RADT W15 Identification of Restoration, Interpretation of Dental Materials and Foreign Objects; Dental Caries
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
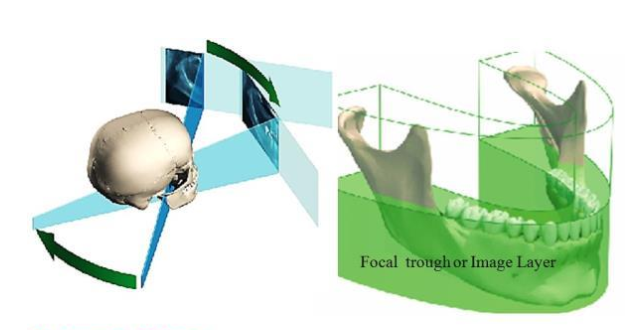
Why does the metal crown not create a ghost image?
Ghost images/artifacting is created when that object is OUTSIDE of the zone of focus/image layer
List the following from least radiolucent to most radiolucent.
Least radiolucent → porcelain → composite resin → acrylic → most radiolucent
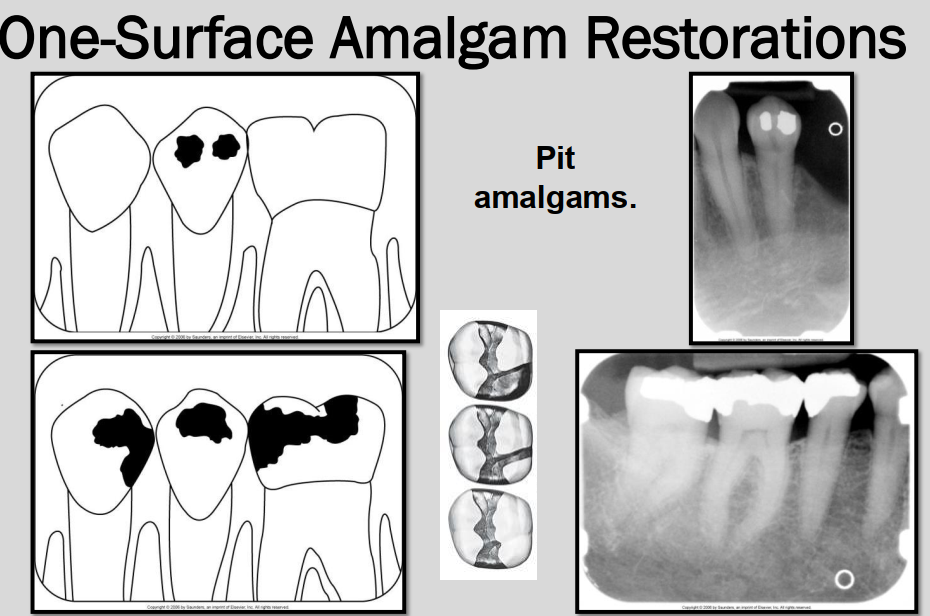
T or F One-surface Amalgam restorations appear as distinct, small, round or ovoid radiopacities.
TRUE

What is this ? → dense radiopacities with irregular borders.
Fragments of amalgam embedded in adjacent soft tissue during restoration → aka Amalgam tattoo.
Clinically seen as blue-ish pigmentation in the gingiva

How do gold restorations and amalgam restorations differ on a radiograph?
Gold restorations have a smooth marginal outline vs amalgam which has an irregular outline.
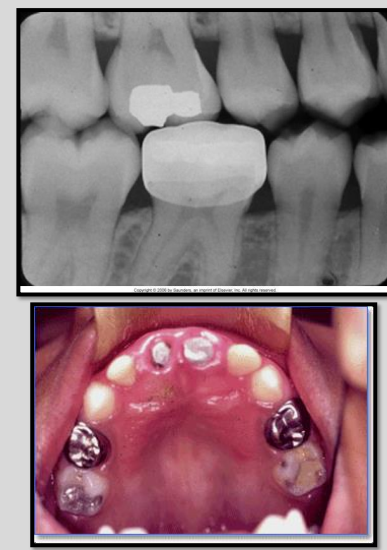
How are stainless steel and chrome crowns differentiated on a radiograph from amalgam or gold restorations?
SS crowns and chrome crowns have smooth and regular margins
usually used as a temporary restoration
Thin and do not absorb as much xrays → appear radiopaque but not as densely as amalgam or gold
may have some “see-through”ish areas on radiograph.
Describe the appearance of an all-porcelain crown on a radiograph.
