PHSL 3051 pulmonary
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
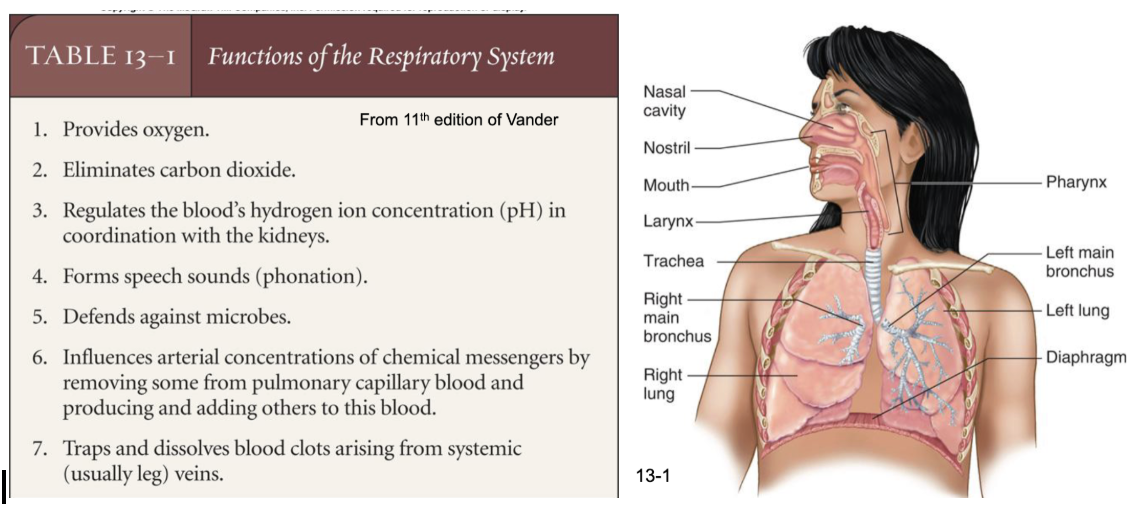
functions of the respiratory system
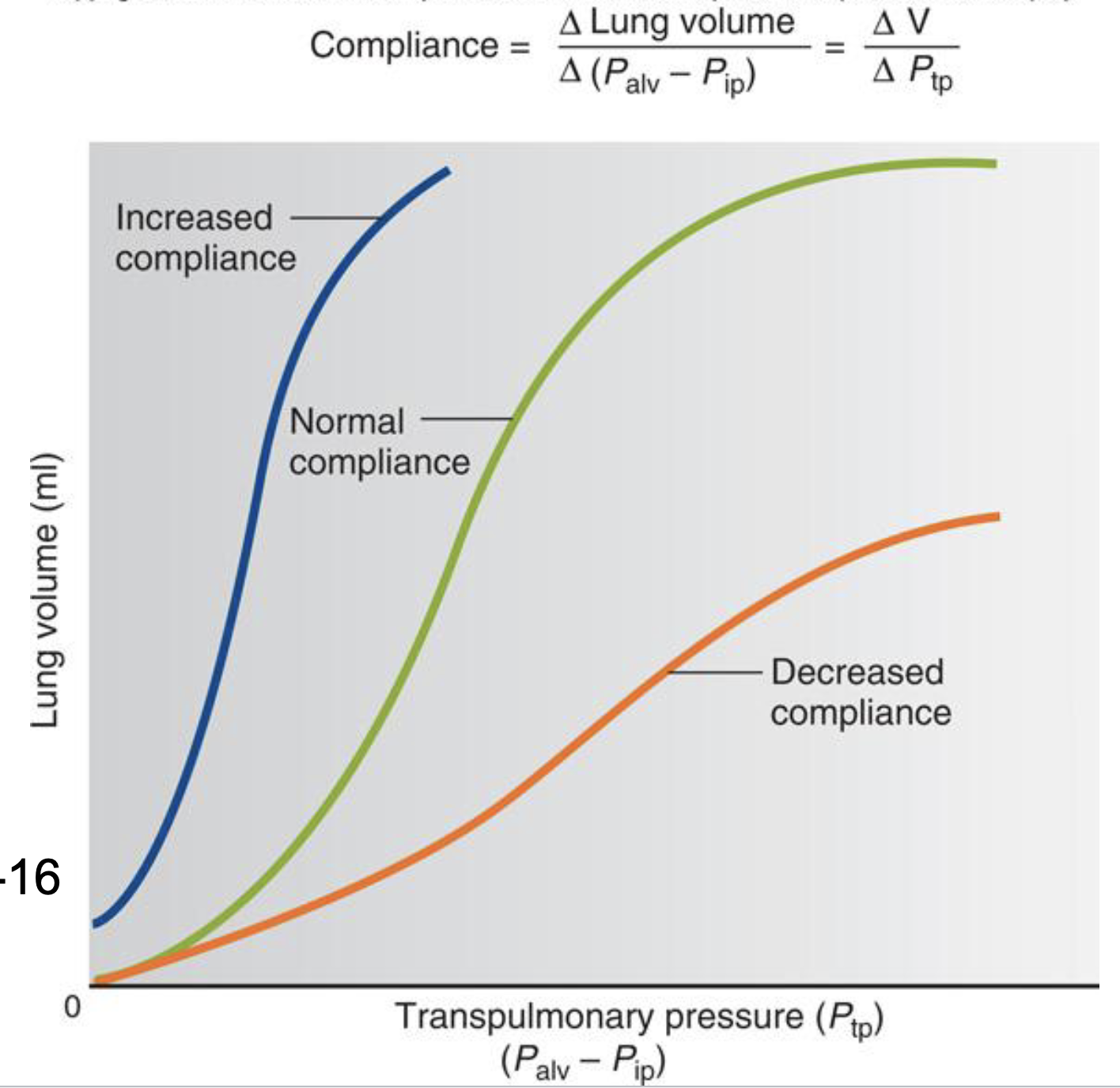
complience
the change in pressure is needed to inflate the lungs to a certain volume
lung tissue matrix is a weave of elastin and collagen fibers
lungs that are more compliant are “stretchier” - it takes low pressure to inflate them
stiff lungs cause restrictive lung disease
emphysema destroys the weave (easy to stretch out, hard to recoil)
surface tension
allows water particles to stick together - like beading of water on a slick window
high surface tension makes alveoli more likely to collapse (harder to open)
different sized alveoli have different collapsing pressures with equal ST
surfactant lowers ST and lowers it more in the small alveoli so that pressures are equalized
surface tension in action - what if the water (saline) in your lungs formed beads?
the alveoli would collapse and pull water in the lungs
you would not be able to breath
**this is why we need surfactant
law of laplace
when two alveoli with different sizes dont have surfactant, their surface tension will be the same; this then creates a pressure gradient between the two alveoli
