Normocytic Anemia I (ExtraVascular Hemolysis)
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
Hemolysis is known to be
Increased Destruction → Has increased reticulocyte count
Can be classified as:
Causes: Intrinsic to RBC vs extrinsic to RBC
Location of hemolysis:
Intravascular and Extravascular
What are the features of all Hemolytic Anemias
Shortened RBC lifespan due to destruction
Reticulocytosis
Liberation of hemoglobin of degradation products
Increased unconjugated (Indirect) bilirubin = acholuric
jaundice (Jaundice without bilirubinuria)
Increased erythropoiesis → Normoblastic erythroid hyperplasia in marrow
Pigmented gallstones
Increased LDH
Decreased/No Haptoglobin
Features of Intravascular Hemolysis
Red cells lyse inside circulation and
release products into blood
Anemia
Reticulocytosis
Decreased Haptoglobin
Increased LDH
Increased Urine Urobilinogen
Plasma hemoglobin
Urine Hemoglobin
Urine Hemosiderin
Methemoglobinemia
DAT negative
Schistocyte
Features of Extravascular Hemolysis
Ingestion of RBCs by macrophages in liver, spleen and bone marrow
Anemia
Reticulocytosis
Decreased Haptoglobin
Increased LDH
Increased Urine Urobilinogen
Normal plasma hemoglobin
DAT positive
Spherocytes
Splenomegaly
Location of Extravascular Hemolysis
Liver, spleen, lymph node
Extravascular Hemolysis Is Caused By
Hereditary Spherocytosis
Sickle cell anemia
Hemoglobin C
Autoimmune hemolytic anemia (AIHA)
Thalassemias
Intravascular Hemolysis Is Caused By
Glucose-6-phosphate dehydrogenase (G6PD) deficiency
Paroxysmal nocturnal hemoglobinuria (PNH)
Malaria
Hemolytic Disease of the Newborn Microangiopathic/thrombotic hemolytic anemia
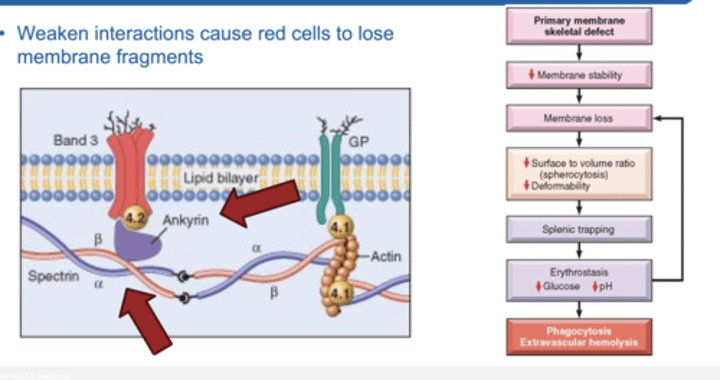
Hereditary Spherocytosis/Elliptocytosis
Autosomal Dominant
Defect of RBCs cytoskeleton-membrane connecting proteins → Ankyrin (band 3 protein, for spherocytosis) → Spectrin (band 4.2 protein, for elliptocytosis)
Cells becomes round → less capable to maneuver in the spleen
Eventually engulfed by spleen macrophages
Splenomegaly
***50% of people will get cholelithiasis due to pigmented gallstones***
Increased MCHC – not usually seen on other anemias !!!
Can have aplastic crisis with Parvovirus B19 infection
Pathophysiology of Hereditary Spherocytosis
Weakened interactions cause red cells to lose membrane fragments
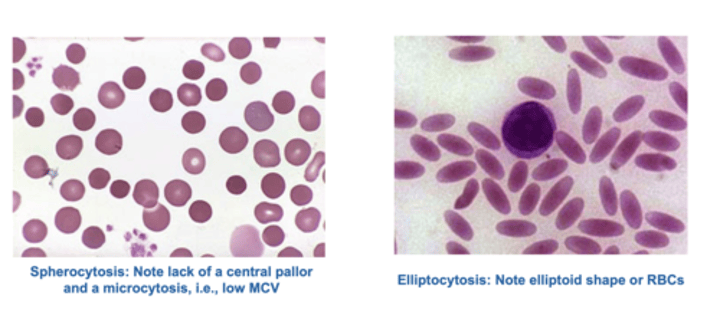
Hereditary Spherocytosis/Elliptocytosis Histological Slides
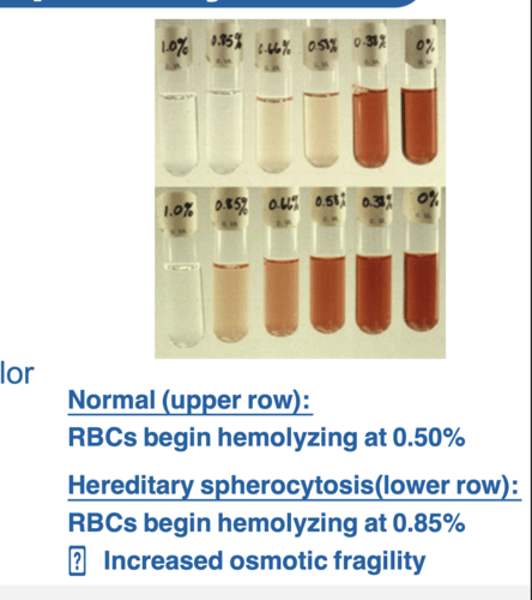
Diagnosis of Hereditary Spherocytosis
Normocytic anemia (MCV 80-100)
Hemoglobin: Mildly reduced
MCH: Normal
MCHC: Increased*
Reticulocyte count: increased (>3%)
Peripheral smear → Red cells appear small and lack central pallor
Polychromasia and Nucleated RBC’s
– Confirmatory test
Osmotic fragility test
Clinical Features of Hereditary Spherocytosis
Triad of findings:
1. Anemia
2. Splenomegaly
3. Jaundice: due to increased unconjugated bilirubin.
Other findings:
1. Gall stones (calcium bilirubinate) → Due to increased concentration of conjugated bilirubin in bile
2. Aplastic crisis → May occur after parvovirus B19 infections
Consider diagnosis of HS:
FH of splenectomy
Increased incidence of gall stones (jet black calcium biluribinate stones)

Treatment of Hereditary Spherocytosis
Splenectomy (anemia is corrected but RBC defect and Spherocytes persist)
Must give vaccines following splenectomy to protect against sepsis from → S.pneumoniae and H.influenzae
Sickle Cell Anemia Leads To
Red cell distortion
Hemolytic anemia
Microvascular obstruction
Ischemic tissue damage
Sickle Cell Disease
10% of African-Americans carry the gene→ protective role against malaria
Homozygous: presence of 2 abnormal Beta genes (1 in 650 African Americans)
→ >90% HbS in RBCs
Sickle Cell Trait
Heterozygous: presence of 1 abnormal B gene resulting in < 50% HbS
Hb with
Pathogenesis of Sickle Cell Anemia
Deoxygenated HbS molecules undergo aggregation and
polymerization
Can occur through hypoxia, dehydration and acidosis
Process is reversible BUT repeated sickling stiffens RBC membranes, making cells more susceptible to hemolysis and can cause vascular obstruction
Hemoglobin F is protective (first 6 months) – newborns asymptomatic
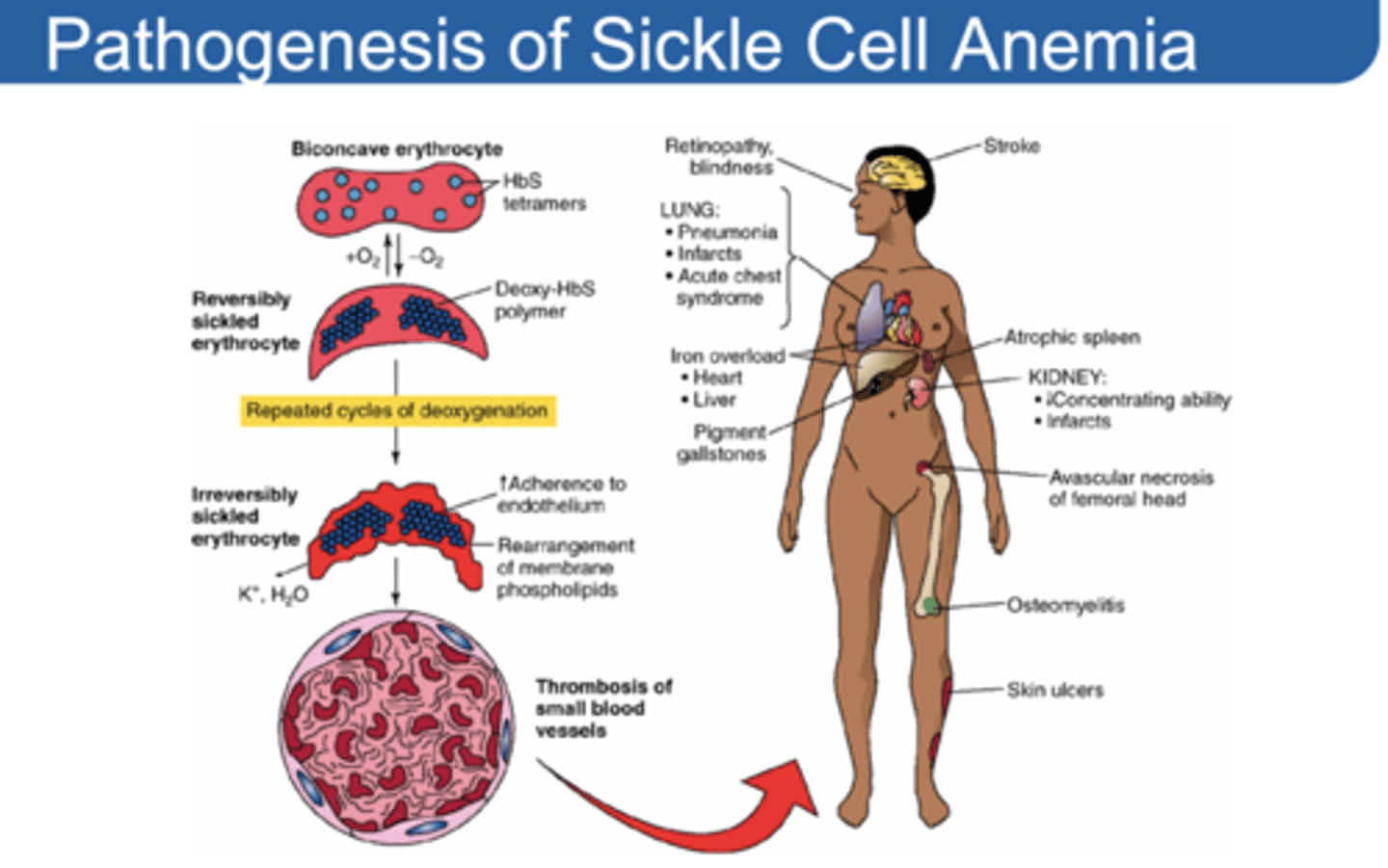
Sticky cells in stacks can cause
Vaso-occlusion and lead to infarction
Features of Severe Hemolytic Anemia
Reticulocytosis - Increased retic count
Jaundice
Hyperbilirubinemia
Erythroid hyperplasia in bone marrow
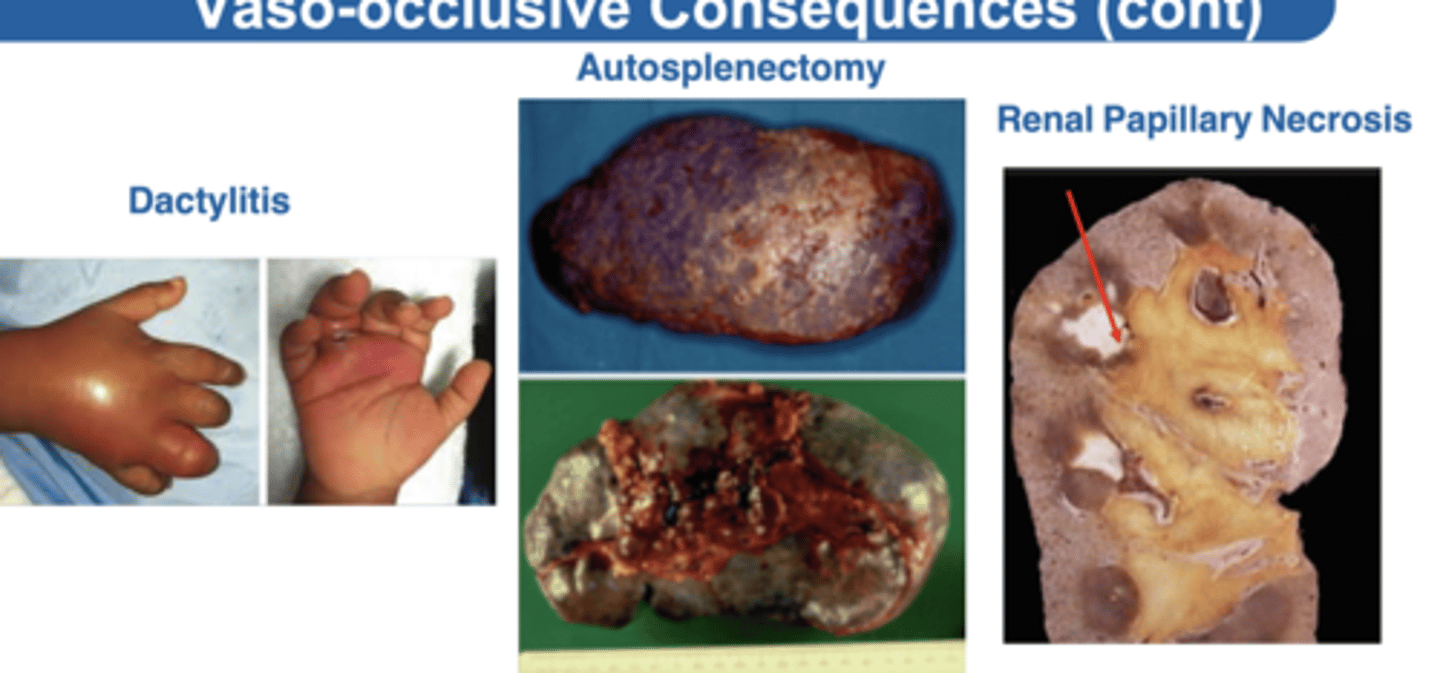
Vaso-Occlusive Consequences
KNOW THESE!!!!!!!!!
