Blood Flashcards (my version)
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Functions of blood:
Transports: O2, CO2, Nutrients, hormones, wastes
Regulates: Body temp, pH in body tissues, fluid volume (ex: salts)
protection: protects against blood lost and disease
What is the pH of blood
7.35-7.45
Composition of blood:
is denser that H2O
temp: 100.4 F (38 C)
constitutes 8% of body wright and 4-5 liters in avg adult
What is normal body temp and what structure regulates it?
37C (98.6F), hypothalamus
Composition of blood—Plasma components:
90% H2O with dissolved compounds
is 55% of whole blood
least dense component
has proteins: albumin, antibodies, clotting proteins
their function: maintain osmotic pressure
electrolytes: Na, K, Ca, Mg, Cl, bicarbonate
What are the formed elements
RBCs, Leukocytes, Platelets
(45% of whole blood)
only WBCs are complete cells (RBC have no nuclei/other organs, platelets=cell fragments)
most formed elements survive in blood stream for a few days
most blood cells originate in red bone marrow and don’t divide
What is hematocrit
% of blood volume that is RBCs
normal values:
men: 40-54%
women: 36-48%
Where are WBCs and platelets located
buffy coat (<1%)
is a thin whiteish layer btw RBCs and plasma layer
Components of Plasma- Albumin
60% of plasma proteins
transports substances (bilirubin, bile salts, T4/T3
Components of plasma—globulins
α (alpha), β (beta) transport hormones, cholesterol and iron
gamma globulins= antibodies (immunoglobulins)
Components of plasma—fibrinogen
precursor for the clotting protein fibrin
How many microliters are there of RBCs (erythrocytes)
4.8-5.4 million/μL
How many microliters are there of WBCs (leukocytes)
4500-11000μL
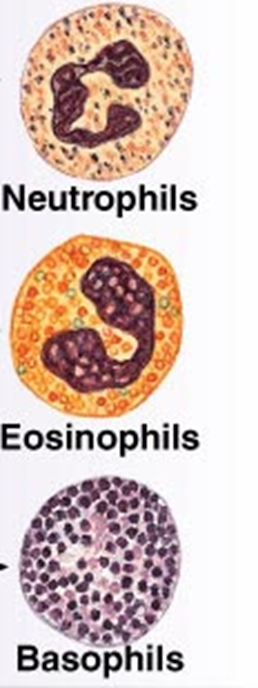
What are the granulocytes and their percentages of WBCs
neutrophils 60-70% of WBCs
eosinophils: 2-4% of WBCs
Basophils: 0.5-1%
What are the agranulocytes and their percentages of WBCs
lymphocytes: 20-25% of WBCs (contains T and B lymphocytes and natural killer cells)
monocytes 3-8%
How many microliters are there for platelets
150,000–400,000/ μL (microliter)
erythrocytes facts:
biconcave shape
no nucli/organelles
lasts 120 days and is then destroyed by spleen or liver
What are the enzymes in the cytoplasm of RBCs
glycolytic enzymes to carry out glycolysis
carbonic anhydrase—converts CO2 to HCO3
What 3 features make efficient gas transportation for RBCs
their biconcave shape—offers huge surface area relative to volume for gas exchange
hemoglobin makes up 97% cell volume (not accounting H2O)
RBCs have no mitochondria
ATP production is anaerobic, they don’t consume the O2 they trasnport
why are red blood cells red
Hemoglobin is made of two main parts: the "heme" group and the "globin" group. The heme group contains iron which gives the red color to the red blood cell. The globin group is a protein that helps the red blood cell carry and hold oxygen in place as it moves throughout the body.
what is the function of erythrocytes
transport oxygen (O2) and to a lesser extent carbon dioxide (CO2)
contains hemoglobin (Hb/Hgb)
each RBC contains 250 million Hb molecules
O2 loading in the lungs
produces oxyhemoglobin (ruby red)
O2 unloading in tissues
produces deoxyhemoglobin/reduced hemoglobin (dark red)
CO2 loading in tissues
20% of CO2 in blood binds to Hb, producing carbaminohemoglobin
what is hemoglobin made up of
4 globin polypeptide and 4 heme groups
a heme pigment is bonded to each globin chain
each heme’s central iron atom binds one O2
each Hb molecule can transport four O2
each RBC contains 250 million Hb molecules
What is erythropoiesis?
production of new RBCs (~3 million/sec)
occurs in red bone marrow
rate of production is controlled by erythropoietin (EPO) that is produced by the kidneys in response to blood oxygen levels
What is hematopoiesis
all blood cells arise from a common stem cell found in red bone marrow
what is the formation of erythropoiesis?
