Regeneration and healing
1/7
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
8 Terms
What are the 2 processes of damaged tissue repair after inflammation and what are they both triggered by?
Regeneration
Scarring (fibrosis)
Both processes triggered by :
Cytokines and growth factors (produced mainly by macrophages)
Anti-inflammatory cytokines to terminate inflammation.
Growth factors to promote repair
Regeneration most seen in epithelium of … and explain with examples the 3 types (labile, stable and permanent) proliferative capacity of tissue?
Regeneration seen: in epithelia of skin liver and intestine as have proliferative capacity and contain abundant tissue stem cells.
Proliferative capacity of tissue:
Labile tissue (continuously dividing tissue)
Cells continuously being lost and replaced → g1 growth
Eg: Heamatopoietic cells (bone marrow), and surface epithelia (epidermis, ailementary tract, respiratory tract , urinary tract)
2.Stable tissues:
Minimal replicative and only proliferate in response to injury (stimulus)
Cells Quiscent (inactive) → G0 phase
Eg: Kidney, fibroblast, vascular endothelium, parenchyma of solid tissue, smooth muscle
3.Permanent tissues:
Terminally differentiated and nonproliferative in postnatal life → Irreversible injury leading to scar
E.G: neurons , cardiac muscle and skeletal muscle cells
Fibrous tissue
Why it happens?
Repair by connective tissue deposition
Repair sequence
Scar vs Fibrosis
Fibrous Tissue (scar) is formed: if the tissue is unable to regenerate/ the structural framework is irreversibly damaged.
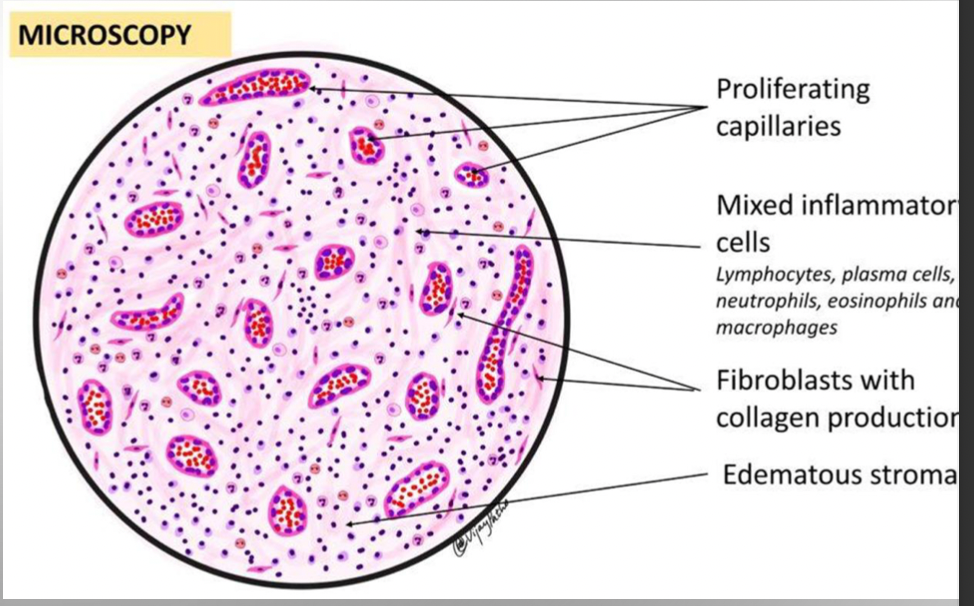
Repair by connective tissue deposition consists of
1.Formation of new blood vessels (angiogenesis)
2.Migration and proliferation of fibroblasts → Collagen synthesis
3.Deposition of Extracellular Matrix (scar formation)
4.Maturation and reorganization of the fibrous tissue(remodeling)
(Repair sequence)
During initial 3-5 days of repair injury site filled with newly formed capillaries, macrophages and fibroblast embedded in granulation tissue (loose extracellular matrix).
Gradually collagen is laid down by fibroblast to form scar.