Thin radiopaque line outlining the prepared tooth that represents cement
cement may be seen through the slightly radiopaque porcelain crown
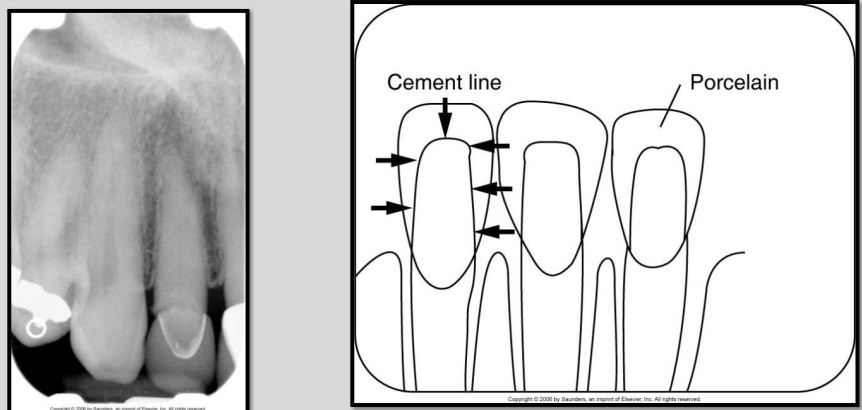
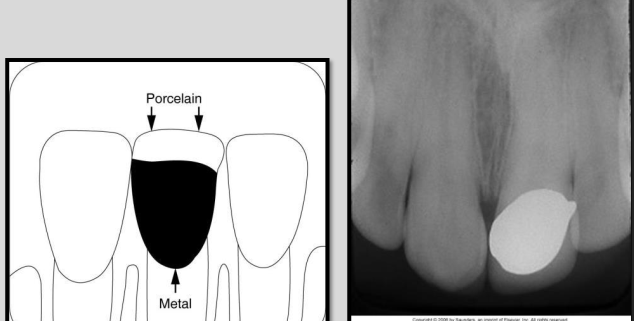
Describe the appearance of Porcelain-fused-to-metal crown on a radiograph.
The metal component appears completely radiopaque
Porcelain components appears slightly radiopaque.
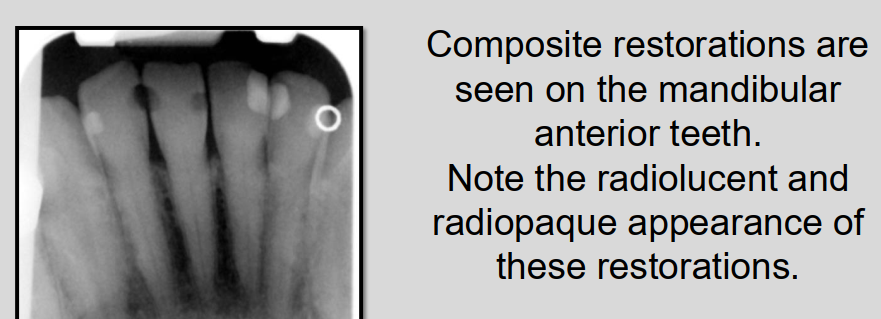
Describe the appearance of Composite restorations.
Appearance can vary on radiographs from radiolucent to slightly radiopaque
density depends on the composition of the composite material
Describe the appearance of acrylic restorations on a radiograph.
Acrylic is the least dense of all non-metallic restorations.
Appears radiolucent or barely visible on radiographs
often only used as an interim/temporary crown/filling
What are base materials? What is an example of a base material?
Base materials are used as cavity liners placed on the floor of a cavity preparation to protect the pulp
ex. Zinc oxide eugenol (ZOE) → a cement applied on floor of cavity prep → appears radiopaque.
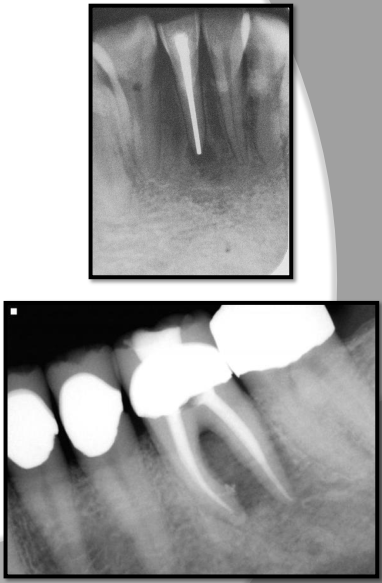
What are metallic pins? what are they used for?
Metallic pins are used to enhance retention of amalgam or composite
appear as cylindrical or screw-shaped radiopacities.
What are Gutta percha?
Gutta percha - clay-like thermoplastic material used in root canal therapy to obliterate the pullp canals.
appears radiopaque similar to base materials
less radiodense than metallic restorations.

What are silver points?
Silver points are used to obliterate pulp canals and appear more radiodense than gutta percha on a xray film.
used in endodontics
Describe the appearance of complete dentures on a radiograph.
looks like rootless or floating teeth.

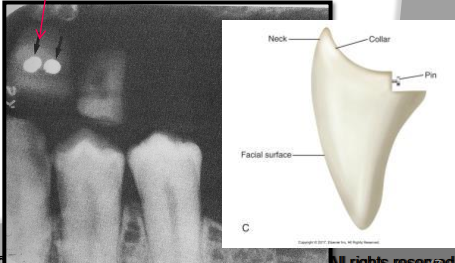
What are diatorics?
Metal retention pins found on the anterior porcelain denture teeth
tiny dense radiopacities superimposed over the denture teeth.
Describe partial dentures and their appearance on a radiograph.
Removable partial dentures (RPD)
have a metal base with acrylic saddles
appears densely radiopaque where metal is
slightly radiopaque in areas of acrylic

T or F - Oral surgery materials appear radiolucent on a dental radiograph with varying sizes, shapes and design.
F - they appear radiopaque.

Glasses on PAN

Daisy chain

hearing aid
Caries definition.
Destructive process causing decalcification of enamel followed by the destruction of enamel and dentin and cavitation of a tooth.
cavitation defn: formation of empty space in a solid object; “creating a cavity”
T or F - Dental caries appear radiopaque on a radiograph.
F - they appear radiolucent
What is the most common bacteria associated with dental cavities?
Streptococcus mutans
What are the 3 pre-requisites for caries development?
Cariogenic bacteria
Supply of substrate for acid production (food)
Susceptible host → factors such as composition of teeth and saliva
What are 3 colour indicators when identifying caries clinically?
