ISD4 The Dentine Pulp Complex
Dentine:
The internal mineralised structure of the tooth
It’s overlaid by enamel in the crown and cementum in the roots
At the CEJ, you can have either/both/neither enamel and cementum
Dentine composition: 70% mineral, 20% organic and 10% water.
45% volume of calcium hydroxyapatite (mineral)
30% volume of collagen (90%) and non-collagenous proteins (DPP&DSP) (organic)
25% volume of water
Is not quite as hard as enamel but the added water/collagen/organic components give it more elasticity.
Early dentine is similar to bone
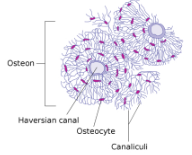
Osteocytes embedded in the bone
Single units of osteons
Through the middle of each osteon is the Haversian canal
Polarised odontoblasts on the periphery with trailing odontoblast process
It migrates away from the dentine as it lays down so it ends up on the inner surface of the dentine
As they are producing the dentine precursor and mineralising it, they leave behind the odontoblast process. This occupies the dentinal tubule
Many dentine variations:
Primary:
Mantle:
Peripheral dentine (supporting overlying enamel)
Peritubular Or Intertubular dentine:
Circumpulpal dentine (overlies the pulp)
Secondary
Tertiary (reactionary or reparative)
Primary dentine = 3-3.5mm thick
Predentine matrix secreted by cells that become mineralised
Mantle:
Atubular
20um thick
Under/unphosphorylated proteins
Elastic/Resilient
Dissipates forces to avoid fracture propagation
Tomes Granular Layer/Tomes Layer)
Intertubular dentine - predentine mineralises - 4-10um per day
Peritubular (Intra) - odontoblast process modifies amorphous matrix
15% more mineralised than intertubular
Accelerated with tubular sclerosis during an insult
Reduces permeability of dentine to endodontic irrigants i.e. older teeth or those which have had chronic inflammation are less permeable to irrigants
Amelodentineal Junction:
Scalloped in appearance at areas of high-load
Dentinal tubules follow S-shaped curvature - “Primary curvatures” - more pronounced in the crown than the root.
Secondary dentine
Commences production when the tooth becomes functional
<1 micron per day
Becomes the most internal layer of circumpulpal dentine
Very similar structure to primary dentine
Tertiary dentine
Reactionary - upregulation of pre-existing odontoblast layer to secrete more predentine which is subsequently mineralised
Reparative - Odontoblast cells are killed or removed and then local stem cells/progenitor cells are recruited to repair the tissue. Atubuler, an irregular structure that is rapidly produced following more severe insults that disrupt the odontoblast layer.
Key Player = Odontoblast
→ Cells polarise
→ Produce pre-dentine
→ Secrete non-collagenous proteins and enzymes that initiate mineralisation
Condense together as cells migrate centrally from ADJ to pulp so the surface area of the dentine-pulp layer is less than at the enamel-dentine layer. This means that the odontoblast process and dentine tubules condense closer together so they occupy a greater area. Therefore, there are more dentinal tubules towards the pulp than the ADJ.
Tubular % surface area:
1% just beneath the enamel
22% towards the pulp
This increase is associated with a corresponding increase in the dentine water content towards the pulp
Diameter of the tubules:
3um adjacent to the pulp
~0.8um near the ADJ
If you were trying to reduce the depth of your restoration, as you go further into the dentine, you are exposing more tubules and wider tubules.
Length of odontoblast process:
0.1-1mm in length (approximately the inner third of dentine)
The shallower the restoration, the better in order to disrupt less odontoblast processes.