the small alveoli will collapse and blow up the big alveoli
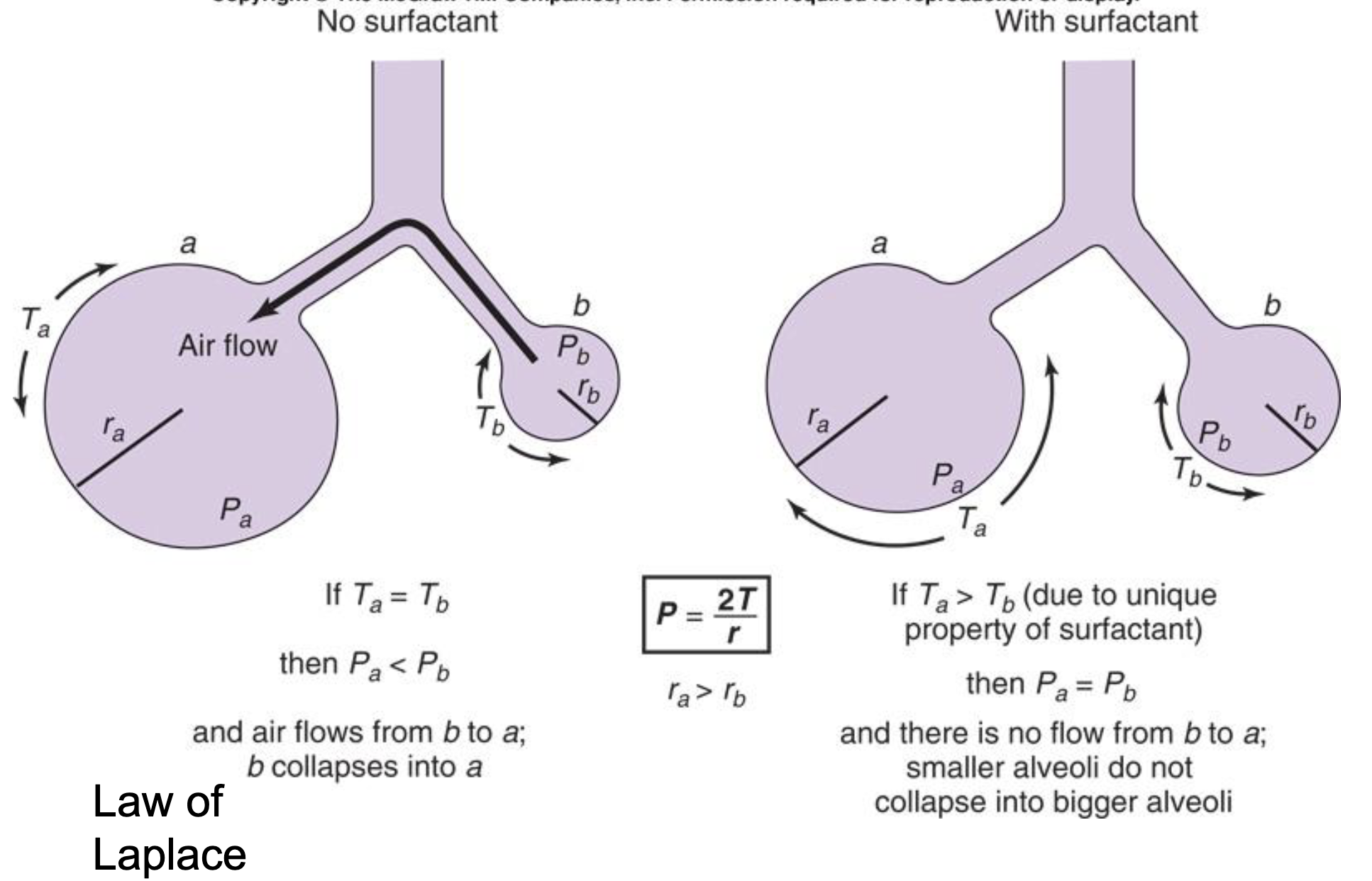
the presence of surfactant (review)
lowers surface tension
increases compliance
equalizes pressures between two different areas of the lungs
overall stabilizes different areas of the lungs
atmospheric pressure (Patm)
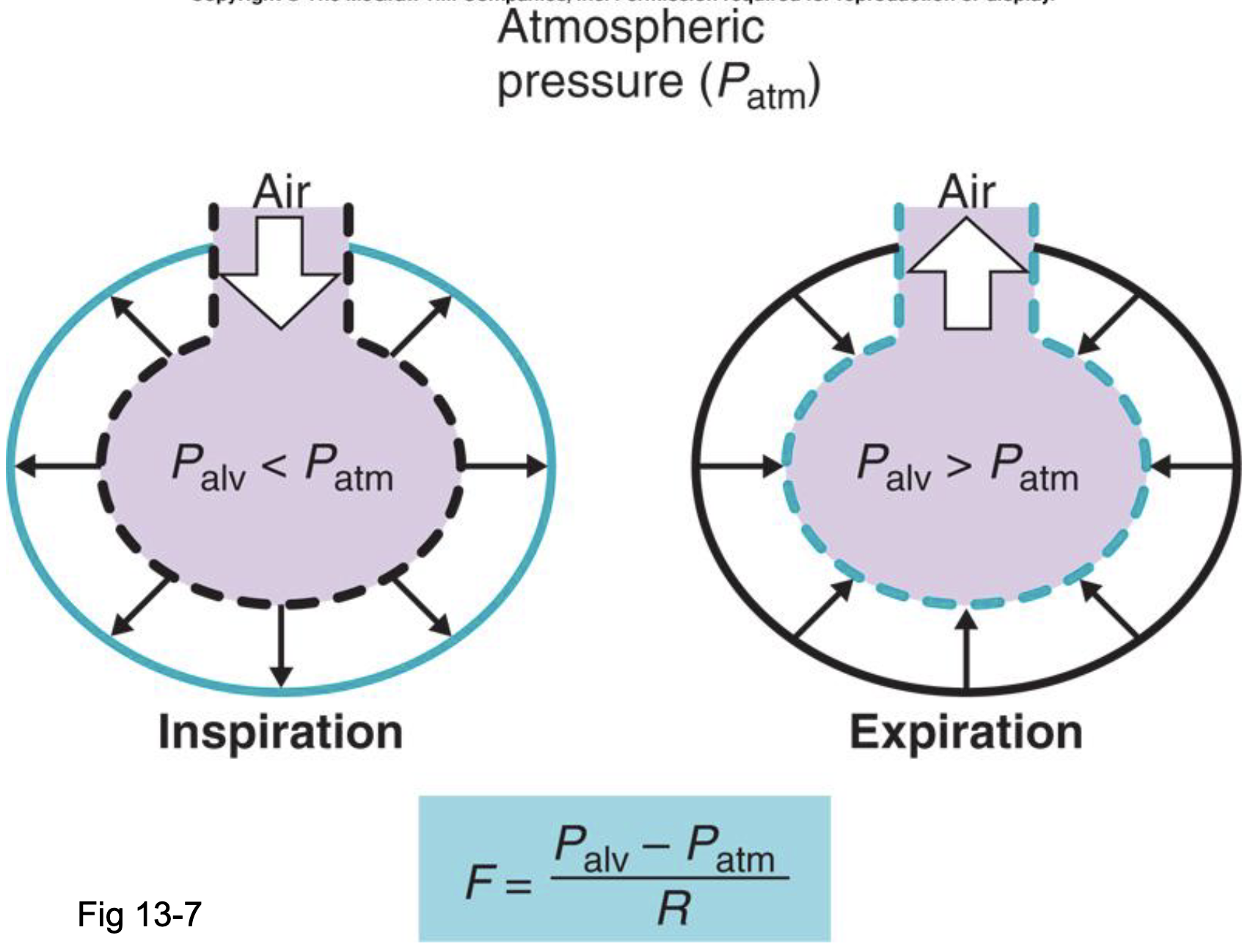
airway resistance
many of the same principles as vascular resistance
flow = change in pressure/resistance
most important influence on airway resistance is the size of the airways
asthma and COPD cause high airway resistance
why does emphysema increase compliance
emphysema destroys the lung matrix, the airways are very collapsable
especially with forced expiration, the airways flatten out such that air is hard to get through
lung diseases (two categories)
obstructive
something is obstructing the airflow
characterized by high airway resistance
restrictive
something is restricting chest expansion
characterized by low compliance
vital capacity
total amount of air that can be moved in and out of the lungs
3.5 to 4.5 L is an estimated value depending on a persons height
reduced with any kind of pulmonary disease