Due to extensive and irreversible sickling
Dactylitis: infarction of small bones of the hand, more common in infants
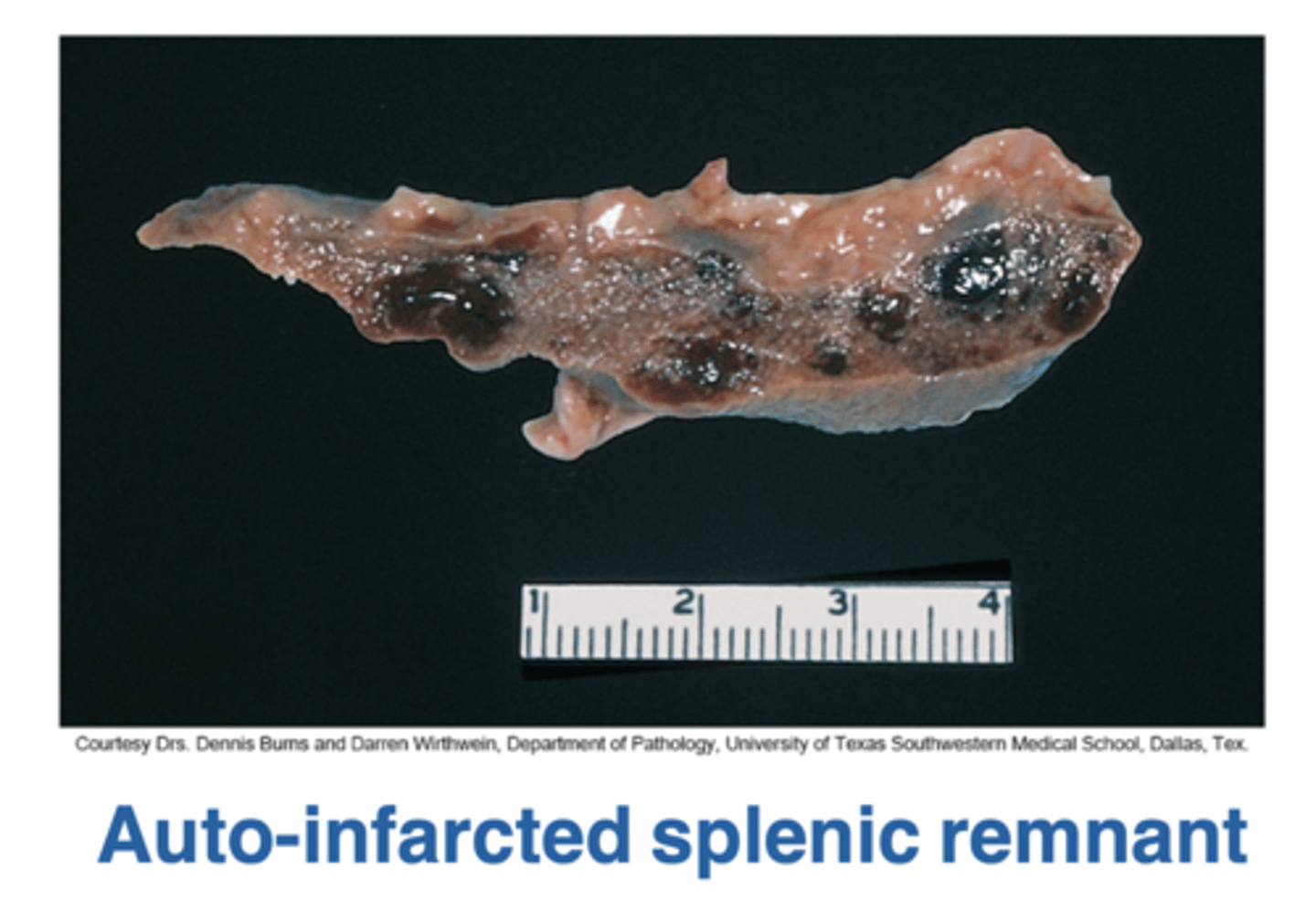
Autosplenectomy: (infarcted, shrunken, fibrotic spleen)
Increased risk of encapsulated organisms → especially pneumococcal
(most common cause of death in infants)
Increased risk of Salmonella osteomyelitis or Salmonella pneumonia
Howell-Jolly bodies in peripheral smear
Acute chest syndrome:
Predisposed by pneumonia
(most common cause of death in adults)
Renal papillary necrosis
Continuation of Vaso-Occlusive Consequences
Pain Crisis – painful limbs, back, chest, abdomen often from infection or dehydration
Aseptic necrosis of femoral head Chronic Leg ulcers → **** Often used as a clinical finding ***