hemocytoblast—> reticulocyte ~15 days
reticulocyte—> matures in bloodstream ~2 days
is controlled by erythropoietin
What is the the consequences of using artificial EPO
the use of EPO increases hematocrit, allows athletes to increase stamina and performance
increases hematocrit from 45-65% w/ dehydration concentrating blood even more
blood becomes like sludge and can cause clotting, stroke or heart failure
What are the dietary requirements for erythropoiesis
amino acids, lipids, carbs
iron (available from diet)
vitamin b12 and folic acid
necessary for DNA synthesis for rapidly dividing cells (such as developing RBCs)
what is the fate and destruction of erythrocytes
life span: 100-120 days
RBCs are anucleate, cannot synthesize new proteins, grow or divide
old RBCs are fragile, Hb begins to degenerate
can get trapped in smaller circulatory channels, especially spleen
macrophages in spleen engulf and breakdown dying RBCs
What are 2 types of blood loss (erythrocyte disorders)
acute hemorrhagic anemia
rapid blood loss
chronic hemorrhagic anemia
slight but persistent blood loss
primary problem must be treated to stop blood loss
What is Iron-deficiency anemia
not enough RBCs being produced
Can be caused by hemorrhagic anemia, but also by low iron intake or impaired absorption
RBCs produced are called microcytes
Small, pale in color
Cannot synthesize hemoglobin because there is a lack of iron
Treatment: iron supplements
What is pernicious anemia
not enough RBCs being produced
Autoimmune disease that destroys stomach mucosa that produces intrinsic factor
Intrinsic factor needed to absorb B12
B12 is needed to help RBCs divide
Without B12 RBCs enlarge but cannot divide, resulting in large macrocytes
Treatment: B12 injections or nasal gel
What is renal anemia
cause: lack of EPO
often accompanies renal disease
kidneys can’t produce enough EPO
treatment: synthetic EPO
what is aplastic anemia
Destruction or inhibition of red bone marrow
Can be caused by drugs, chemicals, radiation, or viruses
Usually cause is unknown
All formed element cell lines are affected
Results in anemia as well as clotting and immunity defects
Treatment: short-term with transfusions, long-term with transplanted stem cells
what is sickle cell anemia
Hemoglobin S: mutated hemoglobin
Only 1 amino acid is wrong in a globin beta chain of 146 amino acids
RBCs become crescent shaped when O2 levels are low
Example: during exercise
Misshaped RBCs rupture easily and block small vessels
Results in poor O2 delivery and pain
what is polycythemia
Abnormal excess of RBCs; increases blood viscosity, causing sluggish blood flow
Polycythemia vera: Bone marrow cancer leading to excess RBCs
Hematocrit may go as high as 80%
Treatment: therapeutic phlebotomy
Secondary polycythemia: caused by low O2 levels (example: high altitude) or increased EPO production
What are leukocytes and their function
protects against infection and initiates inflammation
destroys cancerous cells
tissue repair
What are granulocytes and the 3 diff types of them
granulocytes- granule containing cells w/ lobed nuclei
neutrophils (60-70%)'
phagocytes
first on the scene of infection and triggers inflammation
eosinophils (1-4%)
associated with allergies and parasite infections
basophils (<1%)
contain and release histamine
What are the 2 types of agranulocytes
monocytes (2-6%)
travel into the tissue and mature into macrophages
lymphocytes (25-33%)
specific immune defenses
B, T and NK cells
what is a mnemonic to remember decreasing abundance in blood
Mnemonic to remember decreasing abundance in blood: Never let monkeys eat bananas (neutrophils, lymphocytes, monocytes, eosinophils, basophils)

What is leukopenia
abnormally low WBC count
can be drug-induced, particularly by anticancer drugs or glucocorticoids
what is leukemia
overproduction of abnormal WBCs
Usually involve clones of single abnormal cell
Named according to abnormal WBC clone involved
Myeloid leukemia involves myeloblast descendants
Lymphocytic leukemia involves lymphocytes
Acute (quickly advancing) leukemia derives from stem cells
Primarily affects children
Chronic (slowly advancing) leukemia involves proliferation of later cell stages
More prevalent in older people
Without treatment, all leukemias are fatal
Immature, nonfunctional WBCs flood bloodstream
Cancerous cells fill red bone marrow, crowding out other cell lines
Leads to anemia and bleeding
Death is usually from internal hemorrhage or overwhelming infections
Treatments: irradiation, antileukemic drugs; stem cell transplants
What are platelets
aka thrombocytes
irregular shaped cell fragment from megakaryocytes
play role in blood clotting
normal blood contains 150,000-400,000 platelets/microliter
What is hemostasis
prevents the loss of blood when blood vessels are damaged
requrires clotting factos and substances released by platelets and injured tissues
3 phases that occur at the same time:
vascular spasm
platelet plug formation
coagulation
Detailed steps of hemostasis (step 1)
vascular spasms:
vessel responds to injury with vasoconstriction
vascular spasms are triggered by:
direct injury to vascular smooth muscle
chemicals released by endothelial cells and platelets
pain reflezes
most effective in smaller blood vessels
Detailed steps of hemostasis (step 2)
Platelets stick to collagen fibers that are exposed when vessel is damaged
Platelets do not stick to intact vessel walls because collagen is not exposed