Occlusal surfaces may show DARK staining in fissures, pits and grooves
Smooth surfaces may exhibit CHALKY WHITE spot or opacity
Interproximal ridge may appear DISCOLOURED
What tools are useful for identifying caries during a clinical examination? What are each of their uses?
mouth mirror → indirect vision, transillumination*, retraction
*Healthy enamel will allow light through, areas with caries will appear darkened
explorer → tactile detection for inconsistencies (if it catches on anything in pits, fissures, and grooves.
compressed air → dry teeth and remove debris for visibility; dry dry dry and dry again.
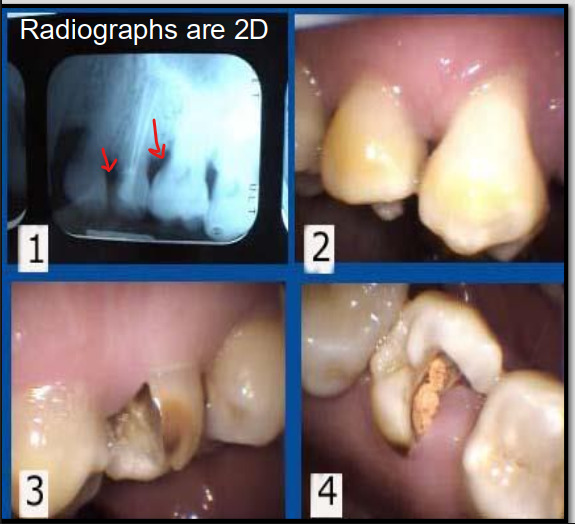
Why are caries farther advanced clinically than what you can see on a radiograph?
Radiographs show a 2D image of a 3D object which can lead to underestimation of the lesions extent.
Lesions can be deeper than they appear on the radiograph.
T or F - Early demineralization changes can affect the density of the tooth making it obvious on a radiograph.
F - Early demineralization DOES NOT affect the density of the tooth so the increased penetration of the x-ray beam is NOT evident on radiographs
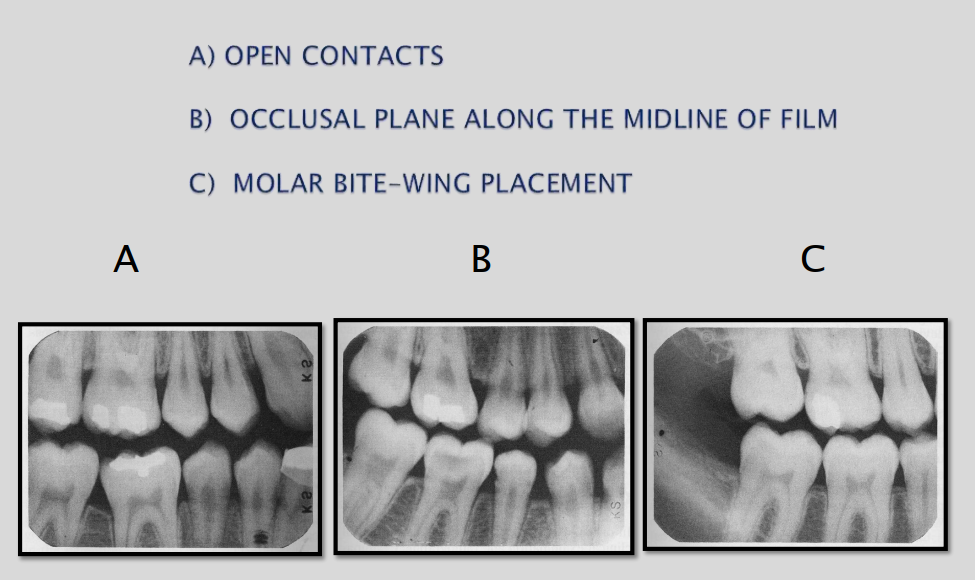
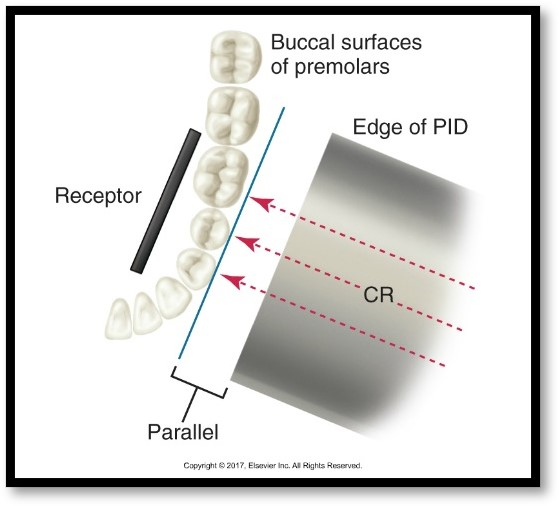
3 Criteria for a bite-wing exposures
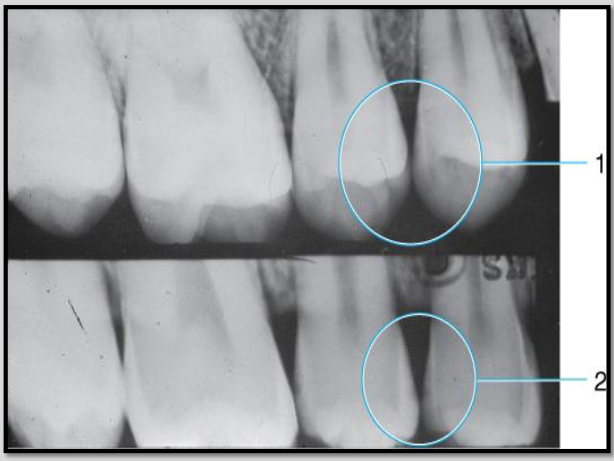
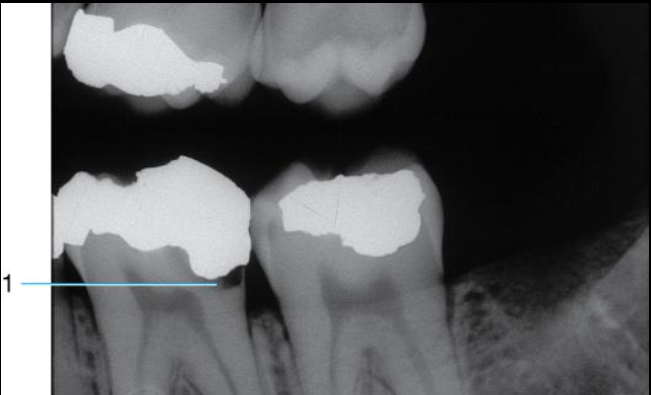
What does #1 show?