the size of vital capacity is an indication of a persons pulmonary health
FEV1/FVC
measure airway resistance
volume of forced expiration in one sec (FEV1) divided by forced vital capacity (FVC)
3 liters/4 liters = 75%
70-80% is normal
decreased with obstructive disease like asthma or COPD
disease - restrictive (R)
low compliance or stiff lungs
small tidal volume with high RR
fibrosis, tuberculosis, interstitial lung disease, ARDS, pulmonary edema
disease - obstructive (O)
high airway resistance
must be taught to breath slowly and quietly (pursed lip breathing)
asthma, emphysema, chronic bronchitis
commonalities between restrictive and obstructive
both have reduced vital capacity
R - difficulty expanding to get air in
O - difficulty recoiling to get the air out
both would have a reduced flow rate
both would have an increased work of breathing (WOB)
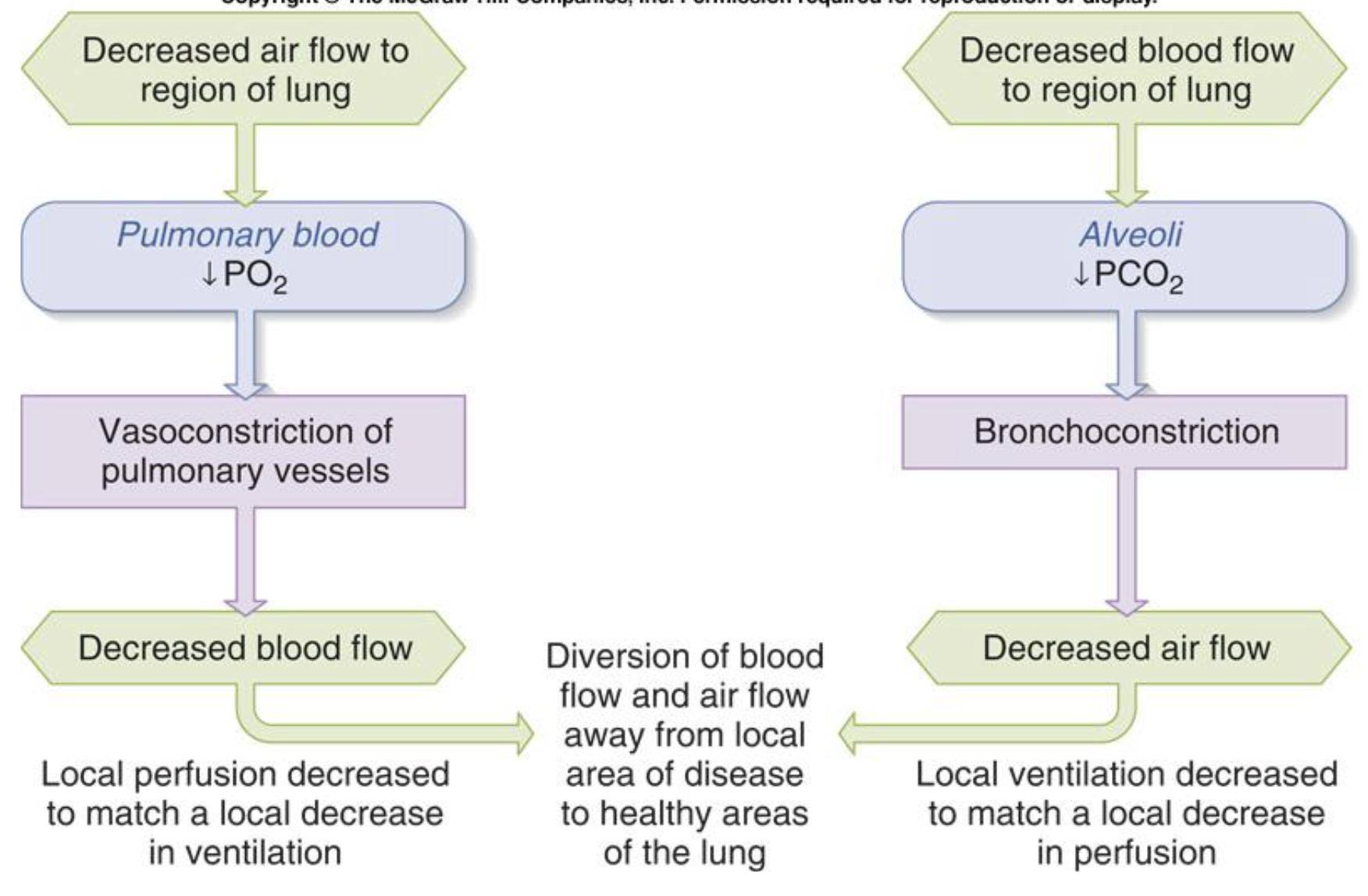
local control of blood flow
exercise dilates arterioles
arterioles get warmer, exposed to metabolic processes, exposed to more CO2 (local control)
this sends more blood flow
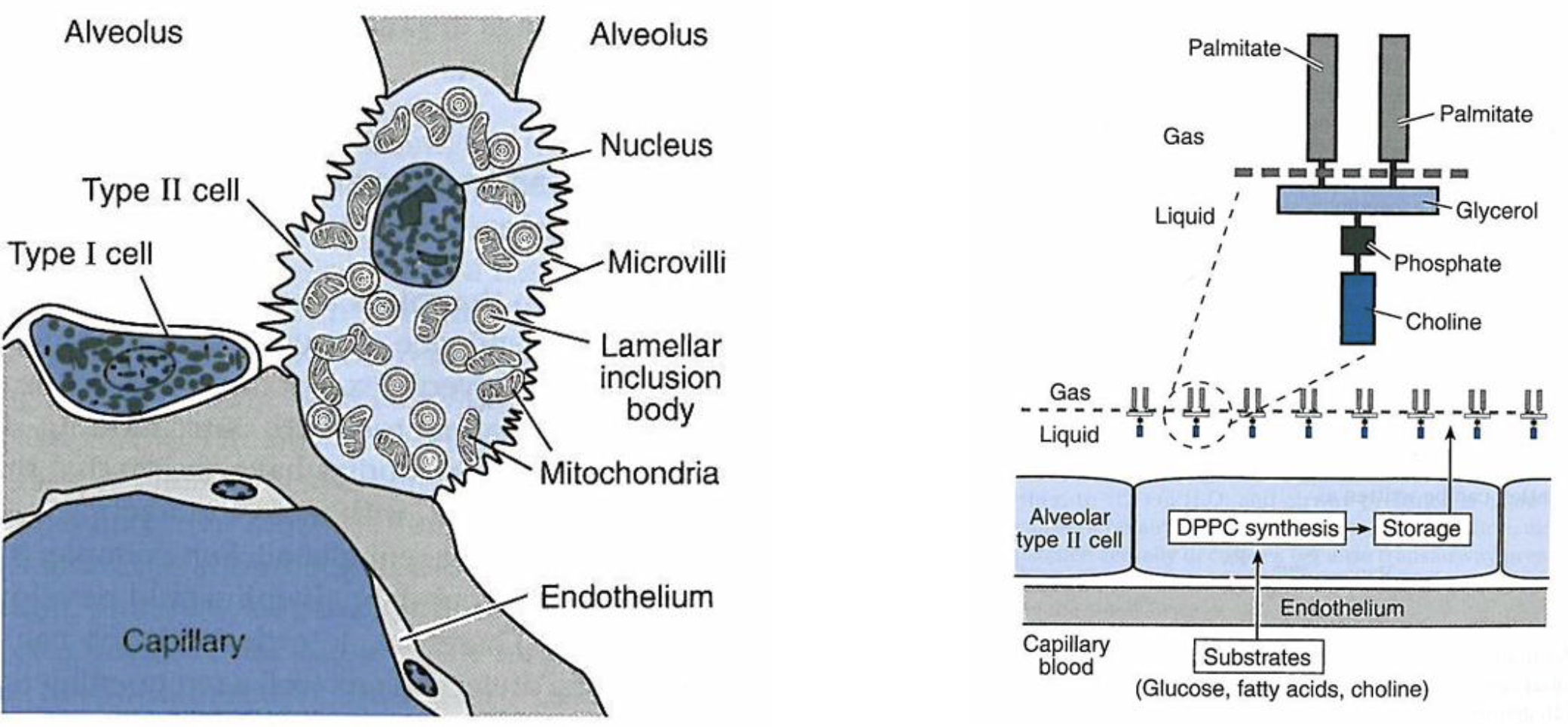
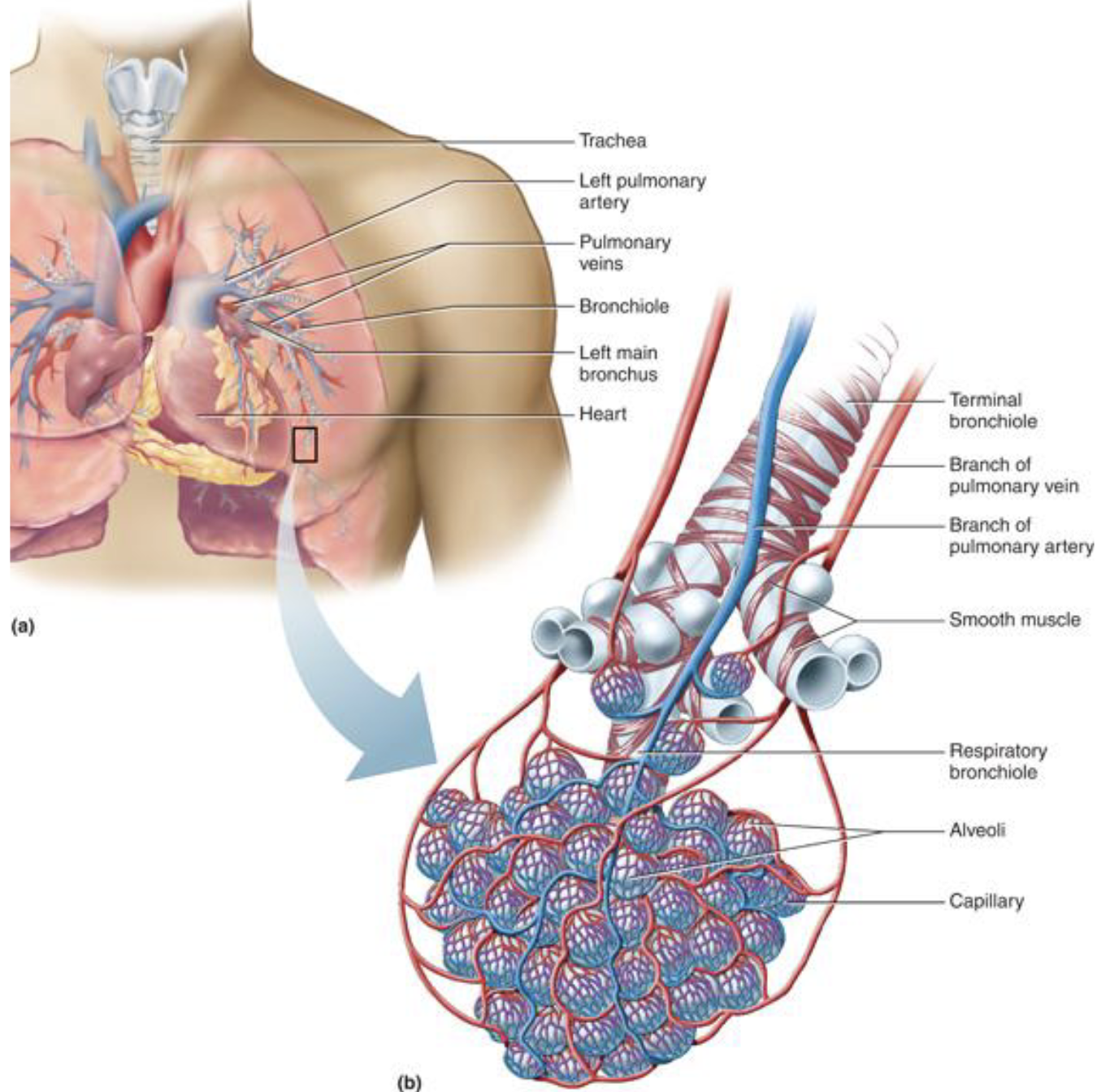
capillaries are dense in alveoli