Scar vs Fibrosis
Collagen deposited in peripheral site (limb, skin) = scar,
Collagen deposited in parenchymal organ in abnormally large amounts (liver, lung), = fibrosis
Fibrosis / Scarring (Describe growth factors involved in repair and angiogenesis)
Growth factors
tgf-β and fibroblast growth factor (FGF) act on fibroblasts in connective tissue → Stimulate their proliferation and collagen synthesis.
VEGF → Formation of new blood vessels that provide nutrition to proliferating fibroblast
Angiogenesis
Vasculogenesis : Vascular network formed from angioblast (endothelial cell precursors)
Neovascularization : Pre-existing vessels send out capillaries to produce new vessels
Cutaneous wound healing : Healing by 1st intention
Healing by 1st intention
Occurs : Clean, uninfected surgical incision of skin closed with surgical sutures
Steps:
Wound initially sealed by blood clot → neutrophil and macrophage arrive
→ small amount of granulation tissue formed → replaced by thin scar
→ surface epithelial cells regenerate and bridge incisional gap
Cutaneous wound healing : Healing by 2nd intention
Healing by 2nd intention
Occurs: More severe, deep skin injuries where edges can’t be closed
Same sequence of events but…
Granulation tissue much larger and persists for longer
More collagen is laid down
Fibrous scar is thicker
By about 4 to 6 weeks, the skin wound is closed with a dense scar.
The skin wound contracts cuz of myofibroblasts action in the connectivetissue.
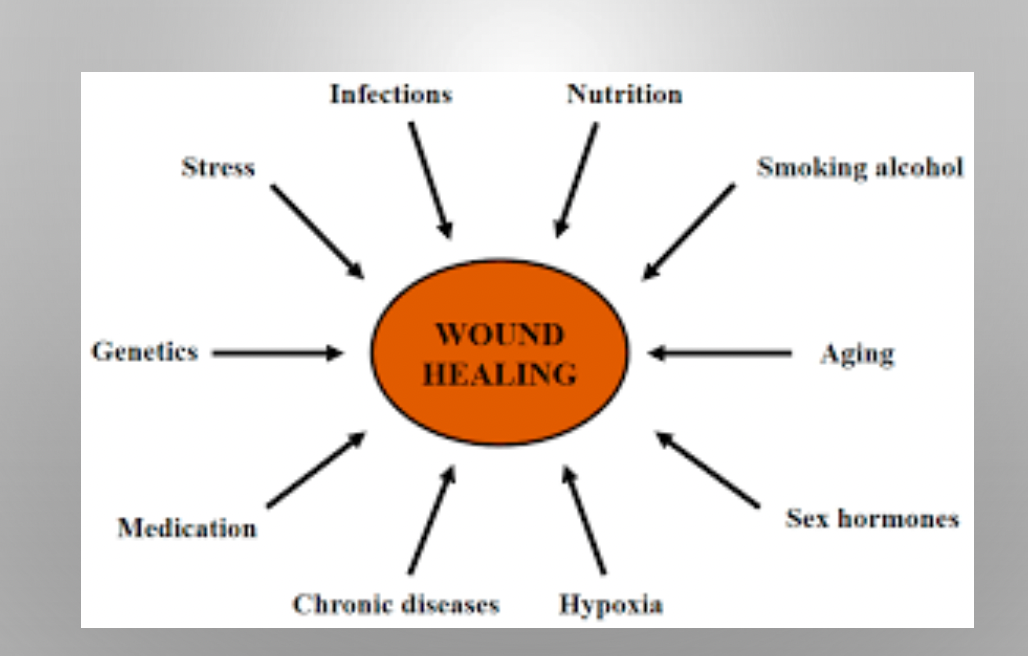
Factors impairing repair
Mechanical factors: like excessive movement and pressure
Infection: prolongs inflammation and causes progressive tissue injury
Diabeties :
Underlying metabolic abnormality
vascular narrowing leading to reduced blood supply,
↑ suceptible to infection due to ↓ neutrophils function and impaired cytokine production by macrophage
Poor perfusion (adequate blood supply) due to atherosclerosis , diabetes..
Excessive repair process conditions
Hypertrophic scars
Develop following injury
Usually regress slowly
Eg:knee joint
Keloids
Scar tissue grows beyond injury margins
Fails to regress
Excess scaring leads to serious disorders such as Pulmonary fibrosis , Liver Cirrhosis