Risk of aplastic crisis – dramatic fall in hemoglobin from → parvovirus B19 viral infection → like spherocytosis
Massive erythroid hyperplasia causes crewcut appearance of skull and chipmunk facies
Factors Affecting Formation of Sickled RBC
1. The presence of hemoglobins other than HbS
2. The concentration of HbS in the cell
3. The length of time that red cells are exposed to low oxygen tension
Treatment:
Hydroxyurea → Increases concentration of Hemoglobin F
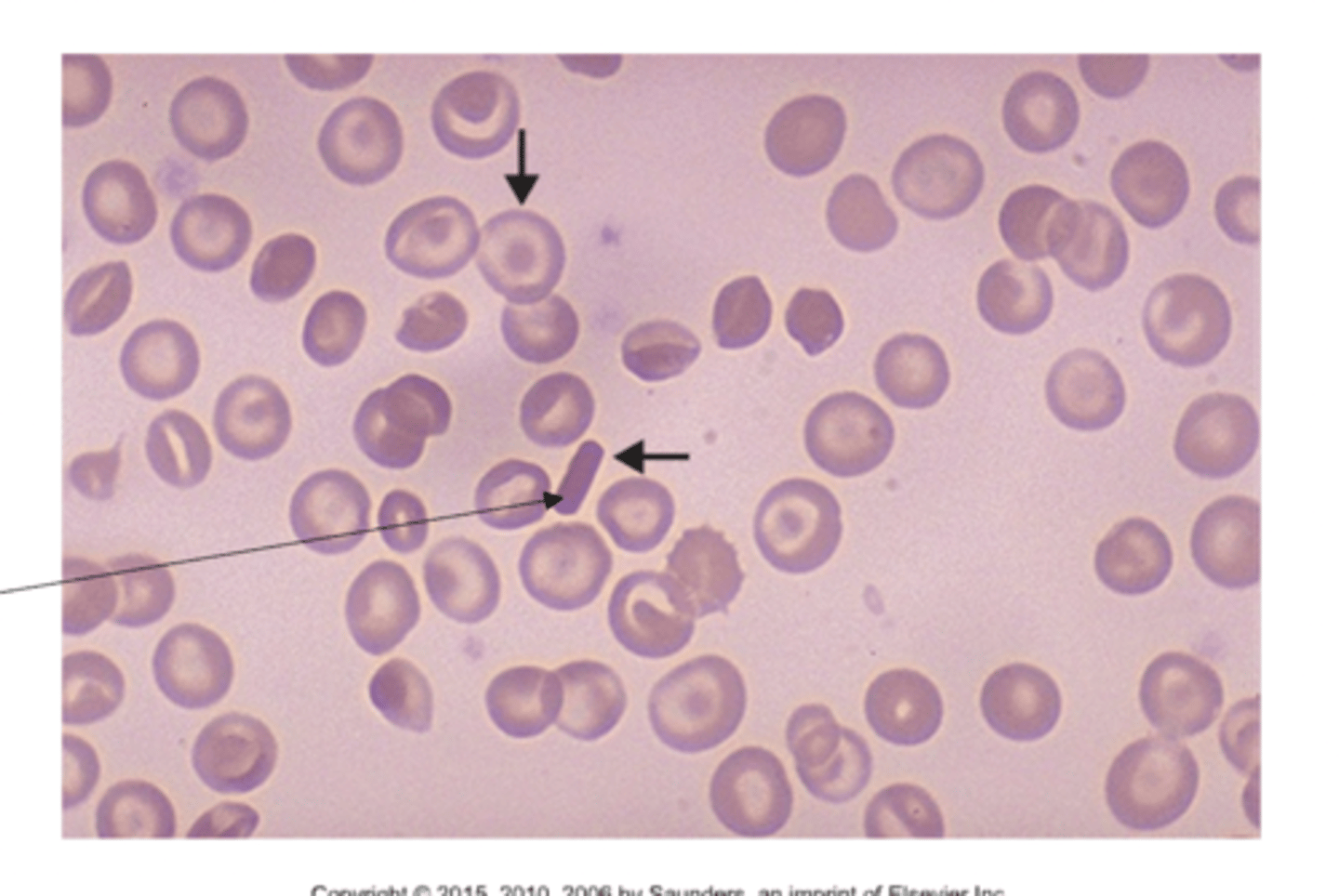
Blood Smear in SCD
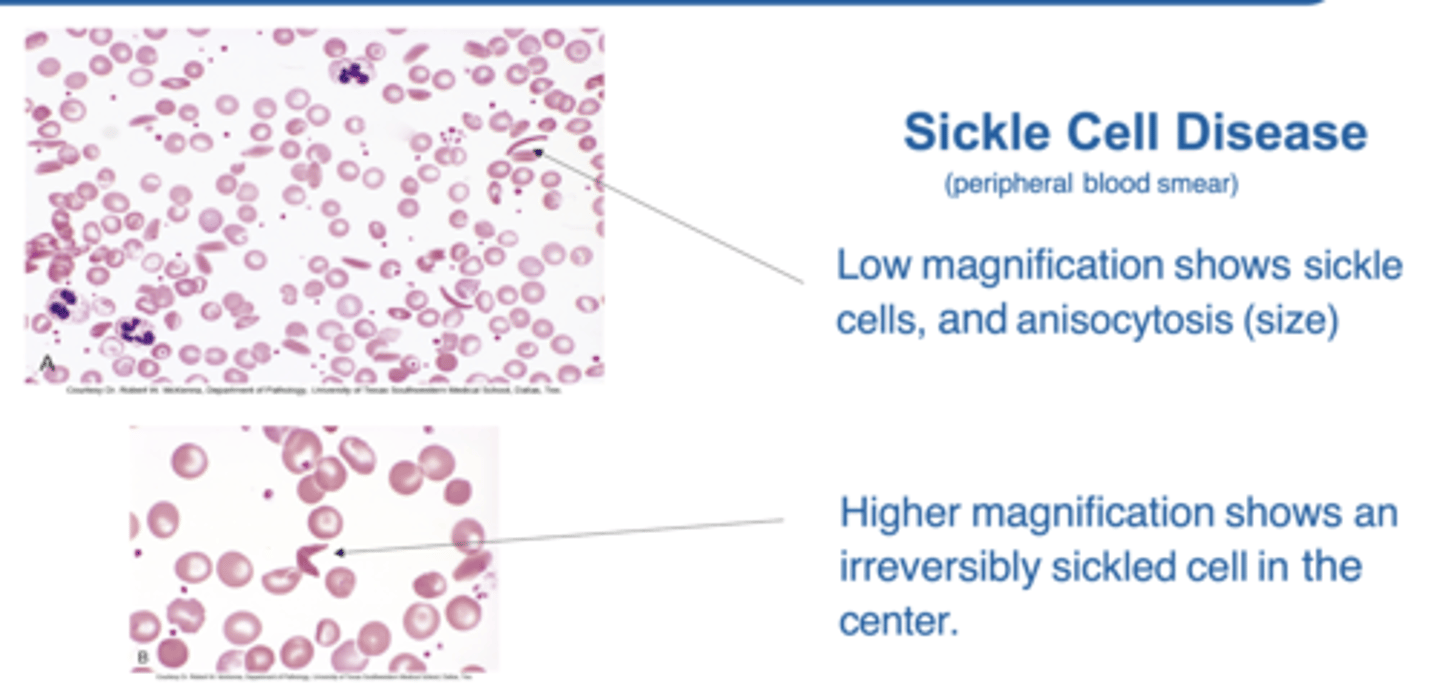
Asplenia
Absence of spleen/absent splenic function
Increased risk of infection
Risk for Encapsulated organisms → Strep. Pneumonia