Dental Pulp
Unmineralised, loose connective tissue
Vascular
High water content (~75%)
Organic components predominantly type 1 and 3 collagen
Cellular components predominantly fibroblasts
Peripheral odontoblasts
Immune cells - lymphocytes, macrophages, dendritic cells
Endothelial cells (pericytes) and lymphatic vessels also
Pulp-Dentine Complex
AKA - Dentopulpal Complex/Dentine Pulp Complex
Dentine protects the pulp ←→ Pulp serves the dentine
The odontoblasts process extends into dentine
It is best to consider both structures as one
Zones of the Pulp
Odontoblast layer
Cell free zone
Cell rich zone
Pulp core
Histological zones
Pulp site-dependent
It is best considered a continuum
Peripheral Fishnet Appearance:
Central arterioles and venules
Subodontoblastic plexus (beneath the dentine, immediately below the odontoblasts)
Aterio-venous and venous-venous anastomosis surrounding these structures
Embryology
Tooth development involves complex interactions between Ectoderm (external layer) and Mesenchyme (internal layer)
Epithelium forms from Ectoderm - enamel is ectodermal origin
Neural crest cell migration is imperative for dentine, pulp, cementum - ectomesenchyme
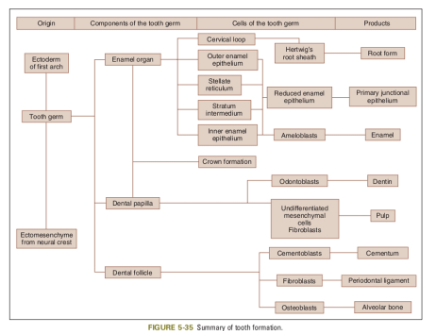
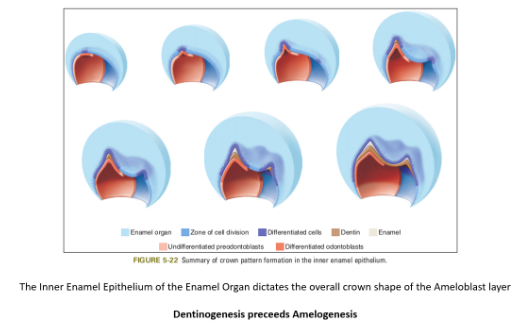
Amelodentinal Junction:
Inner enamel epithelium and dental papilla
Ameloblasts (enamel producing)
Odontoblasts (dentine producing)
Functions of the Pulp:
To create dentine
Supply nutrients to the odontoblasts
Innervate the tooth
Defend against insult, especially bacteria
Pulpal Inflammation
Predominantly opportunistic micro-organisms
Caries (most common)
Acid-producing bacteria - demineralises dentine
Sequestered growth factors are liberated (liberated-dentine-derived ECM proteins)
Diffuse into odontoblast layer
Odontoblasts upregulate secretion
Innate responses - vascular changes:
Normal blood flow in the pulp
Normal fluid flow into dentine
Can be caused by drilling and causing damage to odontoblast processes which, in turn, release cytokines and cell mediators which increase blood flow and increase the likelihood of causing pulpitis
Cellular responses follow - upregulation
Pulpal Innervation and Pain
Pupal nerve fibres - A-delta, A-beta, C fibres and sympathetic fibres
Peripherally-sited A-delta (myelinated)
Centrally-located C-fibres (unmyelinated)
The majority of nerve fibres are reported to be unmyelinated
A-delta = short sharp pain of short duration
C-fibres = dull aching pain associated with more advanced pulpal inflammation.
Hydrodynamic Theory:
Peripherally sited A-delta (myelinated)
Not thermally mediated
Outward flow of fluid due to contraction and expansion of dentine to the thermal changes
Cold = outward flow
Heat = inward flow
Indirect Pulp Cap
- Cavity ½ dentine depth
Assuming pulpal pressure stays the same
Radius increases x16
Length of tubule x0.5
Fluid flow increase x32
- Cavity ¾ dentine depth
Assuming pulpal pressure stays the same
Radius increases x256
Length of tubule x0.25
Fluid flow increases x1024
Key Message:
Deeper cavities:
Expose a greater number of tubules
These tubules have a greater diameter (i.e. surface area)
Cause greater damage to odontoblast processes i.e. less reactionary dentine
Have greater fluid flow
Wet environment for bonding
Allow greater pulpal irritation from restorative materials
Vital Pulp Therapies
“Strategies aimed at maintaining the health of all or part of the pulp”
i.e. avoiding RCT or XLA
Indirect pulp cap
Selective removal CT (1 stage) to firm or soft dentine
Stepwise excavation (2 stage)
Non-selective removal CT (total caries removal)Direct pulp cap
a. Class I - trauma or iatrogenic
b. Class II - deep/extremely deep carious lesion
Partial pulpotomy
Full pulpotomy
Clinical diagnosis is fundamental:
Pulpal diagnosis’Depth and extent of caries (revisit ICDAS)
Take Home Message:
Asymptomatic tooth
Reversible pulpitis
Deep caries
= Avoiding pulp exposure is considered best practice!
Includes: severe reversible pulpitis - increased pain to stimuli for more than several minutes that may require analgesics (Do options 1-3 from above)
Irreversible pulpitis
= Requires caries removal and pulp exposure
Most cases will require partial/full pulpotomy
Vital Pulp Therapies
What to do if you expose the pulp during caries removal?
→ Place cotton pellet soaked in saline to stop bleeding
→ Place biodentine and review
Hydraulic calcium silicate cement
Antibacterial
More consistent dentine bridge than CaOH
Remineralise dentine
Weak mechanical characteristics
→ Speak to supervisor if not in scope (adult tooth)
If biodentine is not available, then:
Setting CaOH cement should be used e.g. DyCal or Life
Non-setting CaOH paste e.g. HypoCal
Then on top you use GIC or zinc oxide eugenol.