hypoxic vasodilation
local responses in the lung are different
low oxygen in the airways cause the blood vessels going to that part of the lung to constrict
hypoxia in the lungs constricts arterials
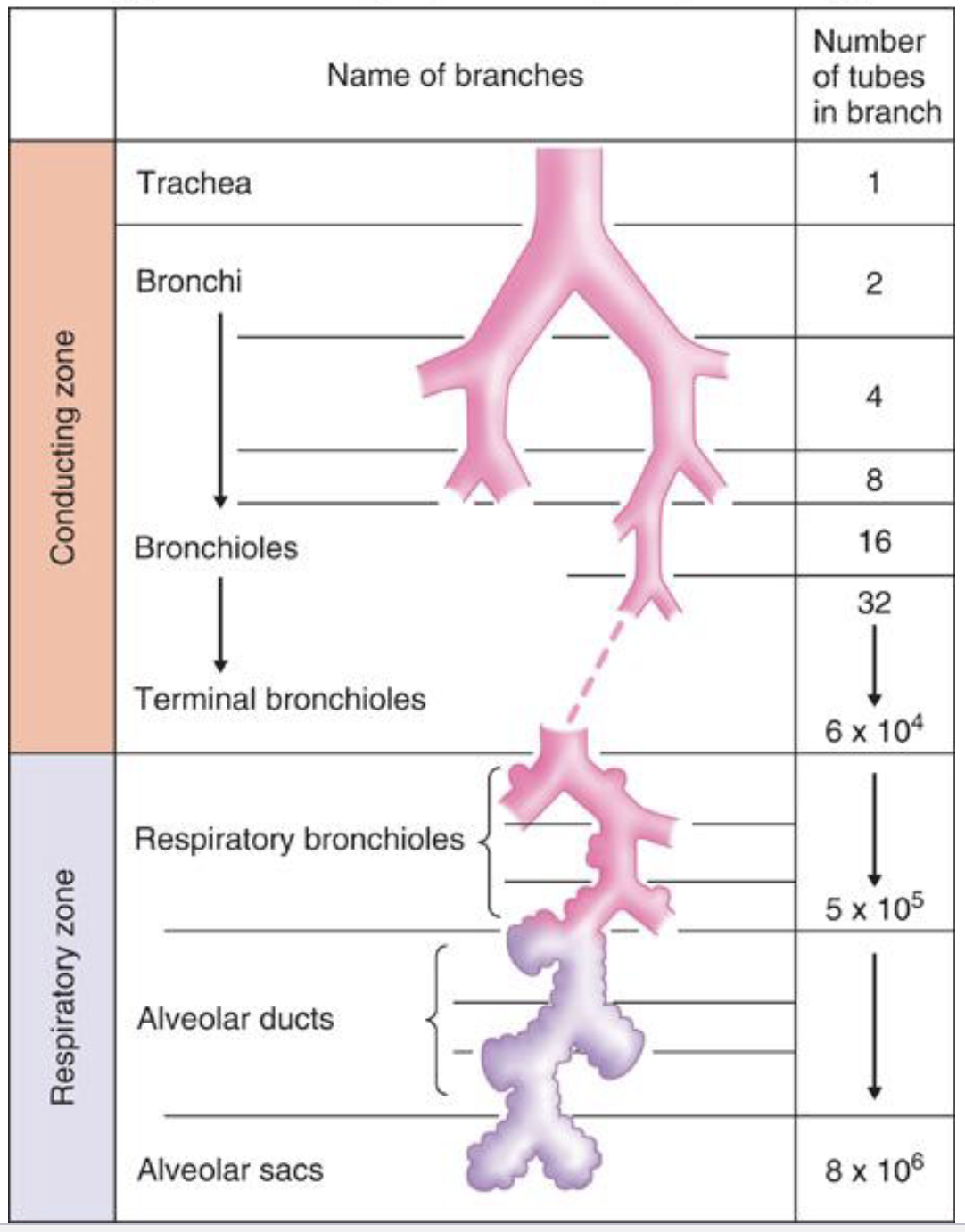
branching
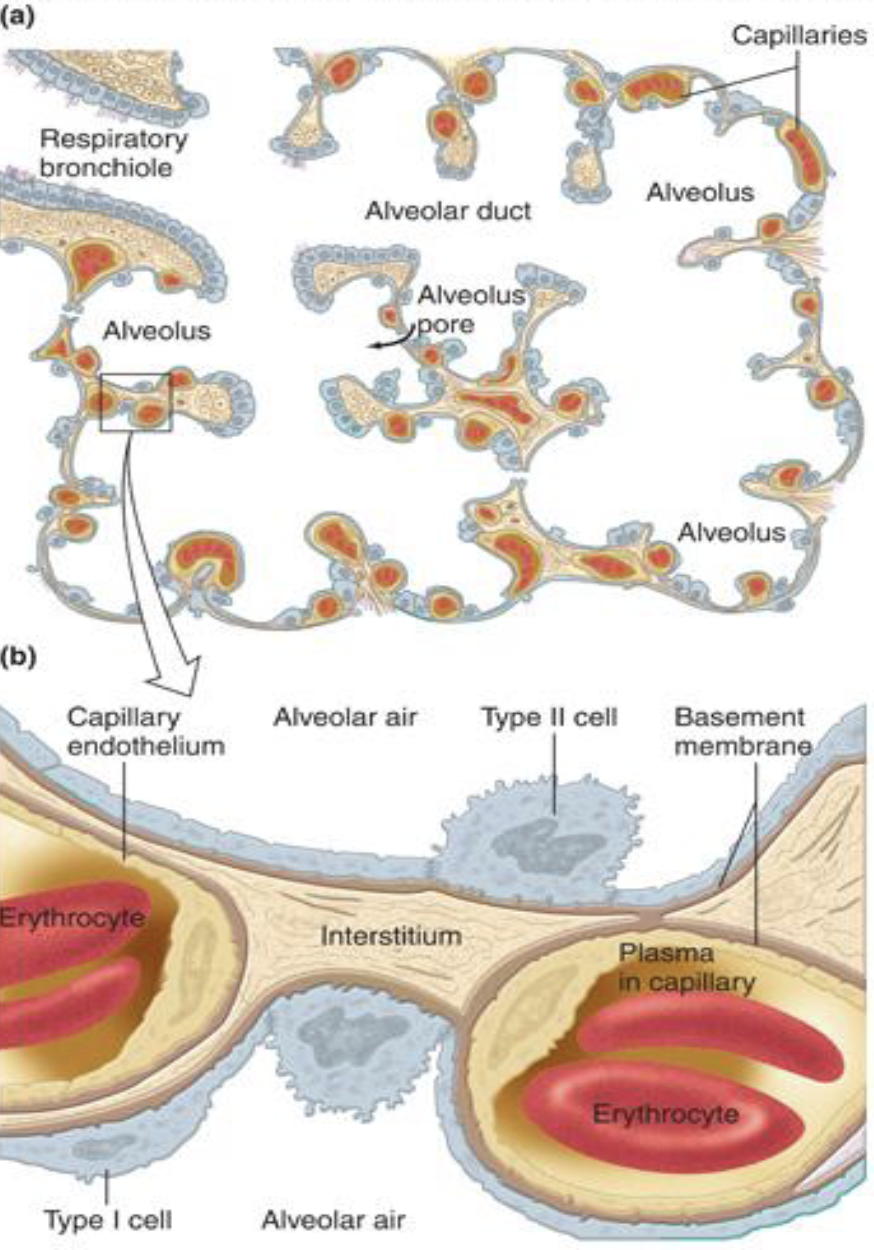
layers of diffusion membrane
alveolar type 1 cell
epithelial basement membrane
interstitial space
endothelial basement membrane
endothelial cell
RBC and hemoglobin binding
diffusion is influenced by
temperature - incoming air is warmed to body temp
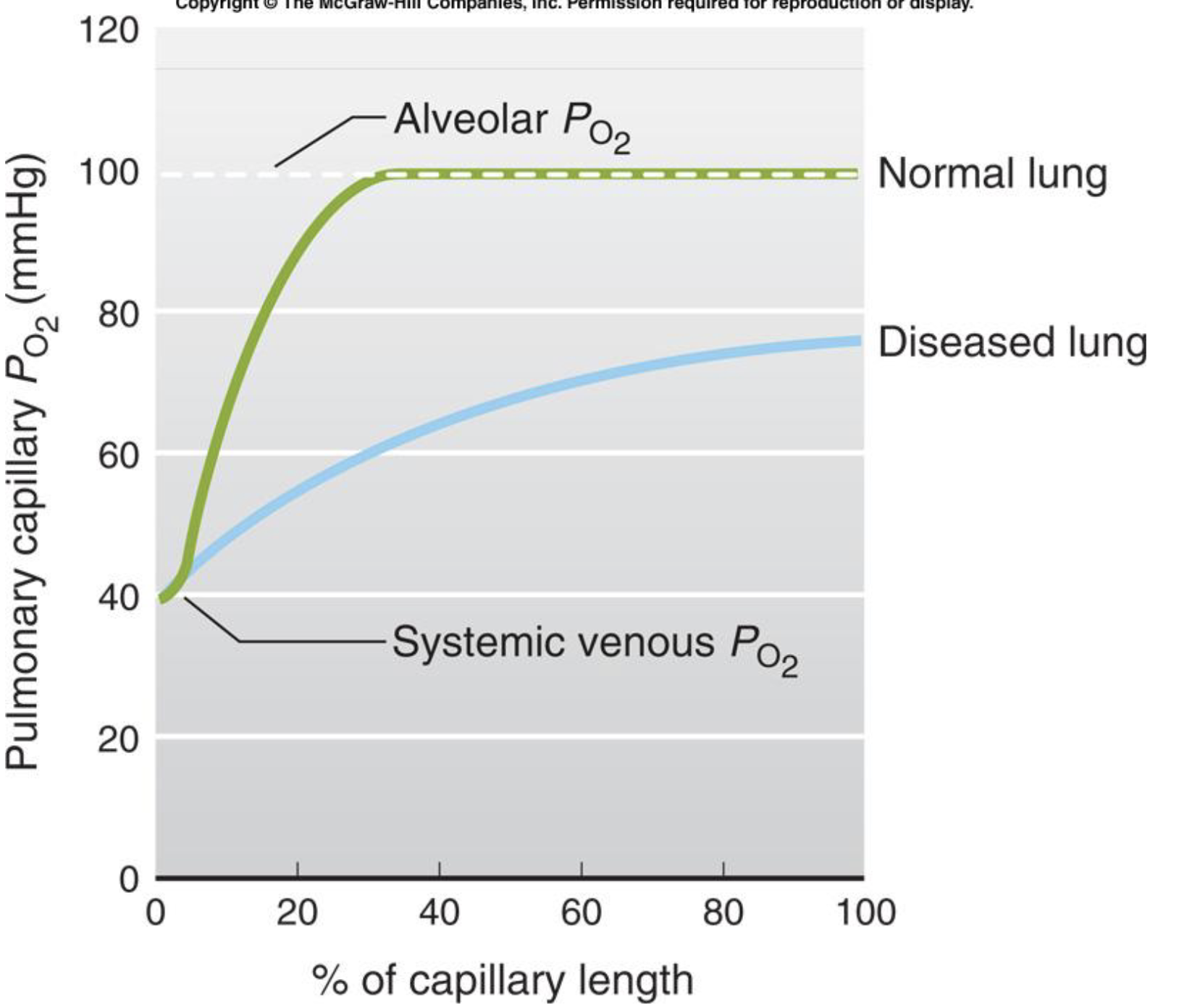
distance - barrier is very thin
surface area - alveolar system increases surface area
gradients - large stable gradients (FRC is about 3L - alveolar gas concentrations are fairly stable)
*human lungs are adapted and structured for diffusion
how do we measure concentration in the pulmonary system
partial pressure in mmHg
atmospheric pressure X fractional concentration of a gas
ex. at sea level, the atmospheric pressure is 760mmHg, and the air is 20% O2
760mmHg x 0.20 = 160mmHg is the PO2 in the atmosphere
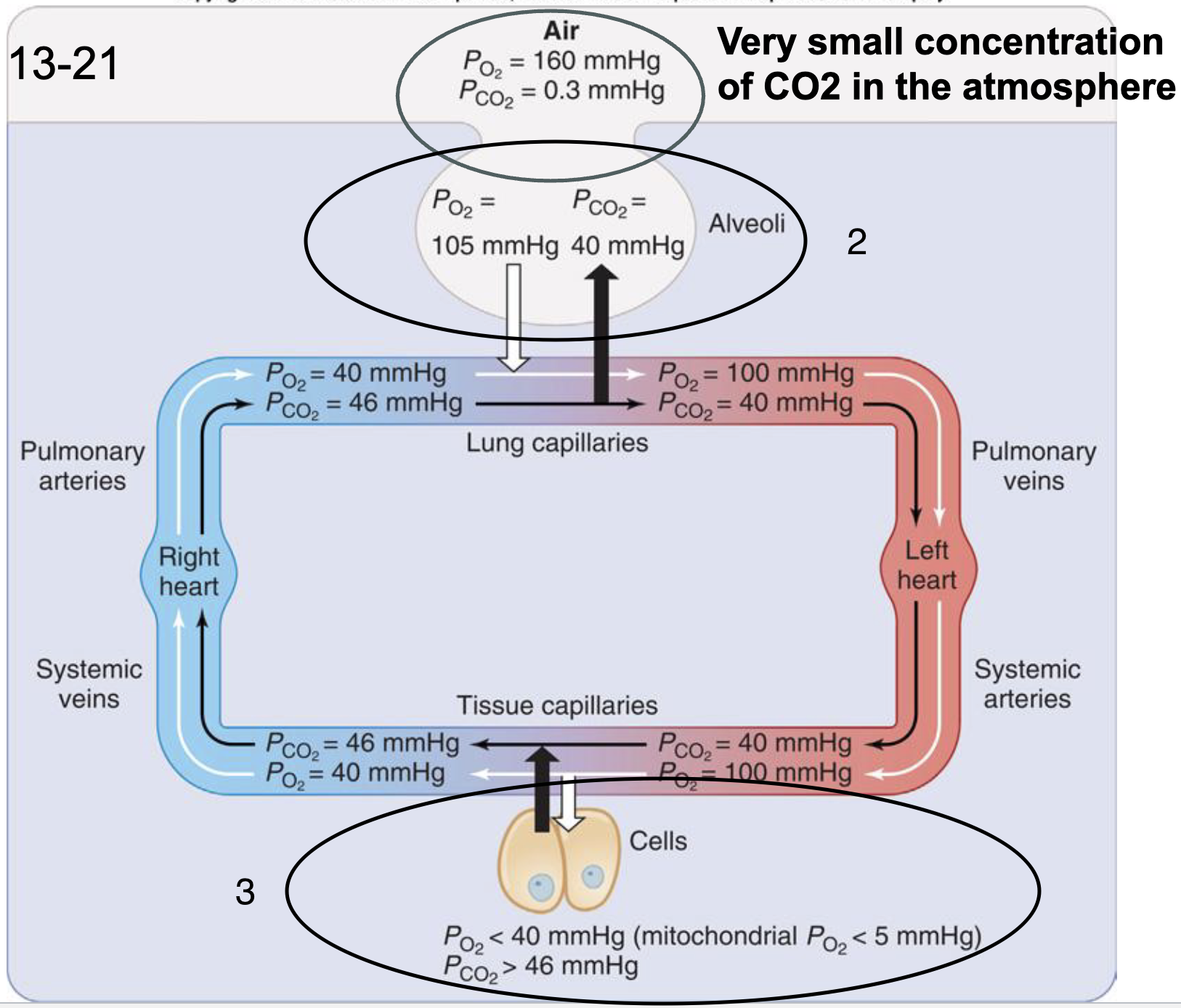
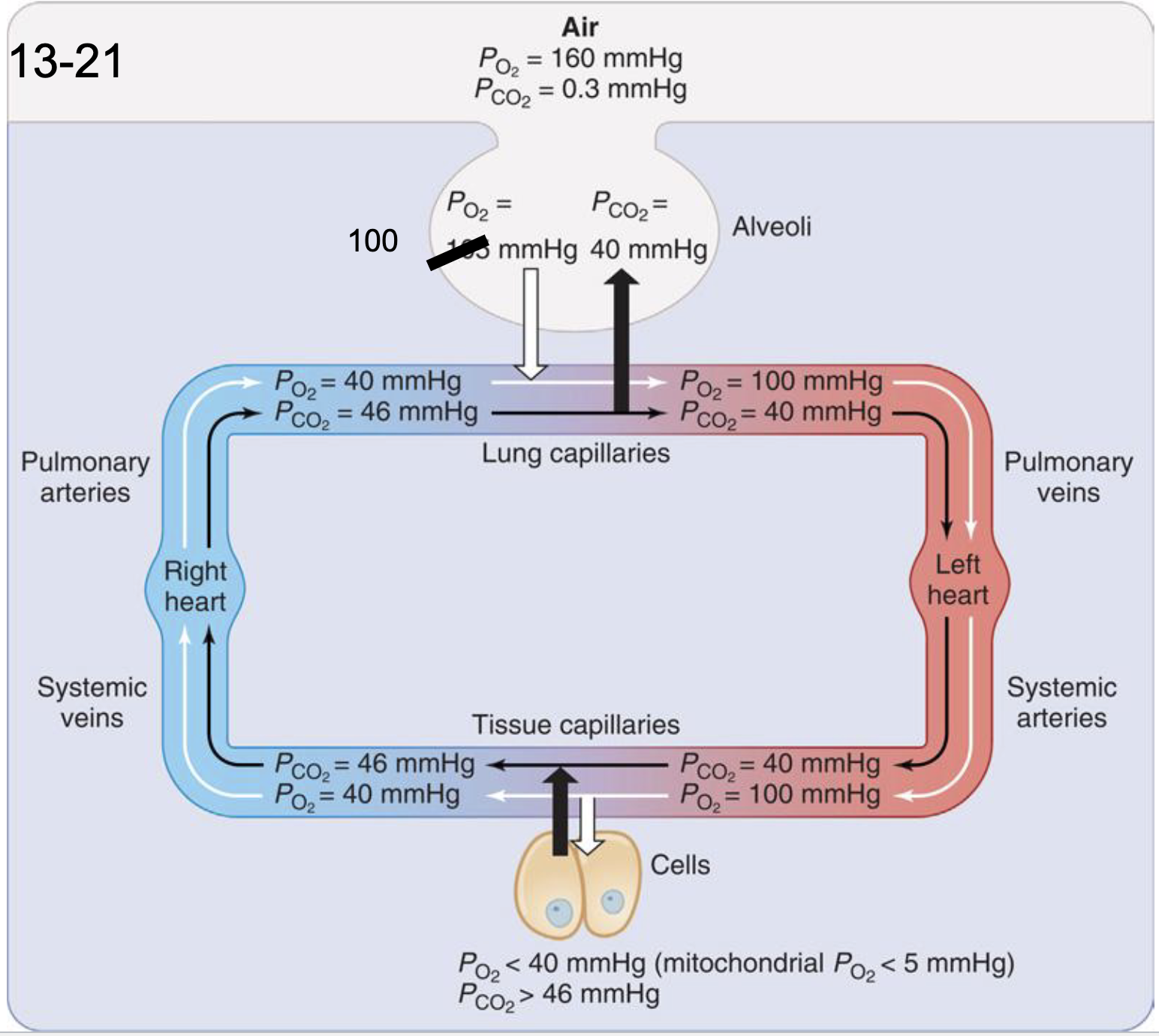
partial pressure diffusion gradients
