8. heart
5.0(1)
Card Sorting
1/97
There's no tags or description
Looks like no tags are added yet.
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
1
New cards
mass transport system
bulk movement of fluid in one direction
2
New cards
factors requiring mass transport system
SA:V ratio
metabolic rate
size
metabolic rate
size
3
New cards
surface are to volume ratio
as the size increases the ratio decreases, as volume increases faster than surface area
4
New cards
unicellular organism
able to rely on diffusion across outer face membrane to supply oxygen and nutrients as large SA:V ration and low metabolic rate allow diffusion to be fast enough
5
New cards
large multicellular organism
diffusion across outer surface is not sufficient to provide all cels with oxygen and nutrients so require specialised exchanged surfaces and a mass transport system. due to small SA:V ratio, cells deep within and high metabolic rate
6
New cards
specialised exchange surfaces
increase surface area for exchange with enviroment eg alveoli in lungs and villi in small intestine
7
New cards
plants
large multicellular organisms which have stomata in leaves to exchange gas, no need to further mass transport system for gas was short diffusion distance but is for water and mineral ions in the form of xylem and phloem
8
New cards
circulatory system
mammalian mass transport system composed of blood vessels (closed system) filled with blood which the heart pumps in one direction
9
New cards
double circulatory system
describes like this as blood is pumped by the heart twice in two circuits (pulmonary and systemic)
10
New cards
