Serotonergics + Adrenergics- AUSTIN
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
Symptoms of depression:
anhedonia (ex: what used to be fun, now is not)
avolition (lack of goal directed behavior)
apathy (don’t care)
lethargy (change in energy levels)
cognitive
sadness, anxiety, guilt, worthlessness
thoughts of self, harm, self-destruction
What is the most important part of the brain effected in depression?
hippocampus—> important for forming, and maybe storage of episodic memories
What brain changes are seen in depression:
structural changes—> decrease neuron density and atrophy
associated w/ HPA axis activation and BDNF
connectivity changes
amygdala, ACC, hippocampus
changes in NT activity
activity changes
baseline changes
response to stress
What is the monoamine hypothesis associated with depression?
what evidence is there for and against this hypothesis?
pathophys of depression is associated w/ decreased activity of monoamines in the CNS
monoamines: serotonin, dopamine, NE
evidence for:
any substance that increases monoamine has antidepressant properties
inhibiting MAO improves mood
reserpine (blocks VMAT) causes depression
evidence against:
delay in clinical efficacy following increased levels of monoamines
only 50-70% of pts. experience full response to therapies that target monoamines (think: if monoamine hypothesis was 100% true than all pts. should respond)
There is no known single underlying cause of depression.
What are some things associated/observed with depression?
genetic
environment (ex: stress, trauma)
HPA-axis abnormalities
increased cortisol associated
Sickness behavior
increased level of pro-inflammatory mediators associated
What is the neurotrophic hypothesis associated with depression?
basically—> Longitudinal Changes are seen
Early depressive episodes are often "reactive" (triggered by stress), but later episodes become more "endogenous" (spontaneous), suggesting cumulative brain changes
austin ex: say your house burns down—> okay youre upset… but then shortly after you crash your car, lose your job—> you start to think “endogenously” or to yourself that bad things are going to happen to you
Hippocampus and other parts of the brain volume decrease correlates with the duration of untreated depression, implying a positive feedback loop (“sad makes more sad”)
Altered signaling of what transmitters in addition to monoamines is associated with depression?
glutamate and GABA
What is the role of SERT?
removes serotonin from the synapse by reuptake
What is the role of NET?
removes NE from the synapse by reuptake
which autoreceptors of 5-HT and NE are inhibitory?
a2 autoreceptors—> inhibitory
5HT1B—> inhibitory
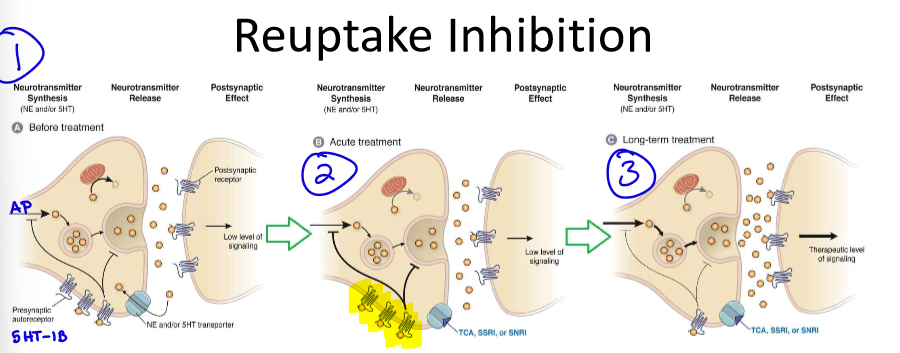
Why does the clinical effect seen with reuptake inhibition take weeks to see?
OVERALL THEORY: chronic use leads to downregulation of inhibitory autoreceptors
when we take acute treatment—> autoreceptors are flooded and shuts down pre synpase= doesn’t allow NT release DESPITE inhibiting reputake
over time—> downregulate autoreceptors and now the synapse can flood with NTs
other theories: long-term tx may increase transcription factors and growth factors—> leading to neurogenesis (brain growth)
All antidepressants have what BBW?
suicidality
What different classes of drugs can be used for depression:
reuptake inhibitors
TCAs
SSRIs
SNRIs
degradation inhibitors
MAOIs
others:
bupropion
mirtazapine
trazodone
serotonin modulators
TCAs are extremely hydrophilic or lipophilic?
what are the advantages/disadvantages to this?