very small concentration of CO2 in the atmosphere
tidal volume mixes with the air already in the lungs (CO2 comes from you!!!)
at the cells, O2 is consumed, and CO2 is produced PO2 must be at least 3 mmHg to make ATP (less than 5 mmHg)
alveolar gases
in the mitochondria, PO2 must be at least 3 mmHg to make ATP via oxidative phosphorylation
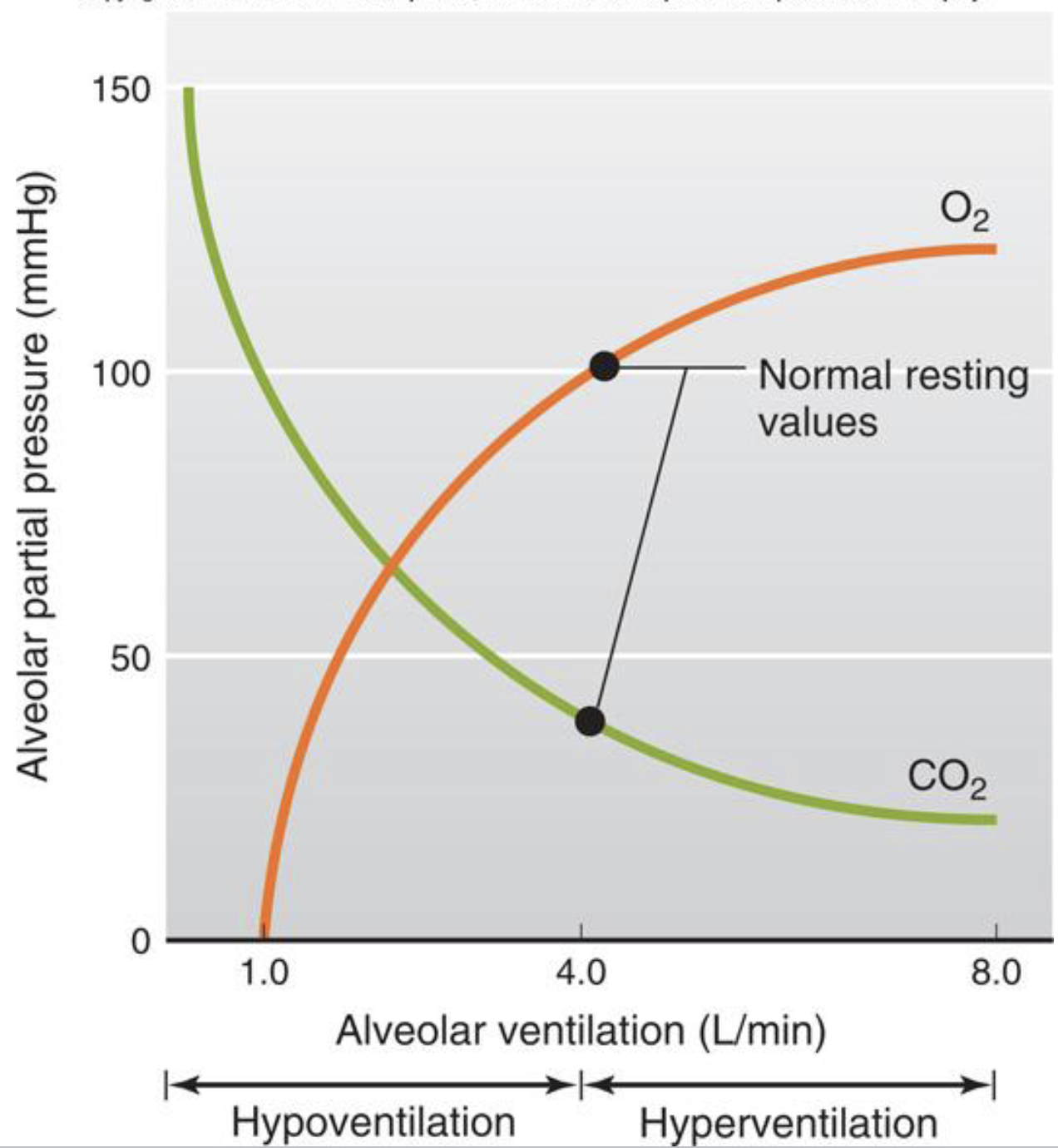
changes in ventilation change the partial pressure of oxygen and carbon dioxide in the alveoli
hyperventilation
hyperventilation is an alveolar ventilation that is higher than required for metabolism *hyperventilation is not a pattern of breathing
PO2 increases above 100mmHg
PCO2 decreases below 40mmHg
PCO2 is linked to pH
hyperventilation causes alkalosis (pH over 7.4)
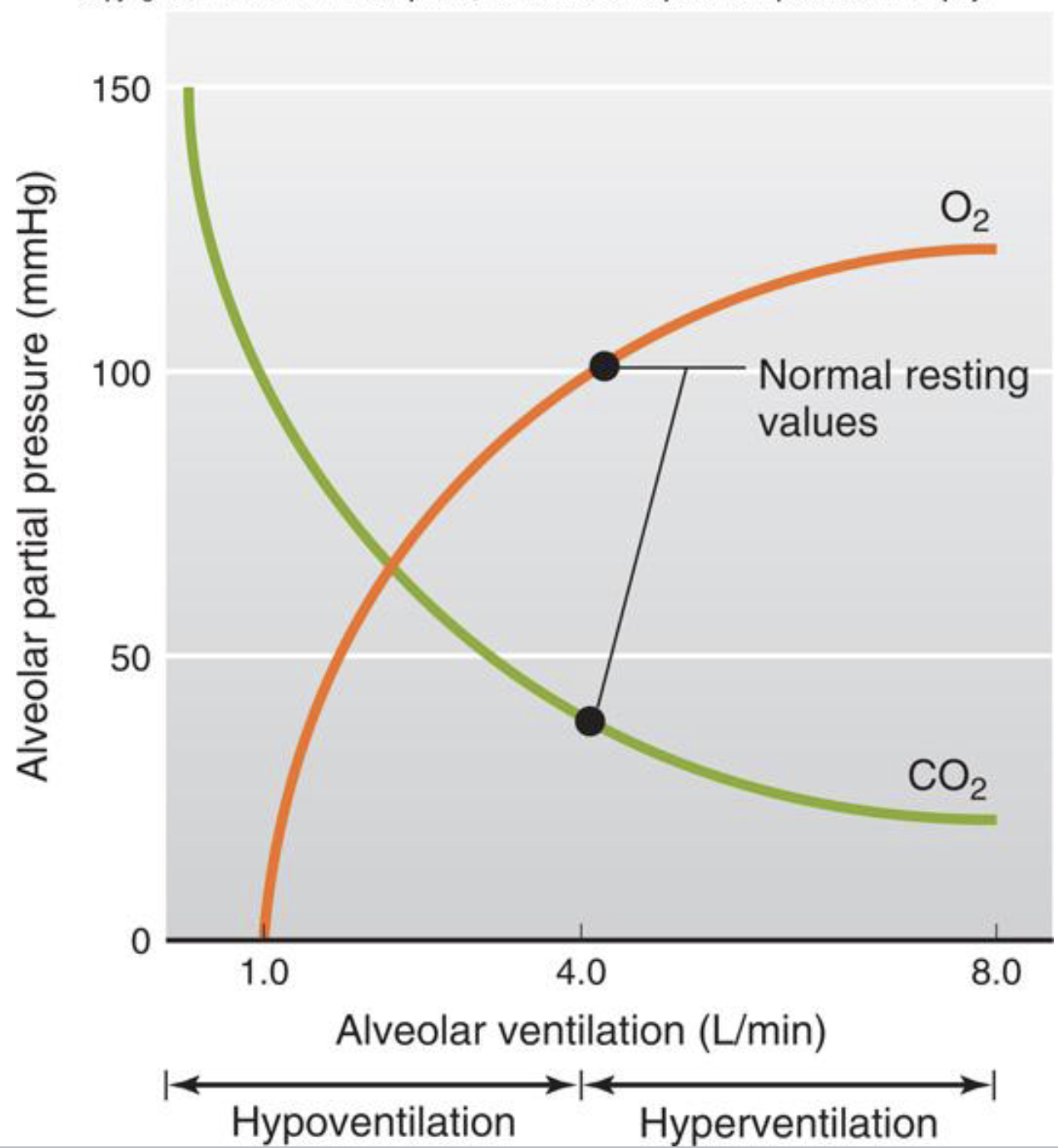
hypoventilation
hypoventilation is an alveolar ventilation that is less than required for metabolism
PO2 decreases
PCO2 increases
CO2 is linked to pH
hypoventilation causes acidosis (pH under 7.4)
why might a person hypoventilate
head injury, lung disease, COVID, drug overdose
if hypoventilation decreases PO2 in the alveoli, what happens to the diffusion gradient for O2 across the alveolar barrier?