pulmonary circulation
circulation that transports blood to the lungs
11
New cards
systemic circulation
circulation that transports blood to the body
12
New cards
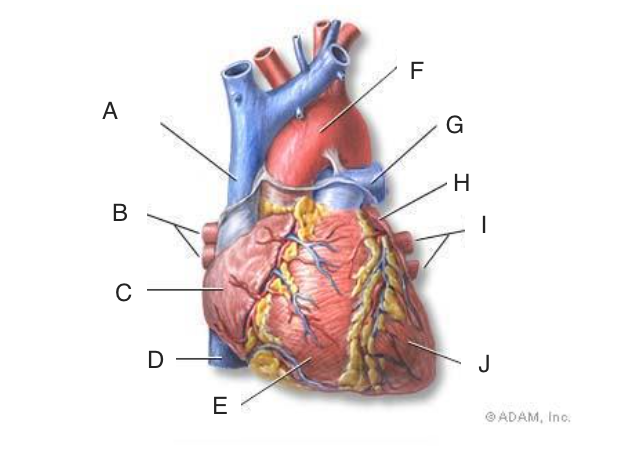
superoir vena cava
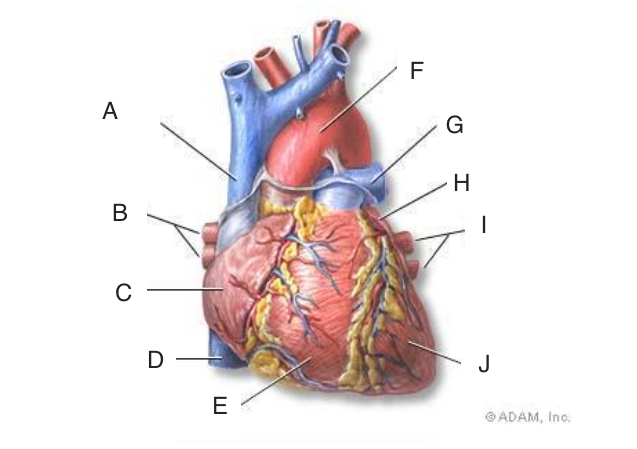
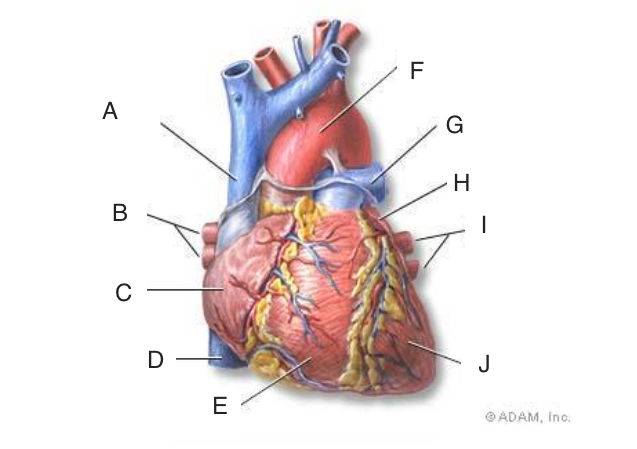
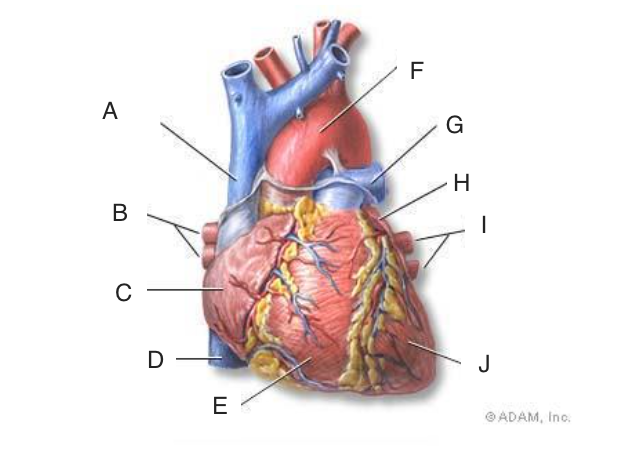
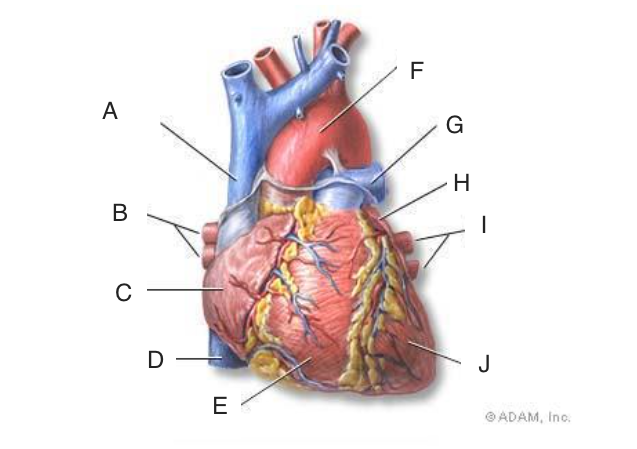
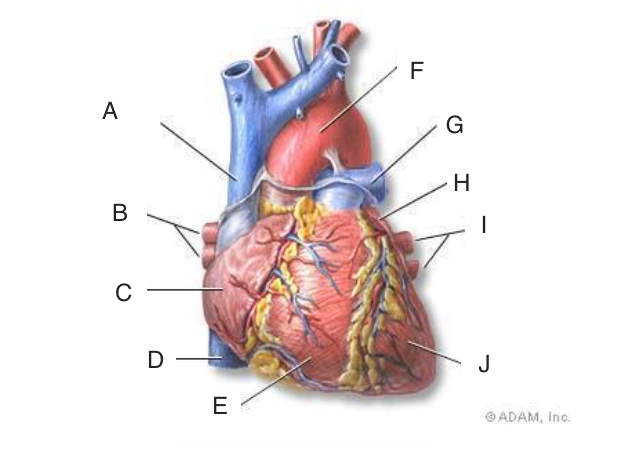
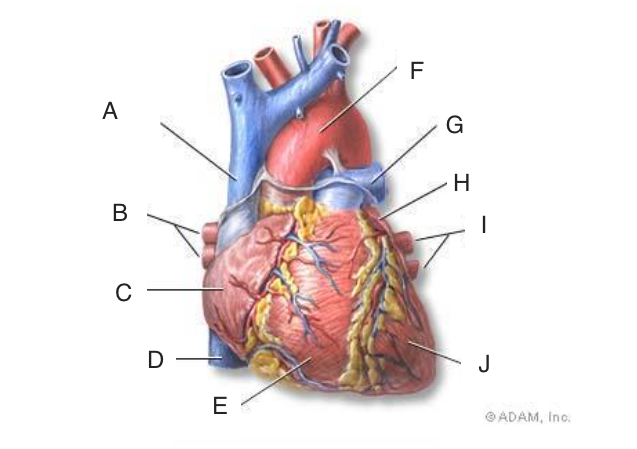
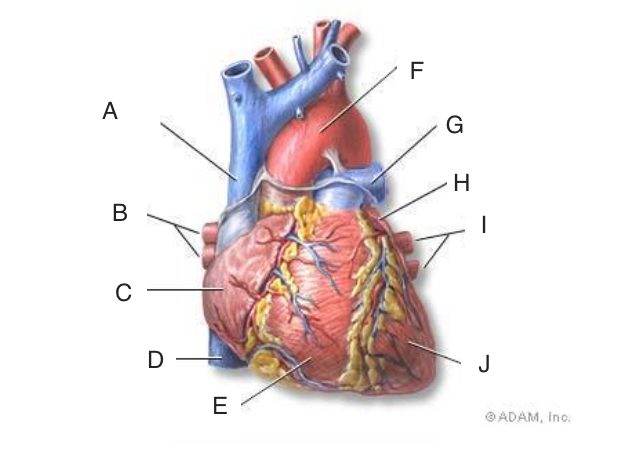
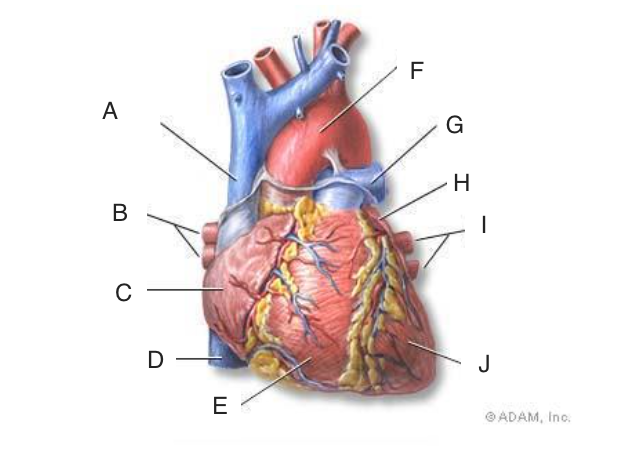
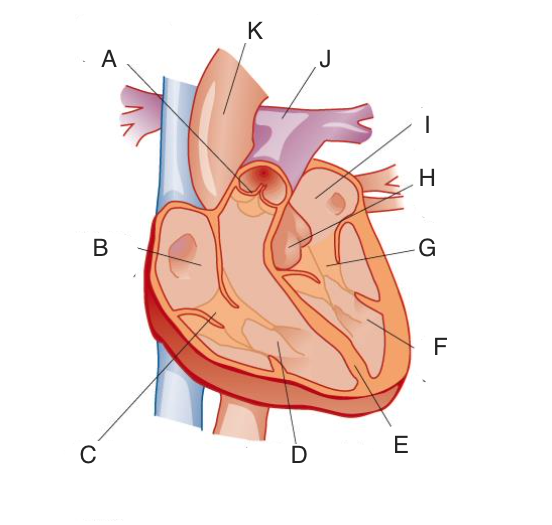
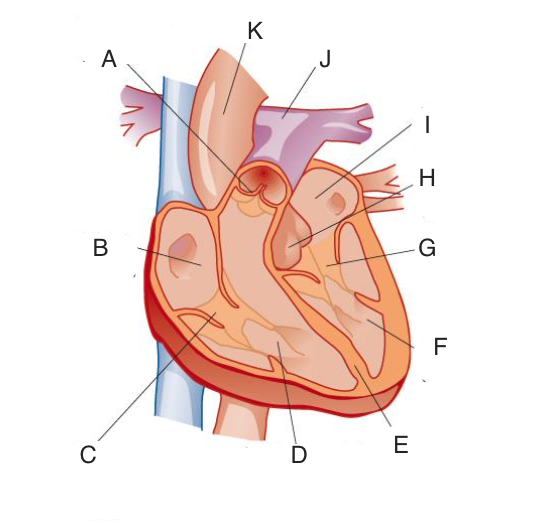
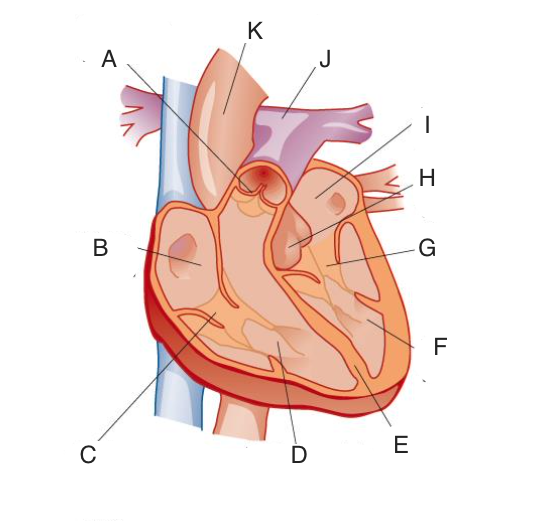
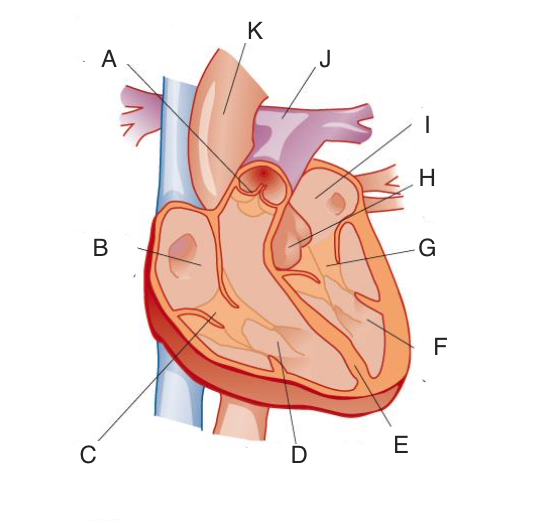
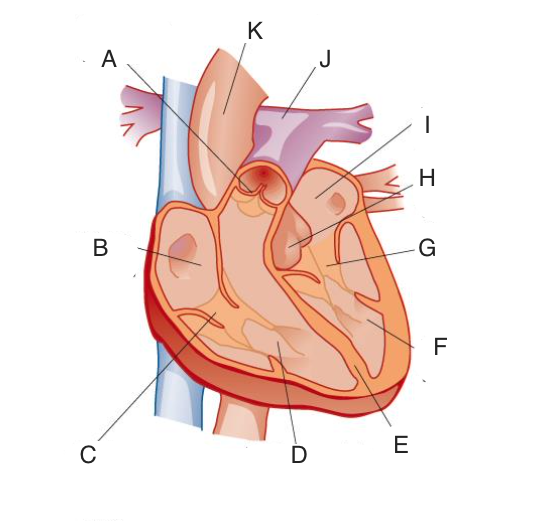
A,
13
New cards
right pulmonary vein
B,
14
New cards
right atrium
C,