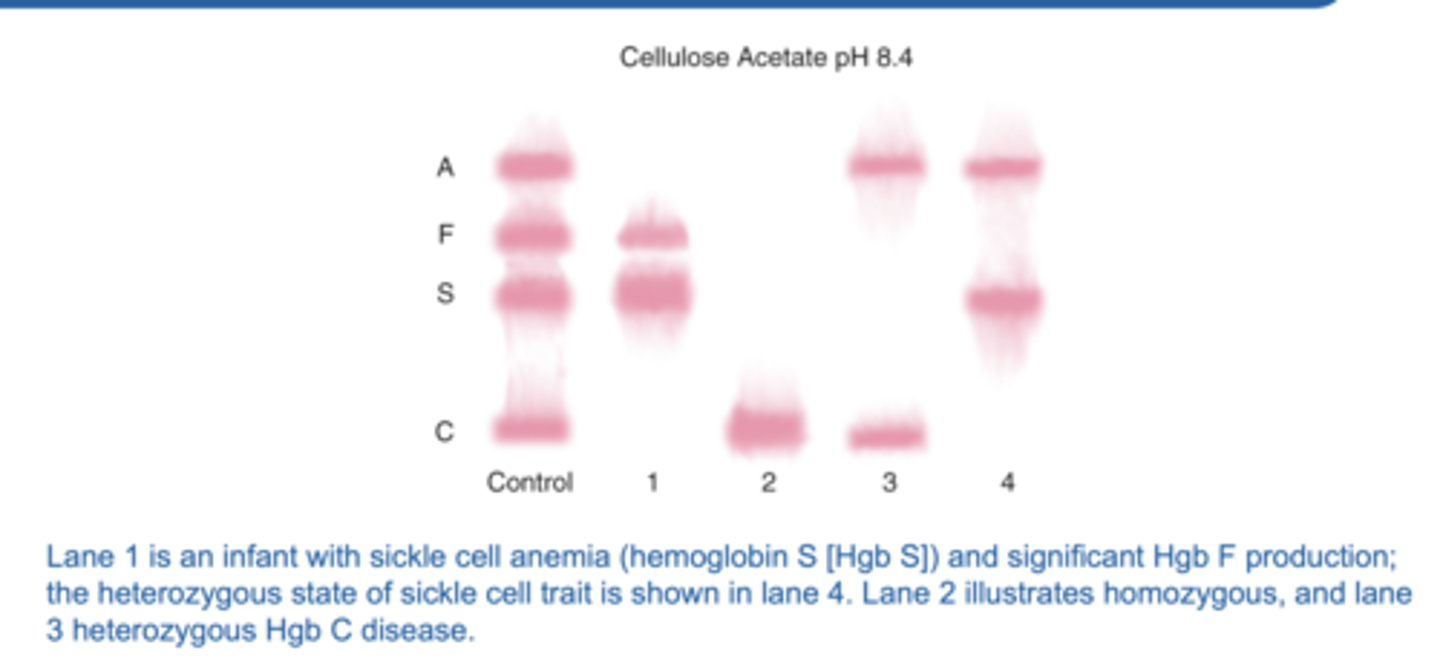
Sickle Cell Lab Findings
SCREEN TEST:
Metabisulfite: causes sickling with any amount of HbS (positive in both disease and trait)
Electrophoresis: presence, and amount of HbS
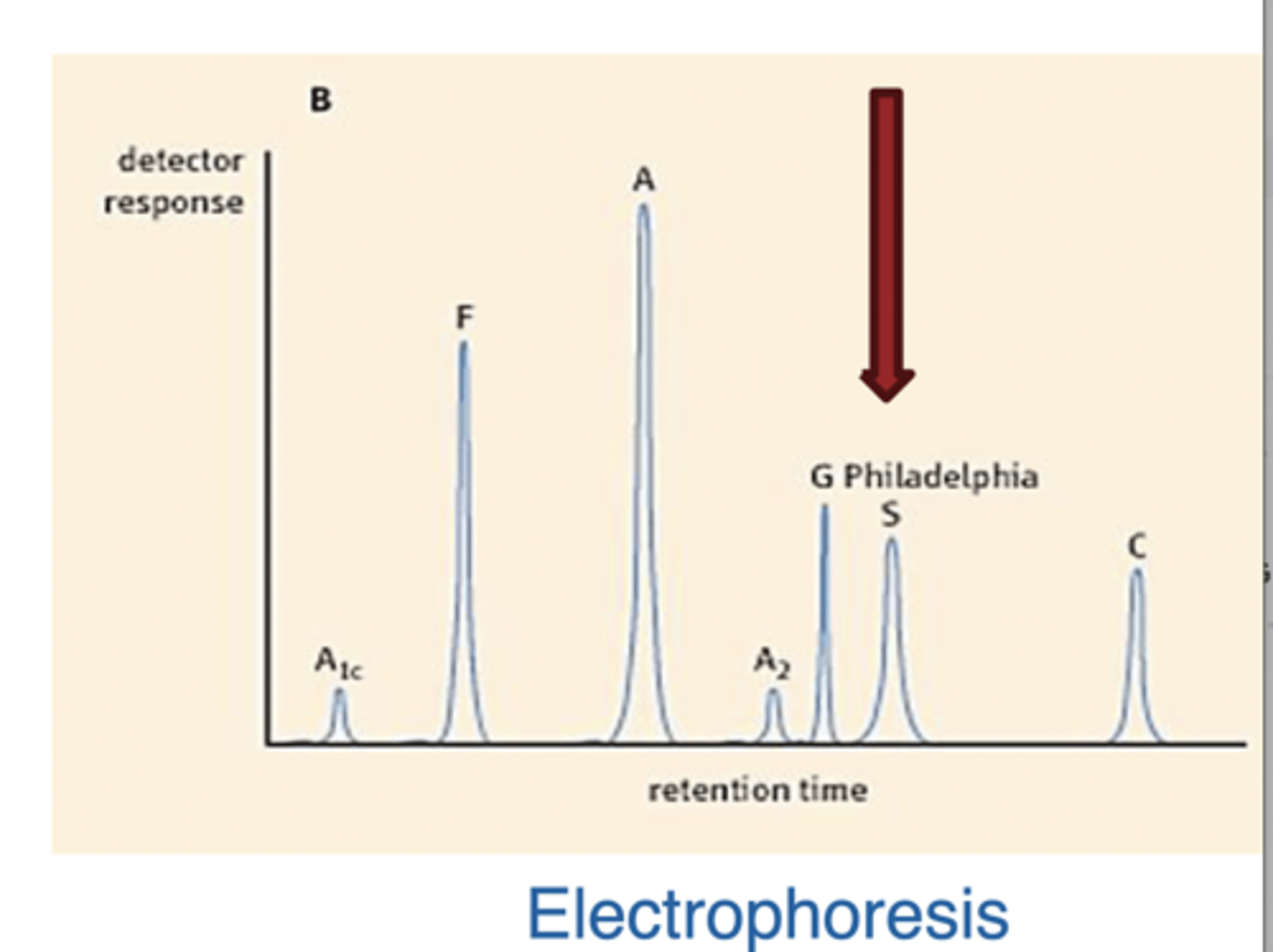
What are the lab findings for Sickle Cell Disease
>50% HbS, (usually >90%)
Some HbF and HbA2 (only few or NO HbA)
What are the lab findings for Sickle Cell Trait
>50% HbA
Hemoglobin Electrophoresis
Hemoglobin C
Glutamic acid is replaced by Lysine
When homozygous → HbC crystals seen on blood smear
Splenomegaly
Target cells
Note: Can have HS and HC combination
More sickling than HC alone
Prone to avascular necrosis of bone and proliferative retinopathy
Autoimmune Hemolytic Anemia