the diffusion gradient will decrease
lowers partial pressure of oxygen (PO2)
how do we transport O2 and CO2 in the blood?
we transport most of the oxygen bound to hemoglobin
we convert most of the CO2 into bicarbonate
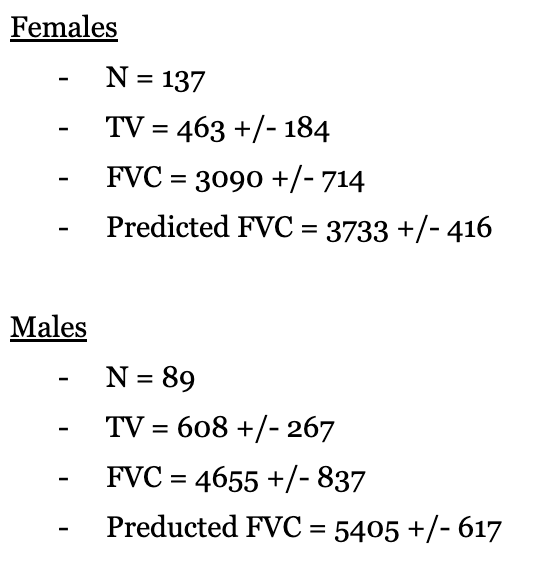
lung volumes in mL (spring 2012)
O2 diffusion gradients
What are the gradients that permit O2 to diffuse into the blood from the alveoli?
PAO2 = 100 mmHg > PvO2 = 40 mmHg
What are the gradients that permit O2 to diffusion from the blood to the tissues?
PaO2 = 100 mmHg > Pmito 3 mmHg
O2 transport
blood is 1/3 of the way through the capillary when it is fully loaded with O2
how is oxygen carried in blood?
dissolved content
bound content (to hemoglobin)
*hemoglobin bound content is more important
bound content
hemoglobin molecule can bind 4 molecules of oxygen
relies on iron
when oxygen binds to hemoglobin it is not oxygen anymore!!!
PP ends equal again
this is what happens in capillaries
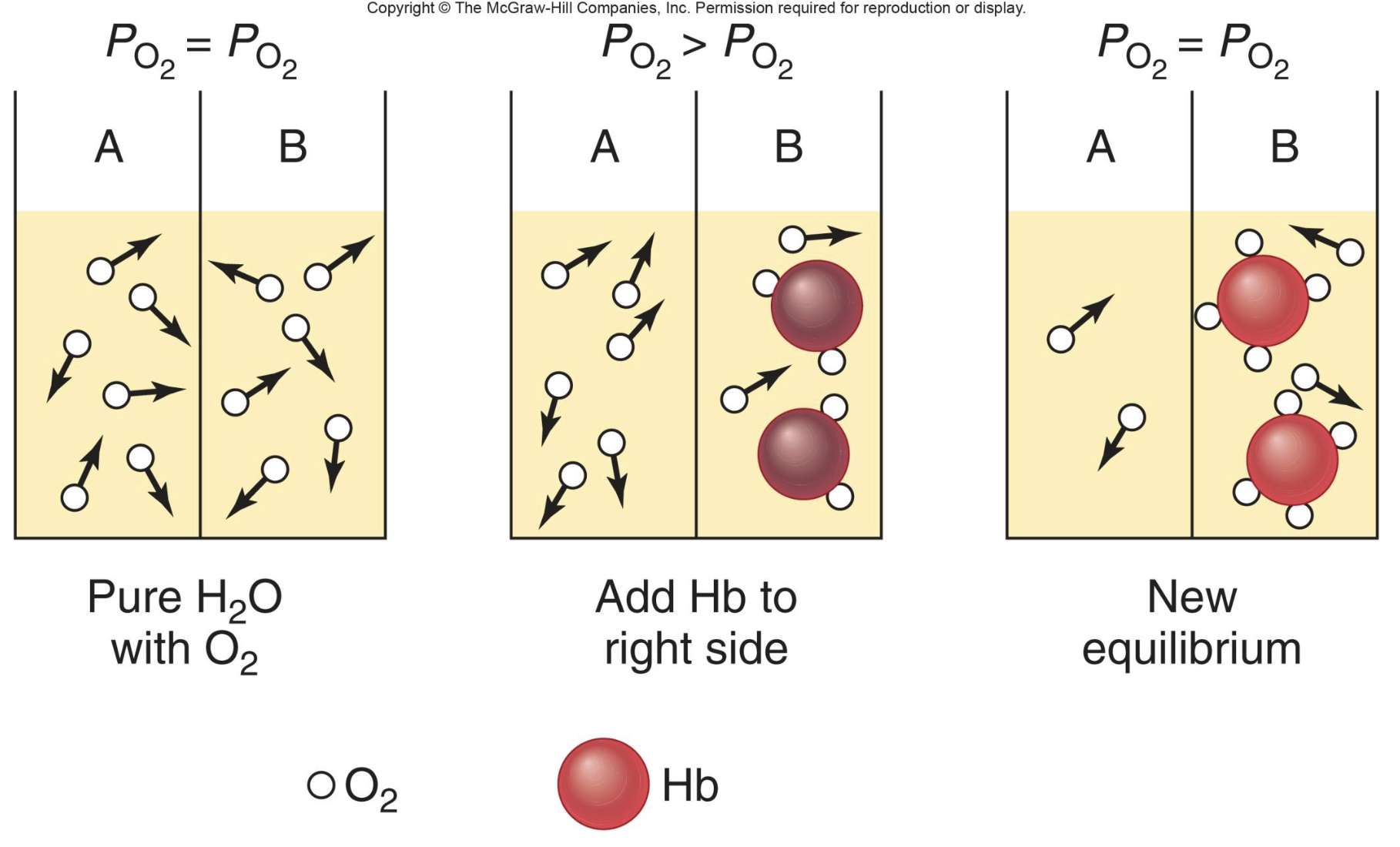
how does O2 diffuse?
O2 diffuses from alveoli into the plasma, binds to hemoglobin, oxygen is no longer oxygen
saturation and coopertivity
saturation is a percent
cooperativity - when a molecule behaves in a cooperative way
when oxygen binds, the easier it is for other oxygen to bind
when oxygen lets go, the easier it is for other oxygen to release
when PO2 is high it favors binding
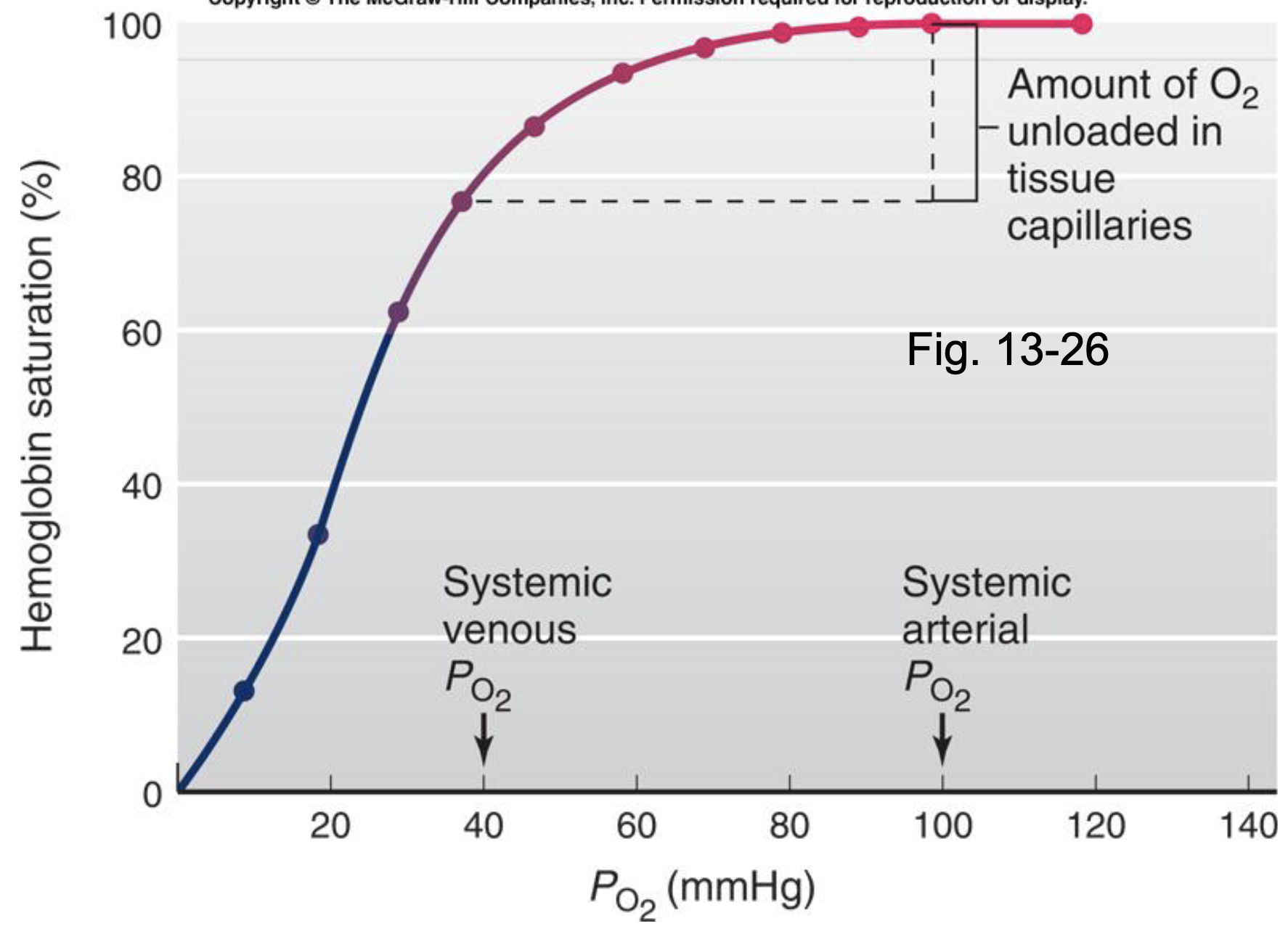
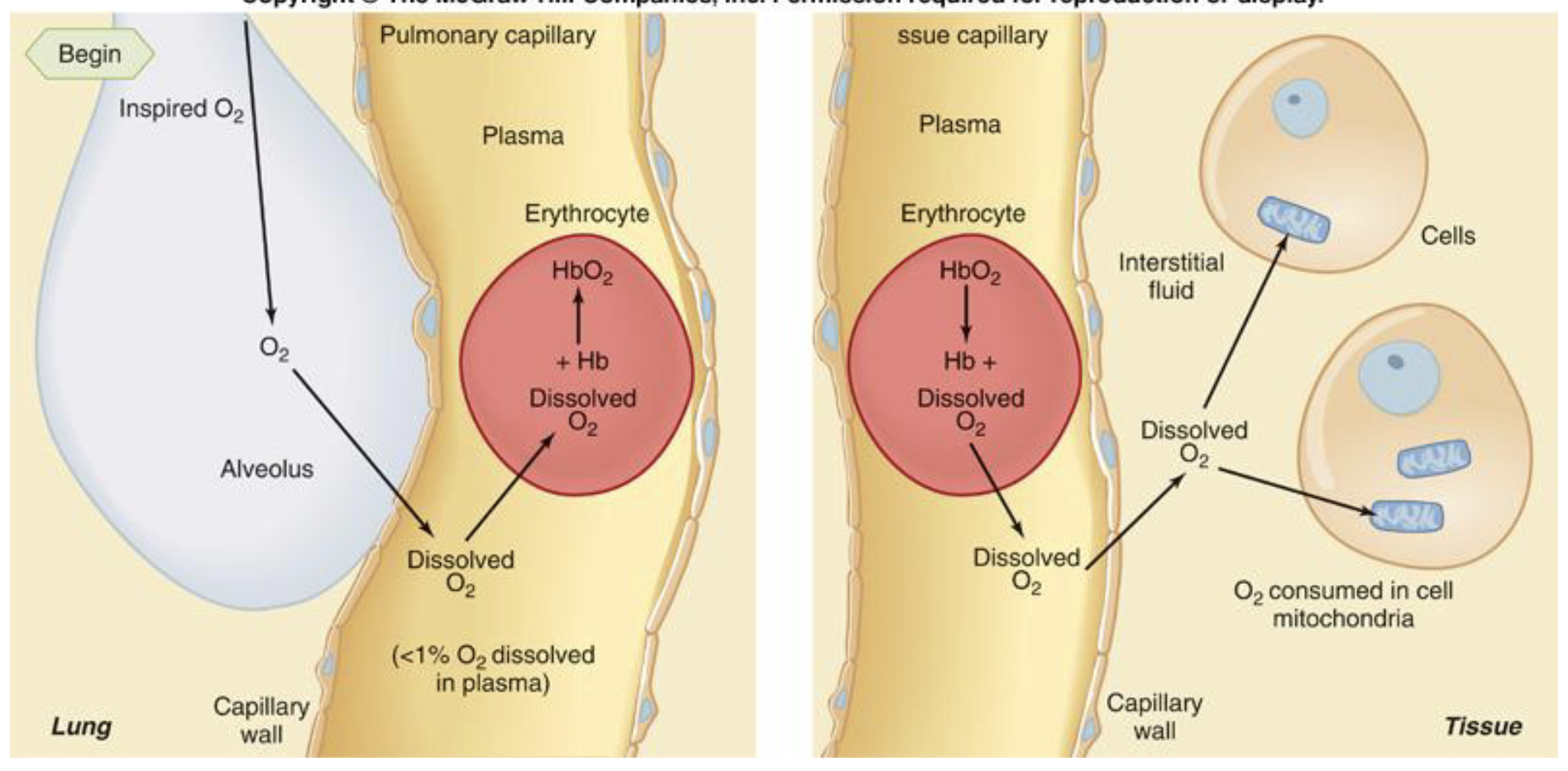
he dissolved oxygen is exerting PO2; the oxygen has to dissolve and diffuse into the RBC before it can bind to hemoglobin
at the tissues, the oxygen has to unbind, dissolve and diffuse into the tissue cell so it can participate in oxidative phosphorylation in the mitochondria
content and saturation
mary has a 12 gm% of hemoglobin and frank has 13 gm%
at PO2 of 100 mmHg of mercury