TCAs= extremely LIPOphilic
advantages: good PK, can cross the BBB
disadvantages: low selectivity for receptors
MOA of TCAs:
Inhibits Serotonin and NE reuptake
selectivity depends on whether it’s a tertiary or secondary amine (tertiary TCAs have increased selectivity for 5HT)
In addition to its main MOA, TCAs also have activity at what receptors?
antagonist: 5HT, NMDA, a1, histamine, muscarinic receptors
agonist: sigma
blocks sodium and L type calcium channels
BBW of TCAs:
suicidality in children, adolescents, and young adults (24 and younger)
What are the effects seen with TCAs?
explain each pharmacologically when applicable (aka what receptor is responsible for that effect)
antidepressant (from NE and 5-HT reuptake inhibition)
analgesic
sedation (H1, M)
orthostatic hypotension (a1)
dry mouth (M)
weight gain (H1)
sexual dysfunction
arrhythmias (sodium and calcium channel blockade)
lower seizure threshold
Names of the TCAs:
which are tertiary amines? which are secondary?
amitriptyline- tertiary
clomipramine
Doxepin
Imipramine
desipramine- secondary
nortriptyline
Why do we want to avoid abrupt discontinuation with SSRIs?
exception to this?
avoid abrupt d/c bc may cause flu-like symptoms, mood changes, tremor, n, dizziness, palpitations
EXCEPTION: fluoxetine bc of its long t ½
MOA of SSRIs:
INHIBIT SEROTONIN REUPTAKE
SSRIs have less activity at other receptors compared to TCAs. What is the implication of this?
SSRIs have decreased risk of ADRs
List the SSRIs:
Citalopram
Fluoxetine
Fluvoxamine
paroxetine
sertraline
Because SSRIs are so structurally different from each other, how do we compare them?
SERT selectivity (aka we look for how high of an affinity the drug has to SERT)
What are the common shared structural features between all SSRIs?
e- withdrawing group (nitro, acetyl, halogen) at para position of non-fused aromatic ring
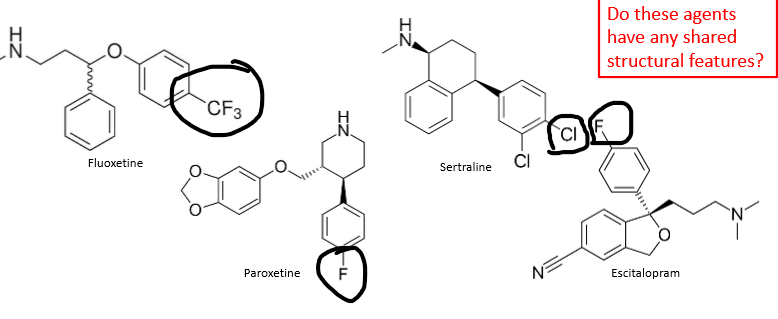
Where do SSRIs bind to on SERT?
exception?
bind to primary/orthosteric site
exception: escitalopram ALSO binds to allosteric site
(makes it work better)
What SSRI is the most selective?
What SSRI is the most potent?
most selective—> escitalopram
most potent—> paroxetine
The #1 thing we use to determine what SSRI to use is the ADRs.
What ADRs are seen from SSRIs? BBW?
GI
n/v/d
GI bleed risk
appetite/weight changes (can be ↑ or ↓)
CNS
HA
insomnia/fatigue
anxiety/agitation/mania
tremors/seizures
BBW for suicidal thoughts and behaviors in pediatric and young adult pts.
others:
serotonin syndrome
sweating
sexual dysfunction
hyponatremia
withdrawal symptoms
anticholinergic effects*
arrhythmias*
*= not seen in all
Most SSRIs are pregnancy category __. What is the exception?
most are pregnancy cat C
exception: paroxetine is cat D—> risk of heart defects, esp in 1st trimester
Do SSRIs have any food considerations?
Metabolized by what main CYP?
can take w/ or w/out food (austin recommends with)
metabolized by CYP2D6, 2C19, 3A4
Answer the following about specific SSRIs:
which has the longest t ½ ?
has the greatest probability of weight loss/anorexia?
most likely to cause diarrhea?
does not inhibit CYP3A4/ has the least enzyme interactions?
most likely to prolong the QT interval?
which are basic?
fluoxetine
fluoxetine
sertraline
citalopram
citalopram
ALL SSRIs are basic
MOA of SNRIs:
Inhibits serotonin and NE reuptake
REVIEW:
Compare the MOAs of TCAs, SSRIs, and SNRIs
TCAs | SERT + NET + other receptors |
SSRIs | SERT |
SNRIs | SERT + NET |
Which is preferred—> SSRIs or SNRIs?
either or—> studies found no clinically significant difference between the two
How do SNRIs play a role in neuropathic pain?
NET inhibition
List the SNRIs:
Venlafaxine
Duloxetine
Desvenlafaxine
Milnacipran
Levomilnacipran
ADRs of SNRIs:
Similar to SSRIs!!!
GI, CNS, sexual dysfunction, serotonin syndrome
INCREASE in blood pressure (bc of NET/adrenergic)
SWEATING
bleeding risk
withdrawal syndrome
SNRIs are metabolized by what CYP?