#1 shows INCORRECT vertical angulation
it is over angulated thus obstructing the interproximal view of the lesion
#2 shows CORRECT vertical angulation
interproximal caries now visible on the radiograph.
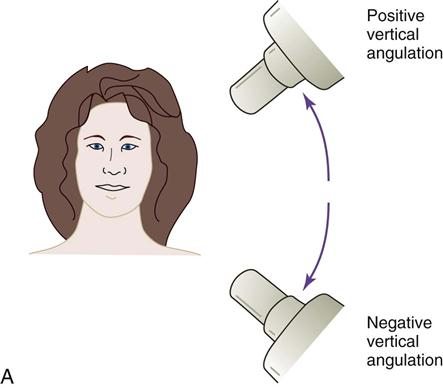
**vertical angulation = tilting PID up or down
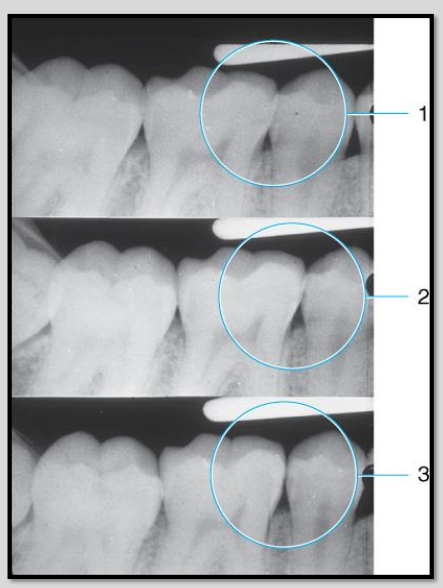
Correcting horizontal angulation for open contacts.
Open contacts are important for revealing interproximal caries.
Image 1 overlap hiding the caries
Image 2 has better horizontal angulation but still some overlap
Image 3 open contacts shows full extent of interproximal caries.
Where is cervical burnout most likely to be imaged on a radiograph?
Apical to the gingival margin
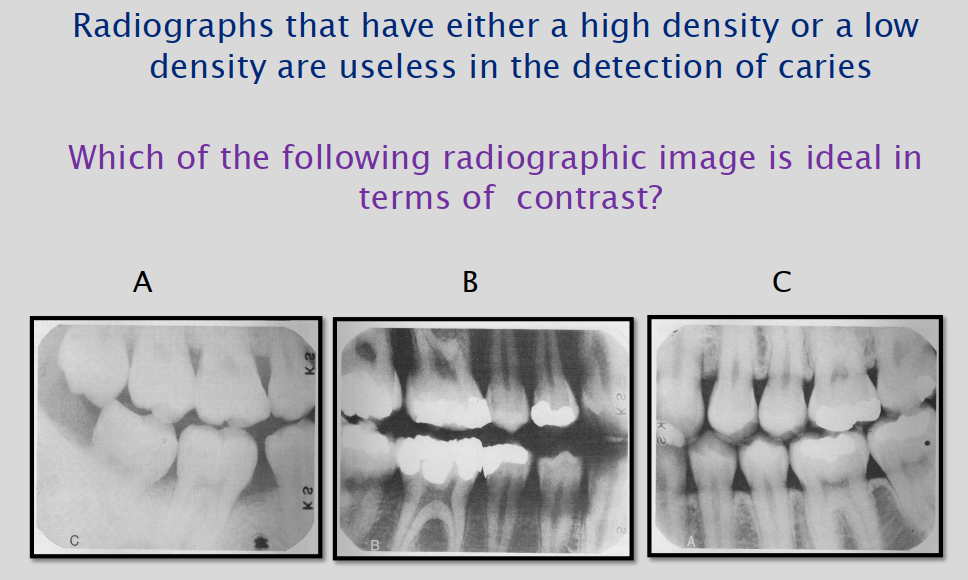
T or F - High contrast films are recommended for bitewing films because optimal contrast enhances caries detection.
TRUE
Answer for Image: C
What are the 6 RADIOGRAPHIC classifications of Caries?
Interproximal
Occlusal
Buccal and Lingual
Root surface
Recurrent
Rampant
Describe interproximal caries.
Interproximal caries occur between 2 adjacent surfaces
typically seen at or just below contact point radiographically
clinically → chalky white spot or stained area followed by cavitation
3-4 years may elapse before interproximal caries become CLINICALLY apparent.