who is more saturated?
equal - their PO2 is equal, so their saturation is equal
who has higher dissolved content?
equal - their PO2 is equal, so their dissolved content is qual
who has a higher bound content?
frank - he has more hemoglobin and spots to bind
saturation and content review
saturation is a percentage
depends on PO2 alone
independent of the hemoglobin concentration
content is an amount
mL O2/100 mL blood
depends on both PO2 and hemoglobin concentration
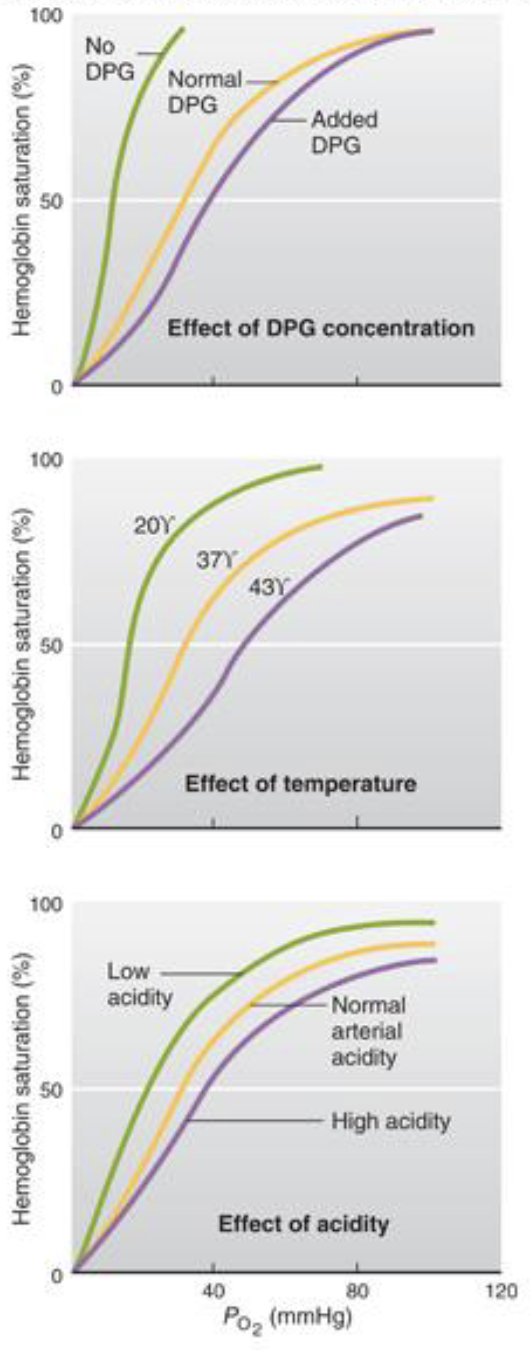
bohr effect (right shift)
right shift (release)
high temp, CO2, H+
promotes O2 release
*50% saturation is farther because oxygen is being released more rapidly
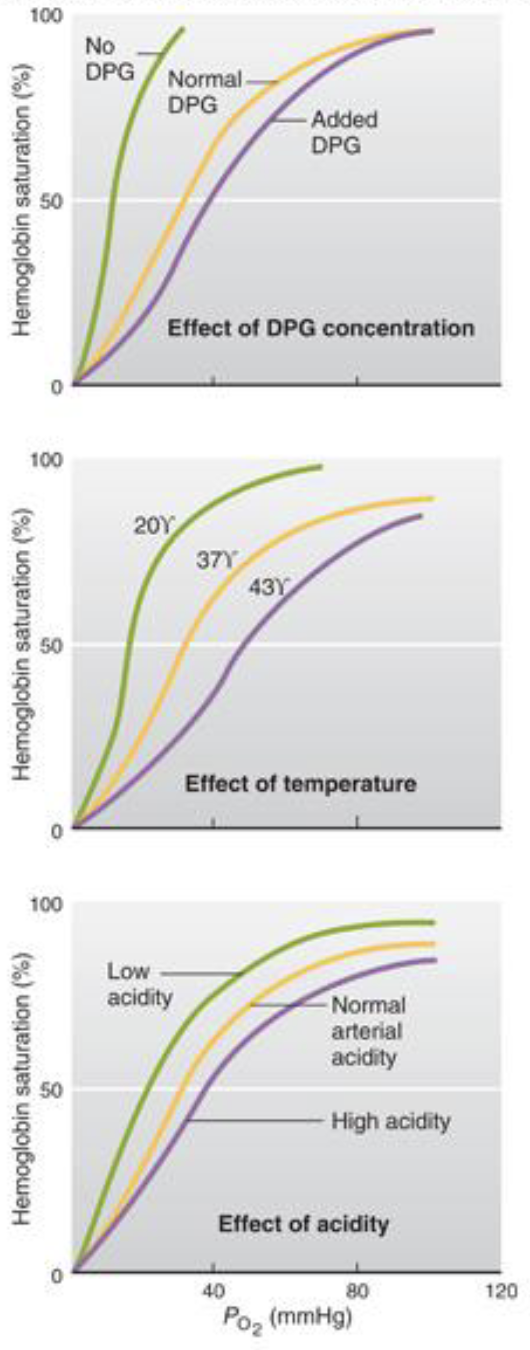
bohr effect (left shift)
left shift (latch)
low temp, CO2, H+
promotes O2 binding
carbon monoxide
240 times the affinity for hemoglobin than oxygen
decreases content with normal PO2 and PCO2
NO SHORTNESS OF BREATH
left shift
carbon monoxide hogs binding sites and prevents oxygen from releasing - causes left shift
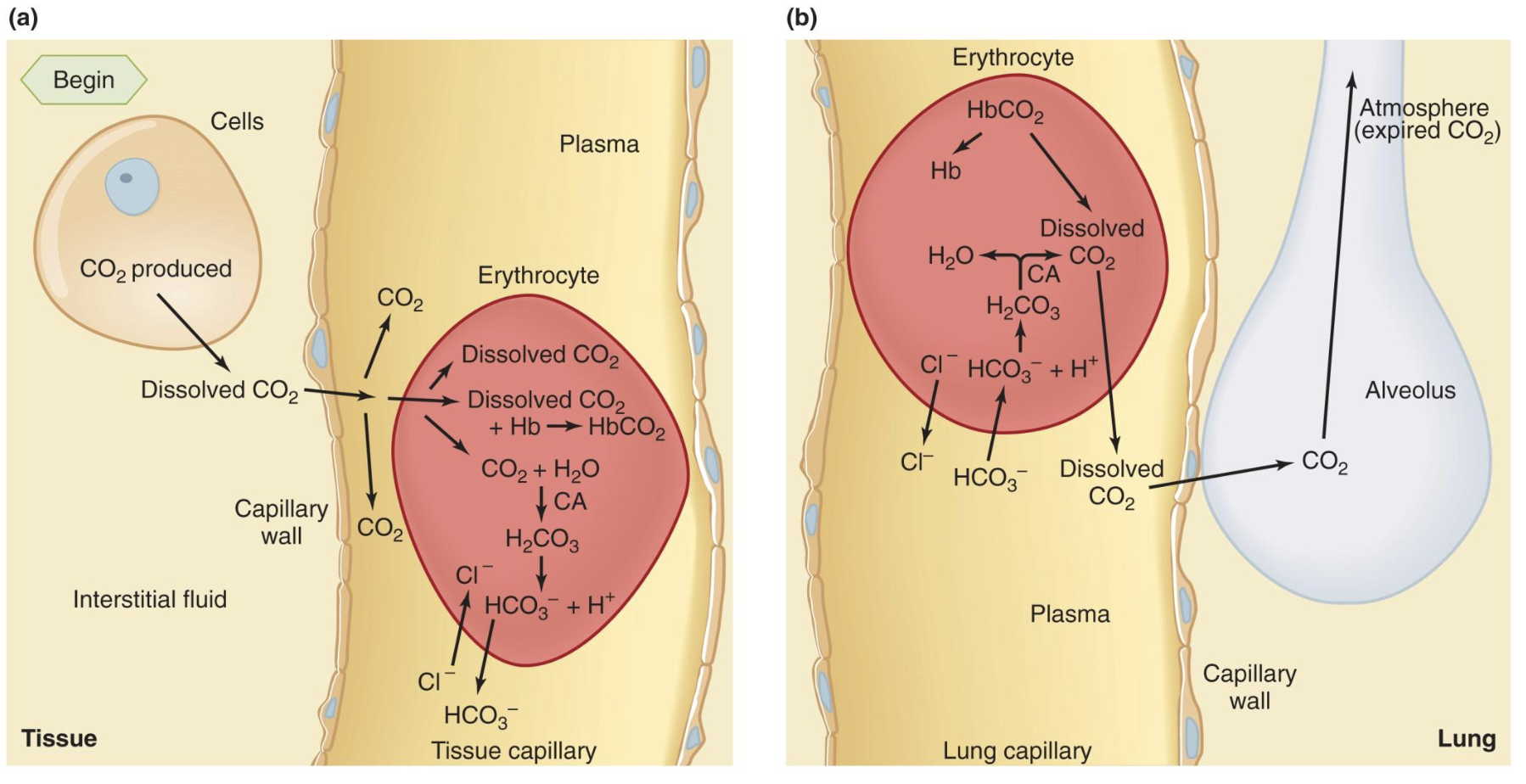
carbon dioxide transport
some dissolves in blood
some binds to hemoglobin
MOST is converted to HCO3-
CO2 + H2O → H2CO3 → H+ + HCO3-
*a build up of CO2 causes a build up of acid
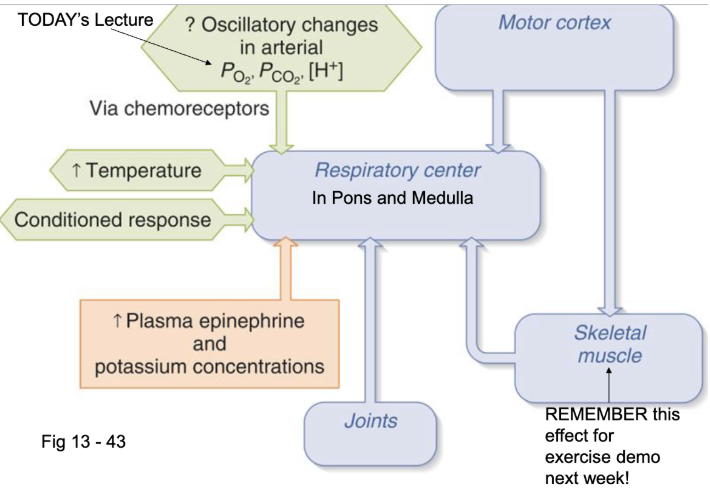
pacemakers of respiration
the pacemakers that drive the system of breathing are in the brain
respiratory centers are in the medulla; some areas in the pons regulate centers in the medulla
CO2 + H20 → Carbonic Anhydrase → HCO3- + H+
*the hydrogen ion stimulates the chemo receptors
receptors
central receptors and peripheral receptors
all regulate arterial blood
are in aortic arch and internal carotids
include baroreceptors and ???
central receptors
respond to and monitor CSF H+ from arterial PCO2
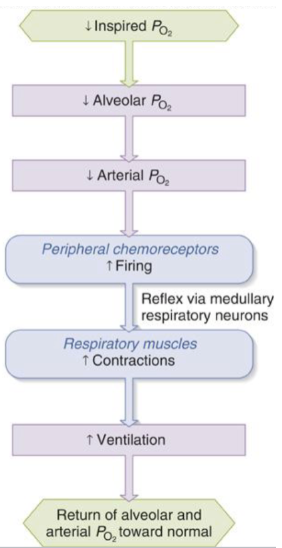