Hemolysis due to antibodies against antigens on RBC
surface
Classification:
1. Autoimmune HA
2. Drug induced HA
3. Alloimmune HA
1. Hemolytic transfusion reaction
2. ABO hemolytic disease of
newborn
3. Rh hemolytic disease of
newborn
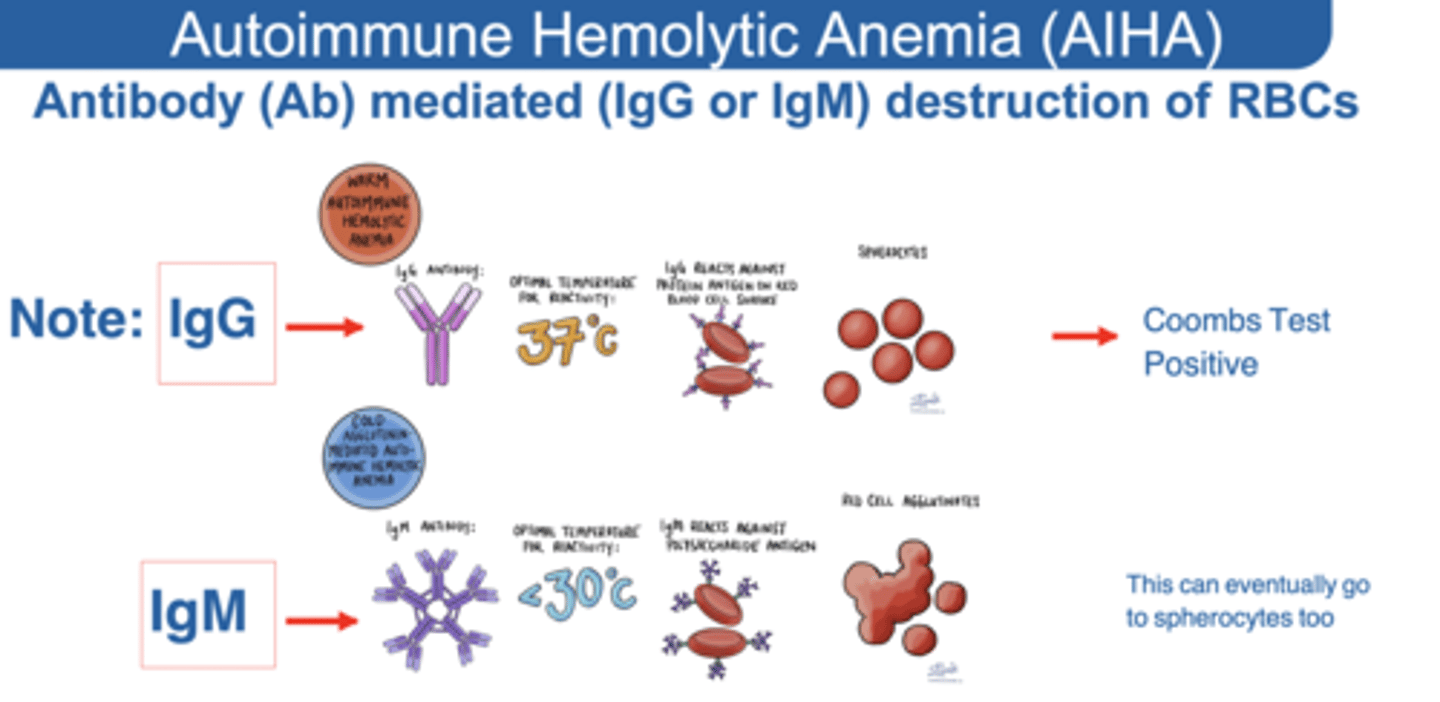
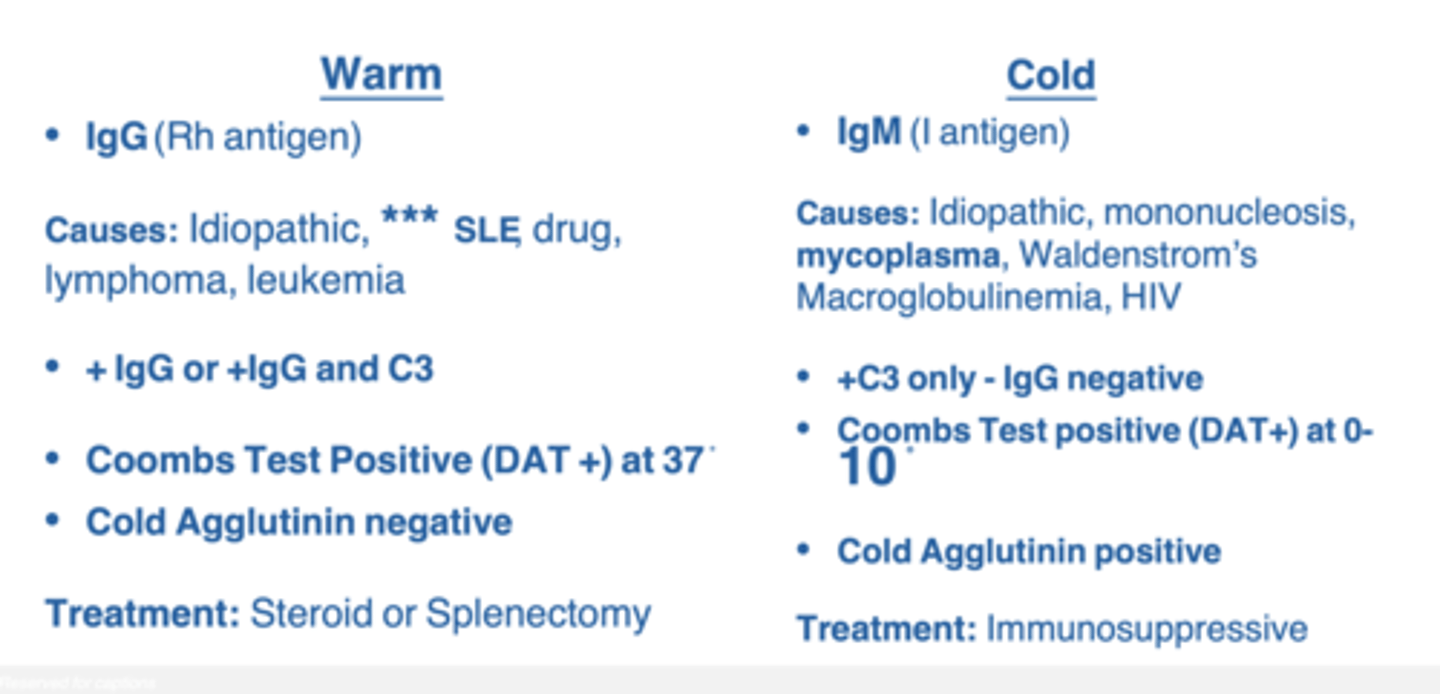
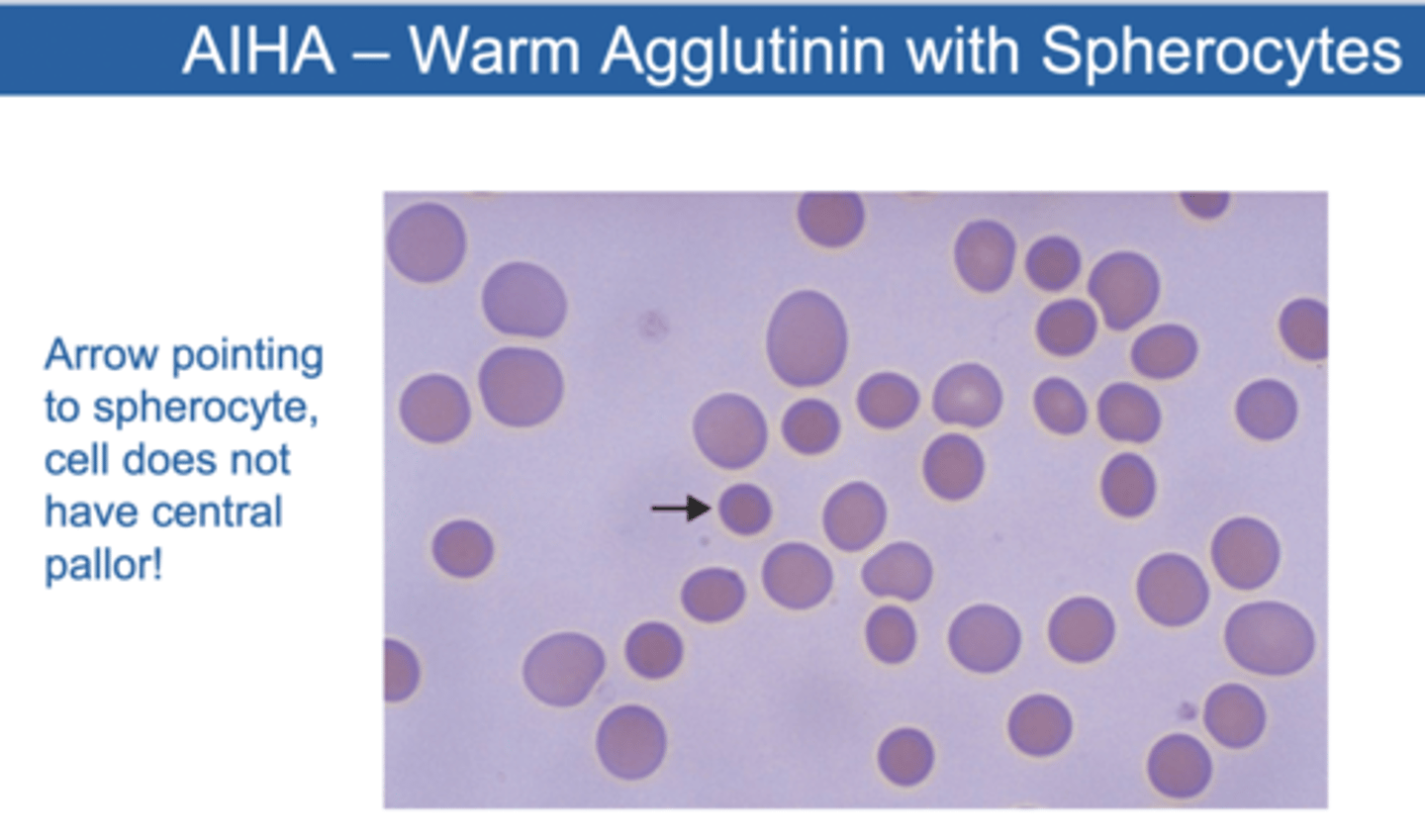
Warm Agglutinins
AIHA→ rare cause of hemolysis precipitated by antibodies directed against blood group antigens
These antibodies are most commonly IgG, and react with proteins on the surface of red blood cells at normal body temperature
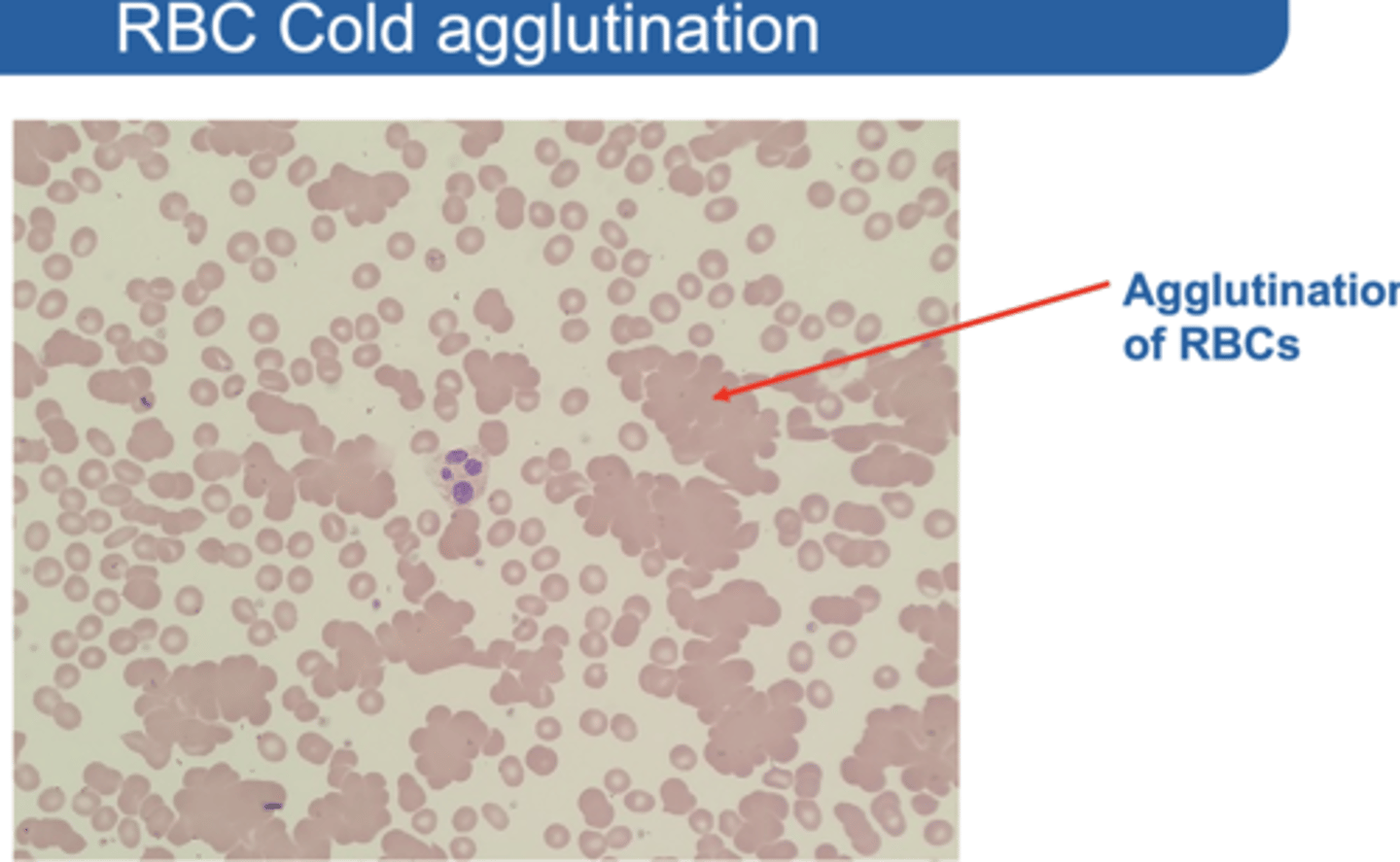
Cold Agglutinins
Autoantibodies that react with antigens on the red blood cell surface