Also prostacyclins and nitric oxide (NO) secreted by endothelial cells act to prevent platelet sticking
Platelet plug formation
Damaged blood vessels cause platelets to become sticky and cling to the site
These platelets release chemicals that:
Attract other platelets
Cause vasoconstriction
When not damaged, normal endothelial cells release prostacyclin and NO to inhibit platelet aggregation
Detailed steps of hemostasis (step 3)
coagulation
is the clotting cascade
involves 13 clotting factors
requires Ca2+ presence
summary of events:
An initial inactive clotting factor, found in the plasma, is activated by exposed collagen
This activates the next factor and so on….. Until thrombin converts fibrinogen into fibrin
What are the intrinsic and extrinsic pathways
intrinsic:
initiated when Hageman factor is activated by exposed collagen
extrinsic:
Factor X is activated by thromboplastin released by damaged tissues
What is the role of thrombin in the clotting cascade
Converts fibrinogen to fibrin
Activates stabilizing factor (XIII)
Enhances conversion of more thrombin from prothrombin
Enhances platelet aggregation
What is clot retraction
platelets rtapped in the clot contract and squeeze serum out
what is vessel repair
platelets attract fibroblasts that repair blood vessel
what is clot dissoultion
urokinase and tissue plasminogen activator (tPA) converts plasminogen into plasmin which breaks down fibrin
what are 2 major types of hemostasis disorders
thromboembolic disorders:
results in undesirable clot formation
bleeding disorders:
abnormalities that prevent normal clot formation
what is the difference between thrombus, embolus and embolism (thromboembolic conditions)
Thrombus: clot that develops and persists in unbroken blood vessel
May block circulation, leading to tissue death
Embolus: thrombus freely floating in bloodstream
Embolism: embolus obstructing a vessel Example: pulmonary or cerebral emboli
Risk factors: atherosclerosis, inflammation, slowly flowing blood or blood stasis from immobility
what are some drugs to help/cure thromboembolic conditions
Anticoagulant drugs: used to prevent undesirable clotting
Aspirin: lowers heart attack incidence by 50%
Heparin: used clinically for pre- and postoperative cardiac care as well as to prevent venous thrombosis
Warfarin: reduce risk of stroke in patients prone to atrial fibrillation
what is thrombocytopenia
deficient number of circulating platelets
Petechiae appear as a result of spontaneous, widespread hemorrhage
Due to suppression or destruction of red bone marrow (examples: malignancy, radiation, or drugs)
Platelet count <50,000/μl is diagnostic
Treatment: transfusion of concentrated platelets
what is hemophilia
Includes several similar hereditary bleeding disorders
Hemophilia A: most common type (77% of all cases) due to factor VIII deficiency
Hemophilia B: factor IX deficiency
Hemophilia C: factor XI deficiency, milder
Symptoms include prolonged bleeding, especially into joint cavities
Treatment: injections of genetically engineered factors; has eliminated need for plasma transfusion.
Restoring blood volume
Death from shock may result from low blood volume
Volume must be replaced immediately with
Normal saline or multiple-electrolyte solution (Ringer’s solution) that mimics plasma electrolyte composition
Replacement of volume restores adequate circulation but does not replace oxygen-carrying capacities of RBCs
transfusing RBCs
Whole-blood transfusions are used only when blood loss is rapid and substantial
Infusions of packed red blood cells, or PRBCs (plasma and WBCs removed), are preferred to restore oxygen-carrying capacity
Blood banks usually separate donated blood into components; shelf life of blood is about 35 days
Human blood groups of donated blood must be determined because transfusion reactions can be fatal
Blood typing determines groups
how many blood types are there?
8
A-
A+
B-
B+
AB-
AB+
O-
O+
What antigens and antibodies do the blood types have in their plasma
A-: A antigen , Anti-B antibody
A+: A antigen, Anti-B antibody
B-: B antigen, Anti-B antibody
B+: antigen, Anti-B antibody
AB-: BOTH A and B antigens, NEITHER antibody
AB+: BOTH A and B antigens, NEITHER antibody
O-: NEITHER A nor B antigen, BOTH anti-A and anti-B antibodies
O+:NEITHER A nor B antigen, BOTH anti-A and anti-B antibodies
what blood type is the universal recipient
AB+
What blood type is the universal donor
O-
What is agglutinogens
agglutinogens= antigens
are antigens on the surface of red blood cells
what are agglutinins
agglutinins= antibodies
Agglutinins are antibodies in the plasma
Agglutination Reaction of ABO Blood-Typing with Antisera
Anti-A Serum | Anti-B Serum | Blood Type |
Agglutination | No Agglutination | Type A |
No Agglutination | Agglutination | Type B |
Agglutination | Agglutination | Type AB |
No Agglutination | No Agglutination | Type O |
Explain Hemolytic disease of the newborn and the rationale for treatment
a condition in which a Rh- mother who was previously sensitized by a blood transfusion or a previous Rh+ pregnancy carries a fetus who is Rh+ and the mother’s anti-Rh antibodies enter the fetus’s circulation
this causes agglutination and hemolysis of the fetus’s RBCs
Treatment for this condition is to remove the fetus’s Rh+ blood and replace it with Rh- blood from an unsensitized donor to lower the level of anti-Rh antibodies.