CYP2D6, 3A4, 1A2
MOA of MAOIs:
difference between MAO-A and MAO-B
inhibit of monoamine oxidase
prevents intracellular of monoamines
MAO-A: metabolizes DA, NE, 5-HT, tyramine
MAO-B: metabolizes DA, tyramine
What antidepressant reacts with cheese, beer, and wine? (known as the “cheese” reaction)
MAOIs
Explain why the cheese reaction occurs:
these foods contain tyramine
tyramine is metabolized by MAO
if we inhibit MAO with MAOIs then tyramine (which is structurally similar to NE)—> displaces vesicular NE—> NE is not metabolized
SHORT term results:
risk of HTN, tachycardia, arrhythmias (hypertensive crisis)
LONG term results:
tyramine stored in vesicles and hydroxylated to octopamine (instead of NE)
when the SNS is activated—> octopamine is released instead of NE, which does not have any vasoconstriction/contraction = decrease BP
austin simplied example: basically blocks metabolism of these foods—> gets into CNS/PNS and displaces NE= makes NE flood out —> heart problems
For MAOIs:
BBW
ADRs
Interactions
BBW—> suicidal thoughts and behavior in pediatric and young pts.
ADRs:
CNS (HA, drowsiness, lighthead)
GI (n/v/d)
sexual dysfunction
others: orthostatic hypotension, anticholinergic, paresthesia
Interactions
SO MANY THINGS
significantly increases risk of serotonin syndrome
List the MAOIs:
Isocarboxazid
Phenelzine
Tranylcypromine
Selegiline
Rasagiline
Are most MAOIs reversible or irreversible inhibitors?
irreversible
What is the triad of effects seen with serotonin syndrome?
cognitive: mental status changes, HA, hallucinations
somatic: hyperrflexia, tremor, myoclonus
autonomic: hyperthermia, n/v/d, tachycardia, sweating
Serotonin Syndrome and NMS are difficult to differentiate. What are the key differences?
In serotonin syndrome—> there will be pupil dilation and reflexes not seen in NMS
Tx for serotonin syndrome?
ciproheptadine (5-HT antagonist)
SUPPORTIVE CARE—> #1 is GET RID OF THE CAUSE
WHAT IS THE WORST COMBO WHEN IT COMES TO SEROTONIN SYNDROME?
MAOI inhibitor + SSRI
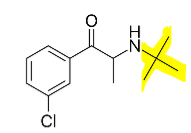
MOA OF BUPROPION?
HAS NO EFFECT ON WHAT????? UNIQUE!!!!!!!!!
inhibits reuptake of NE and DA
NO EFFECT ON SEROTONIN
ADRs of Bupropion:
DOSE-DEPENDENT DECREASE OF SEIZURE THRESHOLD
stimulant-like effect
n/v/d
weight loss, INCREASED LIBIDO
diaphoresis, blurred vision
What functional groups on Bupropion are essential for function? why?
bulky t-butyl group prevents oxidative metabolism
protects the Nitrogen for drug efficacy
prevents drug from forming metabolites that act like meth
MOA and ADRs of Trazodone and Nefazodone?
net effect?
MOA:
5-HT1A partial agonist
5-HT2A, a, H1 antagonist/inverse agonist
minimal SERT inhibition
net effect: enhance 5-HT and NE release
ADRs:
extreme drowsiness
CV
What is a rare ADR associated with trazodone?
priapism
MOA and ADRs of Mirtazapine?
net effect?
MOA:
a2 antagonist (primary)
5-HT2A,2C,3 ,H1 antagonist/inverse agonist
net effect: enhance 5-HT and NE activity
ADRs:
increased appetite/weight gain
sedation
Note: decreased risk of sexual ADRs and serotonin syndrome
How does a2 antagonism with Mirtazapine lead to enhancement of 5-HT and NE activity?
increases release of monoamines (inhibits the inhibitor)
a1 activation by NE on serotonin is excitatory
net effect: decrease in inhibition of serotonergic signaling
What is the MOA of Vilazodone and Vortioxetine?
ADRs?
CYP?
MOA: SERT inhibition, 5-HT1A partial agonists
vortioxetine: 5-HT3 antagonism, 5-HT1B antagonism/partial agonism
ADRs: n/v/d
CYP2D6
What is Allopregnanolone approved for?
BBW?
MOA?
approved for POSTPARTUM depression
BBW: excessive sedation, loss of consciousness
MOA: positive allosteric modulator at GABA-A receptor, antidepressant MOA unclear
For Ketamine:
MOA?
ADRs?
NMDA receptor antagonist, antidepressant mechanism unclear
ADRs: CV, rash, GI, dependence