They may induce complement-mediated hemolysis and agglutination of red cells
Can be precipitated following INFECTION in particular MYCOPLASMA PNEUMONIA organisms
IgG Mediated Disease: Warm Agglutinins
Binding occurs in the warm central part of the body
RBCs are coated with the antibodies - Splenic macrophages remove pieces of the RBC membrane including the antibodies → gradual loss of membrane and *** spherocytosis ***
Drugs attach to the membrane or induce autoantibodies
Treatment of Warm Agglutinins
Remove causing drug, IVIG, and splenectomy if necessary
IgM Mediated Disease: Cold Agglutinin
IgM binds to RBCs and fixes complement
Binding occurs in the relatively cold temperature of the extremities
Residual C3b serves as opsonin for splenic macrophages removing some of the membranes → eventual spherocytosis
Can be seen in mycoplasma infection and mononucleosis (EBV)
Extreme activation of complement by excessive antibodies can lead to intravascular hemolysis
DAT Test
Also called Coombs Test
Antibody mediated (IgG or IgM) destruction of RBCs
Used to test presence of RBC coated by the Ab/complement
Anti Ab/complement is added to blood If RBCs are coated → agglutination occurs → positive test
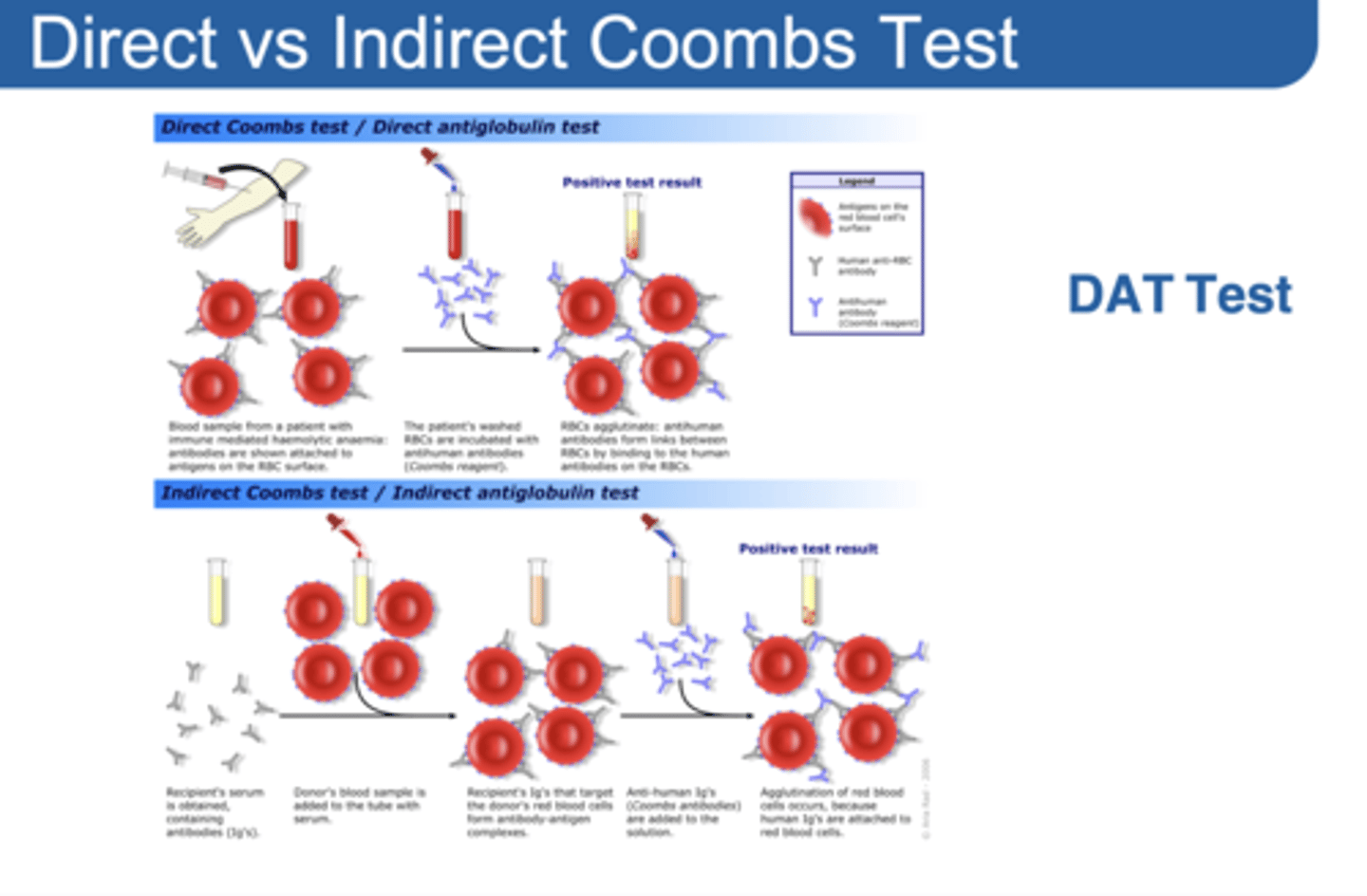
Indirect Coombs test:
Used to test presence of antibodies in patient’s serum
Anti-Antibodies are added to patient’s blood
If antibodies are present → agglutination occurs → positive test
Summary: Characteristics of Agglutinins