peripheral receptors
respond to CO2, H+, and O2
innervated by afferent
oxygen response is ONLY at the peripheral chemo receptors
low oxygen stimulates ventilation at…
PO2 levels of 60mmHg or below
*small changes in oxygen wont change breathing, need dramatic drop to cause change
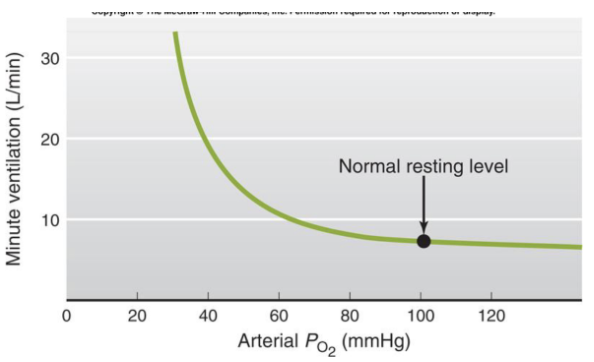
arterial PO2 less than 60mmHg
signals sent to brainstem/medullan - ecourages muscles to contract - encourages contraction - PO2 goes up
*a person in this condition may not feel short of breath (SOB) if both O2 and CO2 were low
most important regulator of ventilation
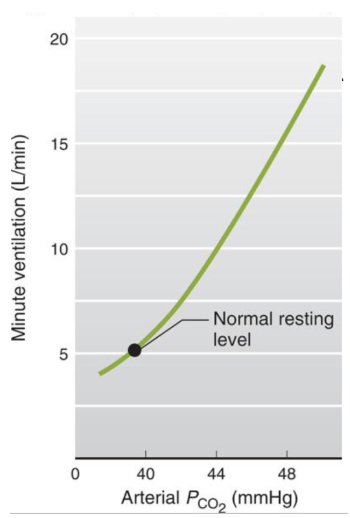
arterial PCO2 is the MOST important regulator of ventilation especially at rest
normal arterial PCO2 is about 40 mmHg, minute arterial ventilation is 5 L/min
PCO2 is tightly regulated, small changes in PCO2 causes big changes in minute ventilation
PCO2 is intimately related to pH - maintain PCO2 = regulating pH
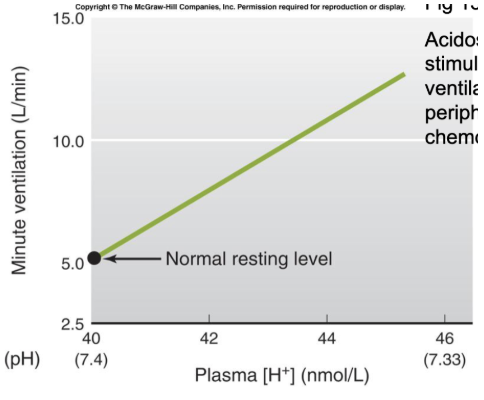
acidosis
acidosis stimulates ventilation at peripheral chemoreceptors
acidosis can be unrelated to breathing (ex. diabetes)
pH should be 7.4
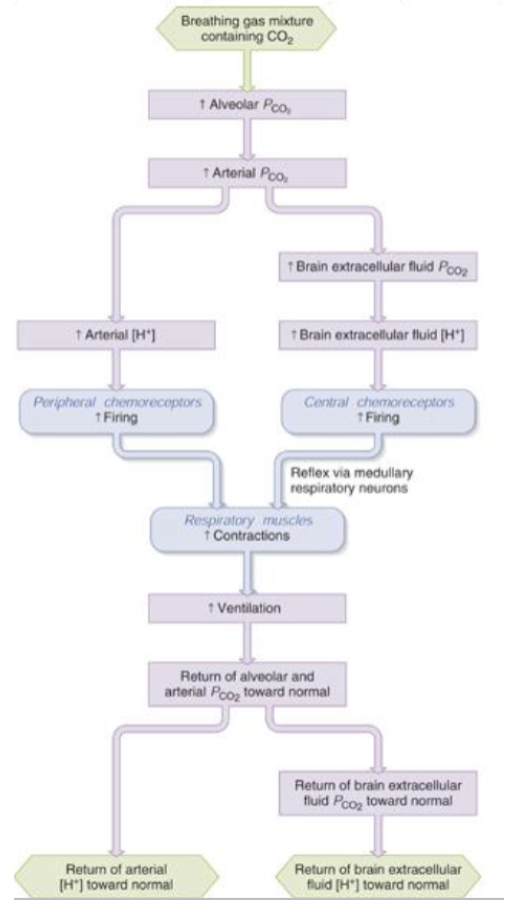
arterial PCO2 is major stimulus of ventilation
stimulates BOTH central and peripheral chemoreeptors
CO2 can be converted to H+ in blood and peripheral chemoreceptors. CO2 can cross blood brain barrier and be converted to H+ in CSF
PCO2 levels have an important impact on dyspnea (shortness of breath)
how do pacemakers and regulators in pons/medulla regulate how fast we breath
decrease in PO2, increase in PCO2, increase in H+ increases breathing
increased temperature increases breathing
increased epinephrine and plasma increases breathing
we can control increase breathing in motor cortex
joint receptors anticipate increased breathing (feedfoward control)