T or F - As caries progresses through enamel, it typically creates a rectangular configuration. When it reaches the DEJ, it spreads laterally and progresses through dentin.
F - creates a TRIANGULAR configuration.
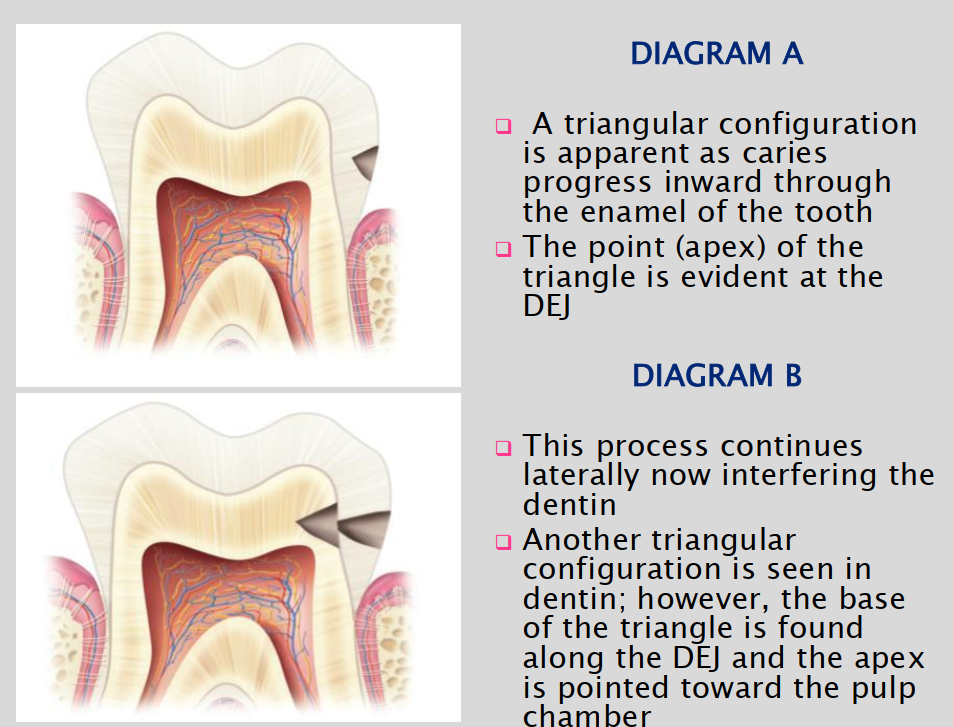
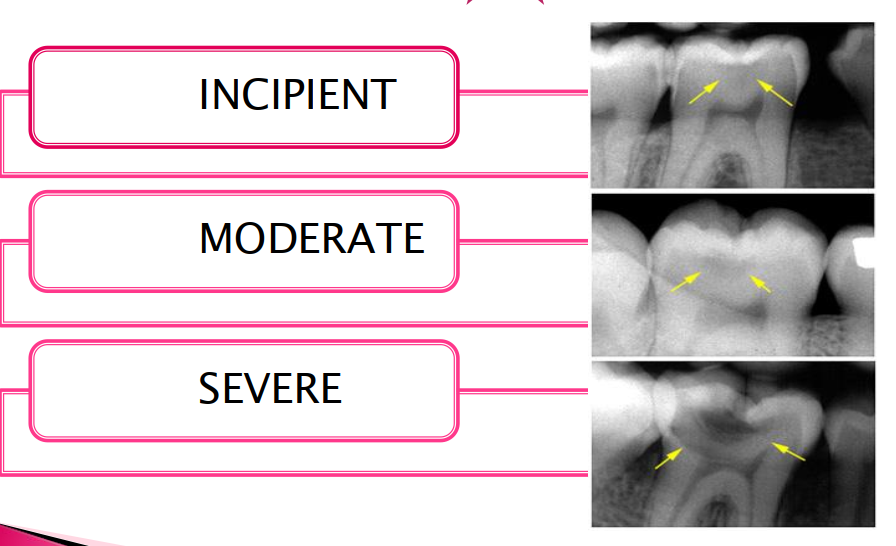
What are the 4 Interproximal dental caries classifications ?
Class 1 = Incipient → beginning stages; small; only seen on enamel; tiny radiolucent notch; extends less than halfway through enamel thickness
Class 2 = Moderate → extends more than halfway through enamel thickness but NOT involving DEJ; evident only on enamel; radiolucent triangle
Class 3 = Advanced → extends INTO or THROUGH DEJ but not more than half way through dentin towards pulp.; affecting enamel and dentin
Class 4 = Severe → extends THROUGH enamel and dentin and more than half the distance to pulp
