloride shift
movement of chloride ions into RBC→ occurs when hydrogencarbonate ions are formed
negatively charged hydrogencarbonate ions transported out of red blood cells
negatively charged chloride ions transported into RBC via transport proteins→ prevents electrical imbalance
oxygen dissociation curves
shows rate at which oxygen associates and dissociates with haemoglobin at different partial pressures of oxygen
partial pressure of oxygen
pressure exerted by oxygen within mixture of gases→ measure of oxygen concentration
affinity for oxygen
ease with which haemoglobin binds and dissociates with oxygen
high affinity→ binds easily and dissociates slowly
low affinity→ binds slowly and dissociates easily
explanation of oxygen dissociation curve
shallow gradient at start→ difficult for 1st oxygen molecule to bind
after first O2 molecule binds, protein changes shape→ easier for next oxygen molecule to bind ∴ steeper gradient in middle
levels off at end→ less remaining binding sites so longer for 4th oxygen molecule to bind
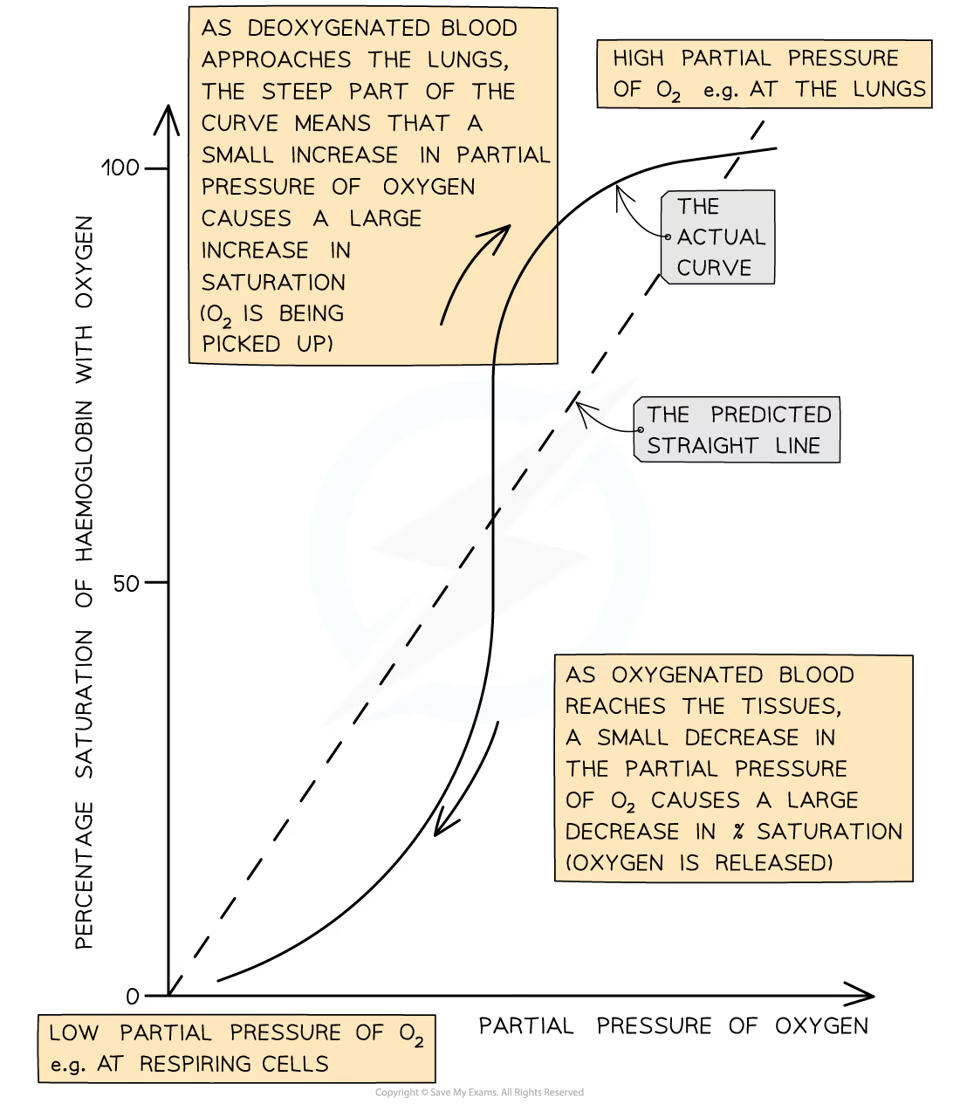
interpretation of oxygen dissociation curves
low pO2:
oxygen binds slowly to haemoglobin
low affinity for oxygen at low pO2
medium pO2:
oxygen binds more easily to haemoglobin
saturation increases quickly
small increase in pO2=large increase in haemoglobin saturation
high pO2
oxygen binds easily to haemoglobin→ can pick up oxygen and become saturated as blood passes through lungs
high affinity for O2 at high pO2
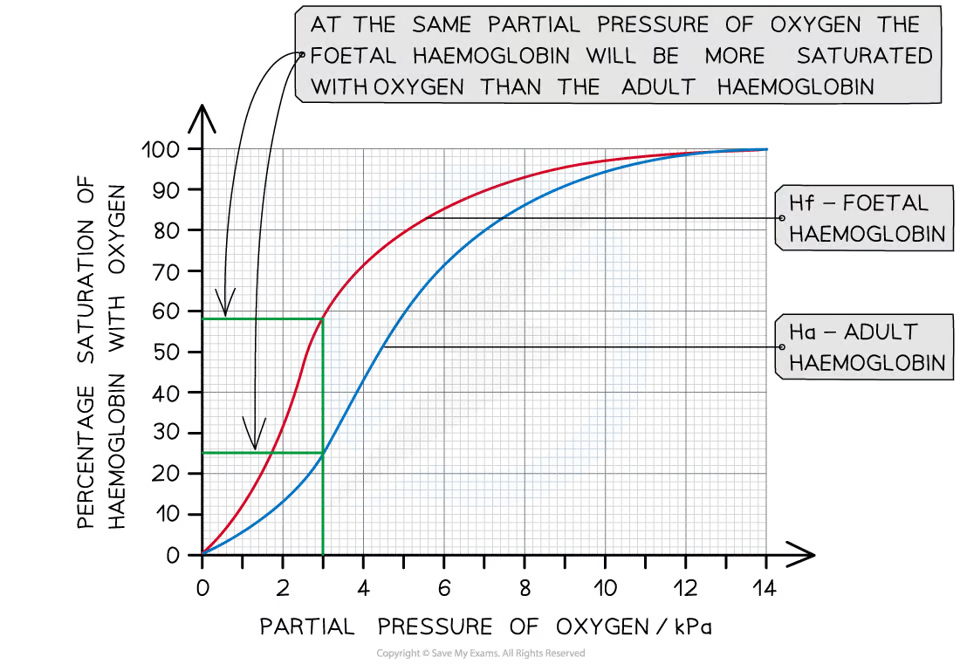
foetal haemoglobin
higher affinity for oxygen than adult haemoglobin
allows foetus to obtain oxygen from mother’s blood:
foetal haemoglobin can bind at low pO2
at low pO2, mother’s haemoglobin is dissociating with oxygen
after birth, baby produces adult haemoglobin→ gradually replaces foetal haemoglobin:
important for release of oxygen in respiring tissue
types of haemoglobin
haem groups same
globin chains can differ between species→ determine precise properties of haemoglobin
can bind to oxygen in different conditions→ adaptations
effects of altitude on haemoglobin
pO2 is lower at higher altitudes
haemoglobin adapted to conditions→ binds more readily