15
New cards
inferior vena cava
D,
16
New cards
right ventricle
E,
17
New cards
Aorta
F,
18
New cards
left pulmonary vein
G,
19
New cards
left ventricle
H,
20
New cards
left pulmonary vein
I,
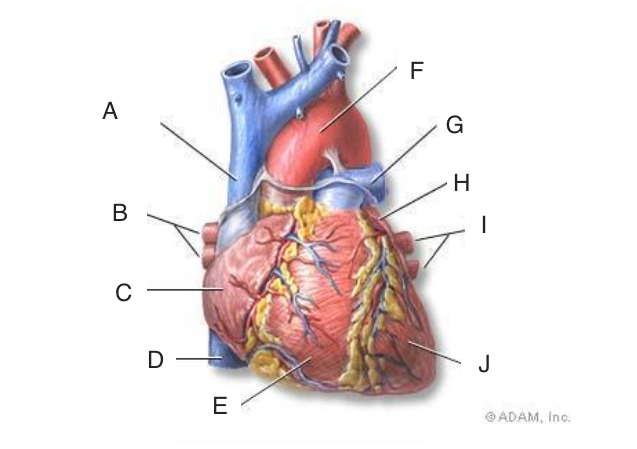
21
New cards
left ventricle
j,
22
New cards
A
semilunar valve
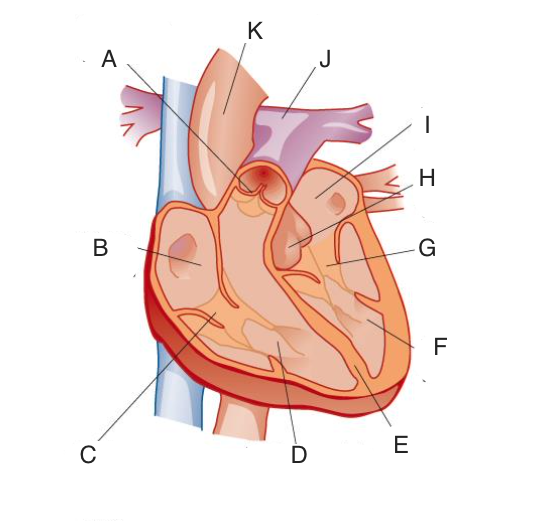
23
New cards
B
right atrium
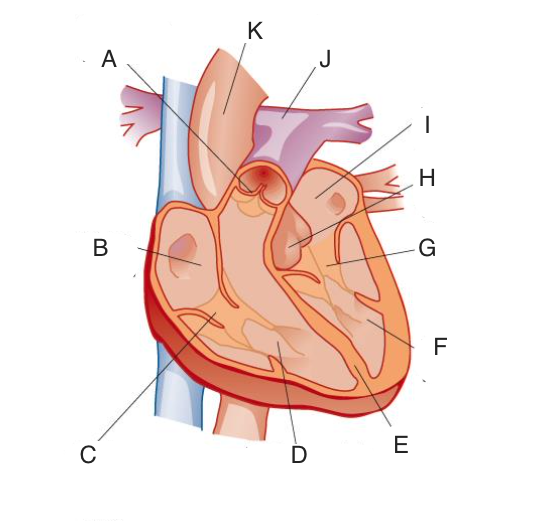
24
New cards
C
right atrioventricular valve which prevents back flow of blood form ventricle to the atria
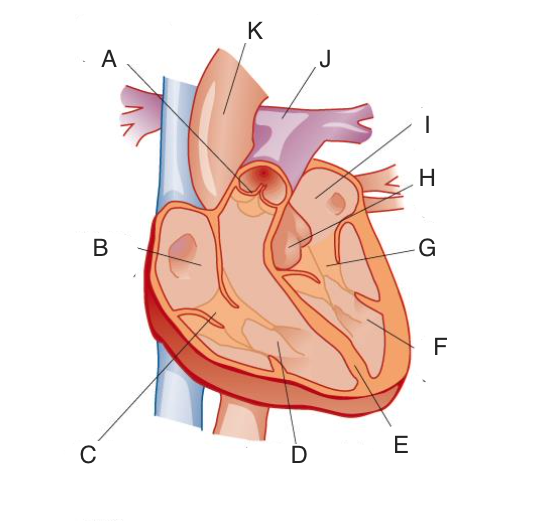
25
New cards
D
right ventricles
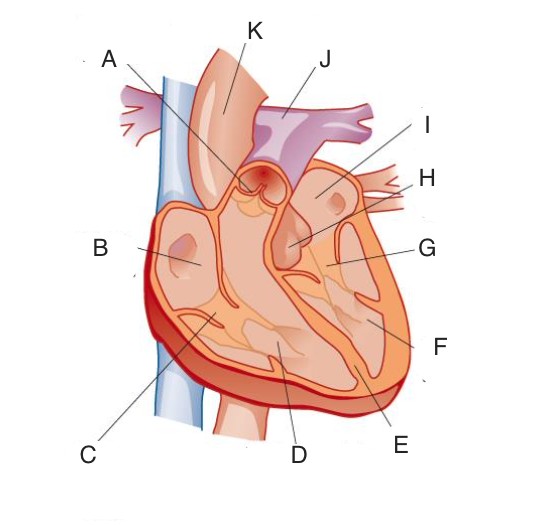
26
New cards
E
ventricular septum
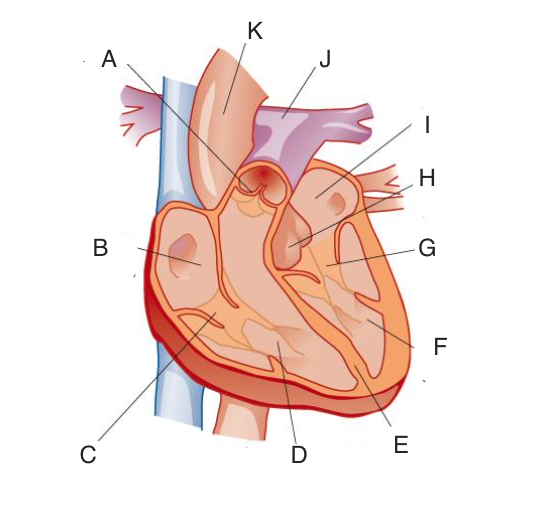
27
New cards
F
left ventricle
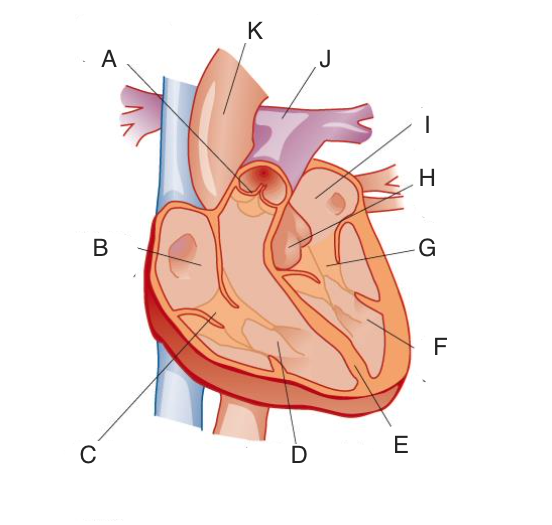
28
New cards
G
left atrio-ventricular valve