** NOT THE SAME AS BLACKS CLASSIFICATION.
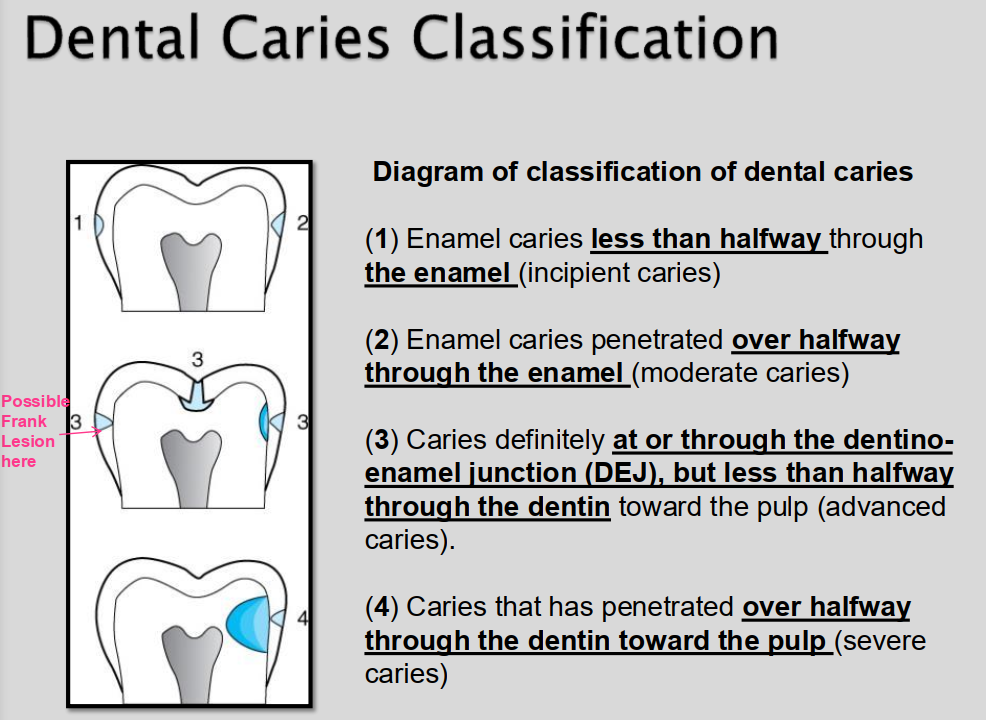
What are Frank caries?
Overt or Frank caries are used to identify caries that REACH THE DEJ.
caries lesion that minimally penetrates dentin
may or may not involve cavitation
frank lesions and incipient lesions are NOT the same

What class of interproximal caries is this?
Class 1 - incipient lesion

What class of interproximal caries is this?
Class 2 - Moderate

What class of interproximal caries is this?
Class 3 Advanced
What class of interproximal caries is this?
Class 4 Severe
Describe Occlusal caries
Caries involving the chewing surface of posterior teeth
Thorough clinical exam is method of choice for occlusal caries
CANNOT BE SEEN ON RADIOGRAPH UNTIL DEJ INVOLVEMENT
Describe the 3 levels of occlusal caries.
Incipient → cannot be seen on radiograph; only detected clinically; use explorer
Moderate → thin radiolucent line in dentin; located under enamel of occlusal surface; little radiographic changes noted in enamel; spreads laterally extending downward towards pulp once DEJ involved
Severe → large radiolucency extending through enamel and dentin beyond DEJ; clinically appears as hole or cavity in tooth

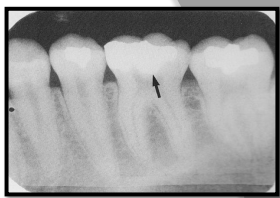
Classify this carious lesion.
Occlusal caries - moderate
Classify this carious lesion
Severe Occlusal caries
Why might air abrasion used on occlusal surfaces for caries detection?
Removes surface debris and stains → improves visibility of fissures and pits.
Opens up narrow grooves → allows clearer access for visual or laser-based caries detection.
Helps differentiate between stain and demineralization.
Provides a clean, dry surface, enhancing accuracy of diagnostic tools (e.g., DIAGNOdent, visual inspection).
Can expose incipient lesions that were hidden under plaque or debris.
T or F - Buccal and lingual caries are best detected radiographically. Why?
FALSE - best detected clinically due to the SUPERIMPOSITION of densities of normal tooth structure.
Radiolucency may appear better define if lesion is located on the _____ surface because of the close approximation of the film to the caries area.
LINGUAL
Identify the carious lesion.
Buccal caries
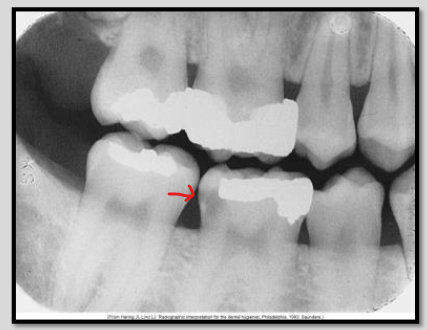
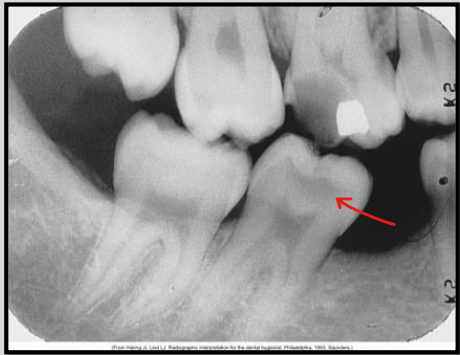
Describe root surface caries.
Involves cementum and dentin; NO ENAMEL INVOLVEMENT
Early lesions may be difficult to detect on radiograph
Typically occurs just below cervical region of the tooth
Bone loss and gingival recession must be evident
Describe the clinical and radiographic appearance of Root surface caries
Clinical → easily seen on exposed root surface; SAUCER-SHAPED; brownish colour; leathery texture
Radiographic → cupped-out or crater-shaped radiolucency; interproximal just below CEJ
T or F Root surface caries are most commonly seen on maxillary premolars and molars
FALSE - most common for MAND PM and Molars

Identify the carious lesion.
Root surface caries
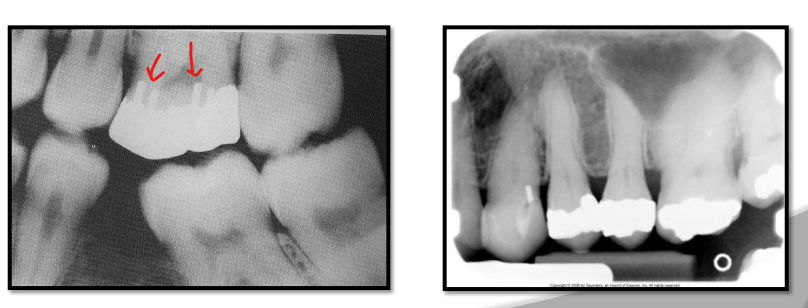
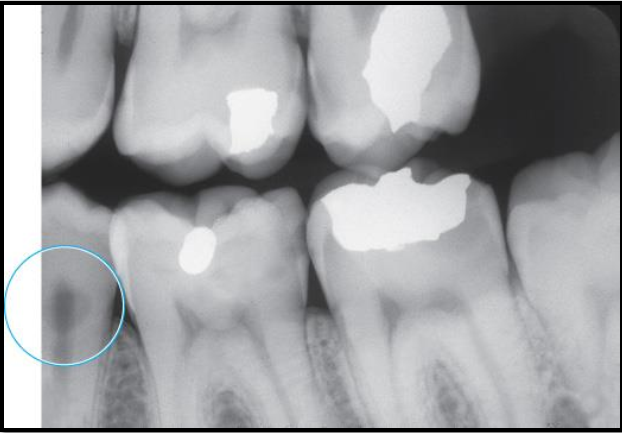
Describe Recurrent caries
AKA Secondary caries
Evident adjacent to pre-existing restoration due to inadequate cavity prep, defective margins, or incomplete removal of caries prior to placing restoration
appears as radiolucent area just beneath restoration on radiograph.
Describe Rampant caries.
Rampant caries refers to growing or spreading caries.
Advanced and severe affecting numerous teeth (can happen to both primary and permanent dentition)
Happens in children with poor dietary habits, nursing bottle syndrome or in adults with xerostomia (dry mouth) due to mediations.
Can also be a secondary condition to chemo radiation therapy

What are 4 conditions that can resemble caries on a radiograph?