29
New cards
H
semilunar valve
30
New cards
I
left atrium
31
New cards
J
pulmonary artery
32
New cards
K
aorta
33
New cards
right ventricle to the left atrium
movement of blood in the heart via the lungs
34
New cards
left ventricle to the right atrium
movement of blood in the heart via the body
35
New cards
pulmonary artery to the pulmonary vein
blood vesicles the blood flows through from the heart to the the lungs and back
36
New cards
aorta to vena cava
blood vesicles the blood flows through from the heart to the the rest of the body and back
37
New cards
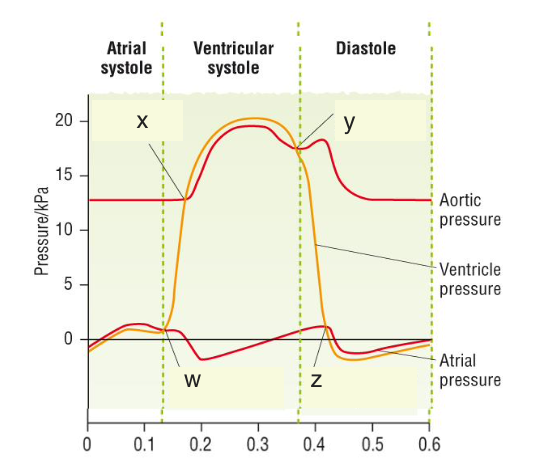
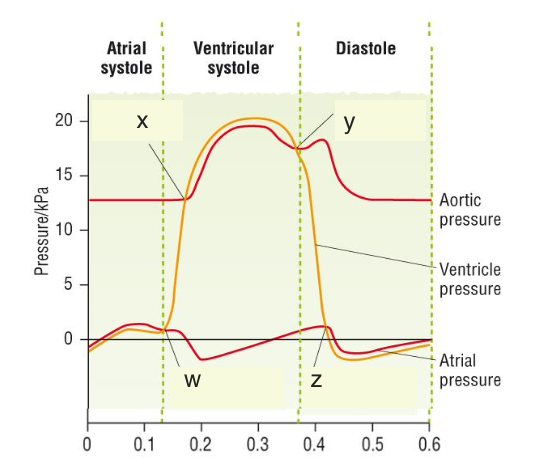
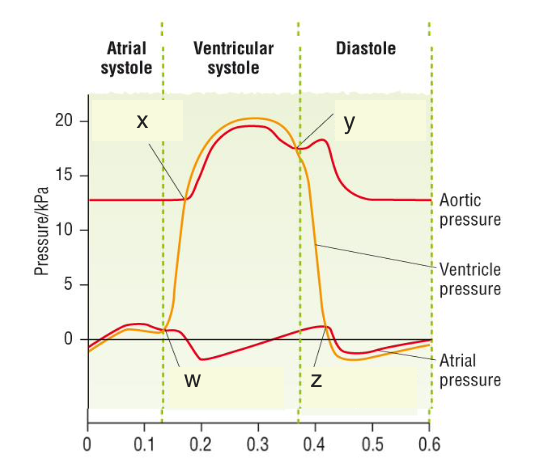
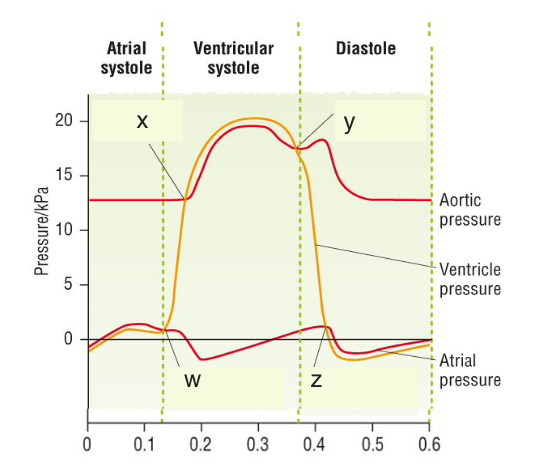
ventricular systole
ratio relax