Restorative material
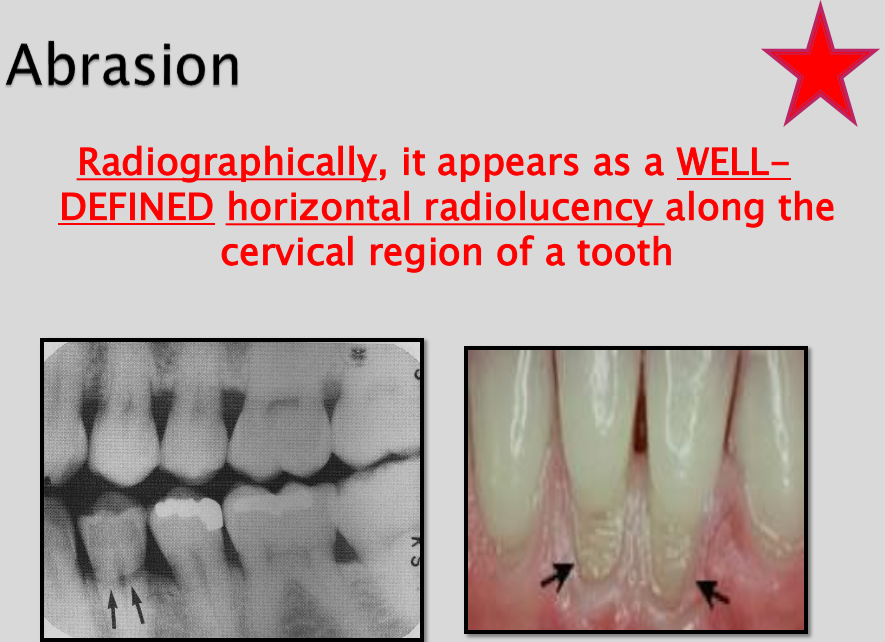
Abrasion
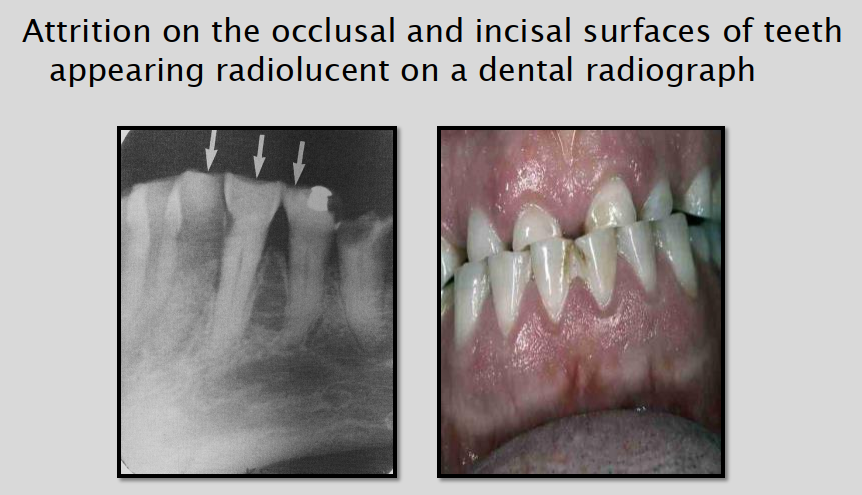
Attrition
Cervical burnout
________ appears clinically as a hard, highly polished defect in the dentin with a V-shaped wedge at cervical margin.
Abrasion
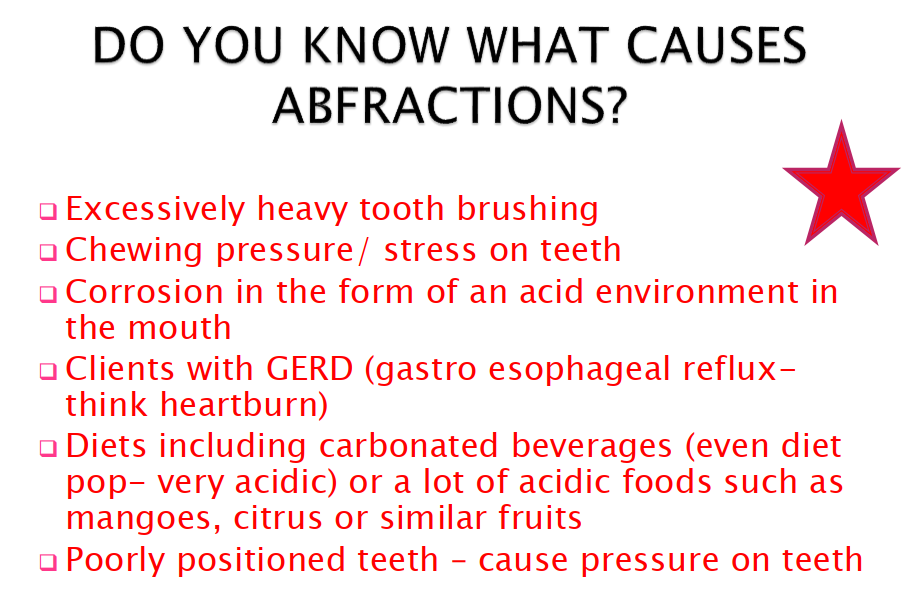
Describe the appearance of Abfraction
small cracks or notches in the teeth → due to clenching, chewing and biting pressures on teeth
cracks and splits in enamel
shining bright light on the tooth reveals VERTICAL lines of Abfraction on the length of the tooth.
How do we distinguish Attrition from Carious lesions?
We use clinical examination to differentiate.
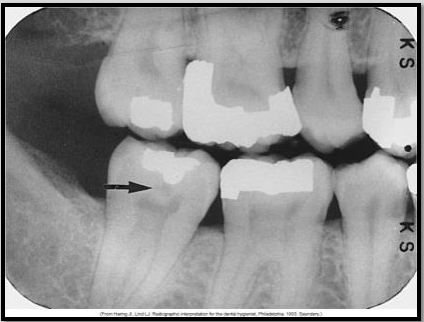
Describe cervical burnout.
Appears as a collar or ill-defined wedge shaped radiolucency on the mesial and distal root surfaces near CEJ
May confuse with root caries
Artifact results from difference in densities of adjacent tissues
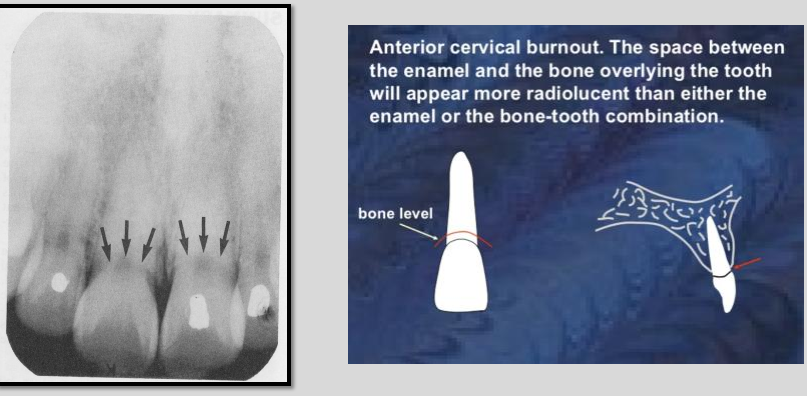
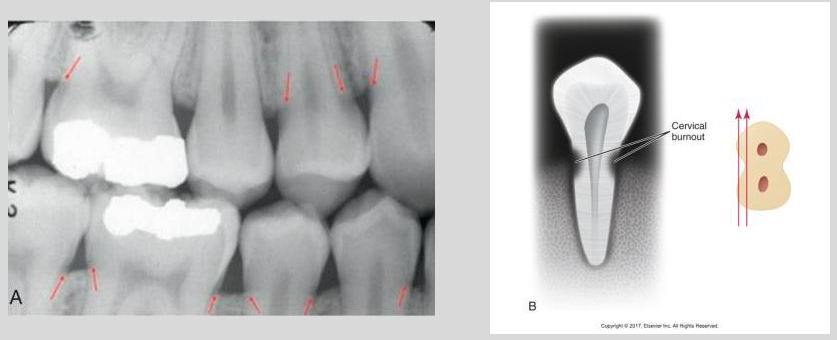
Cervical burnout on posterior teeth
Not to be confused with posterior teeth root caries
Questions to ask yourself when viewing radiographs:
Evidence of severe interproximal caries?
Evidence of overhang?
Evidence of recurrent decay?
Evidence of Subgingival calculus?
Evidence of Gingivitis?