ventricles relax to decrease volume and increase pressure, as pressure exceeds atria the atrioventricular valve close, making ‘lub’ noise
pressure continues to increase it exceeds pressure in arteries and opens semilunar valve and blood flows out
ventricles relax to decrease volume and increase pressure, as pressure exceeds atria the atrioventricular valve close, making ‘lub’ noise
pressure continues to increase it exceeds pressure in arteries and opens semilunar valve and blood flows out
38
New cards
atria systole
ventricles relaxed
atria wall muscles contract to push any last blood out in ventricle (atrial kick)
atria wall muscles contract to push any last blood out in ventricle (atrial kick)
39
New cards
diastole
both atria and ventricles relaxed
semilunar valves close ‘dub’ sound, prevents back flow of blood
atrioventricular valve open allowing atria and ventricles to passively fill with blood
semilunar valves close ‘dub’ sound, prevents back flow of blood
atrioventricular valve open allowing atria and ventricles to passively fill with blood
40
New cards
atrial systole, ventricular systole
order of cardiac cycle after diastole
41
New cards
Y
semilunar valve closes, as ventricle walls relax and pressure in ventricles drops below arteries, DUB sound
42
New cards
z
atrioventricular valve open, as both atrio and ventricle walls are relaxed so pressure of ventricle pressure falls below atrium
43
New cards
w
atrioventricular valve closes, as ventricle walls begin to contract increasing pressure in ventricles until it exceeds atrial pressure, cause LUB sound
44
New cards
x
semilunar valve opens, as pressure form ventricles exceeds pressies in aorta and pulmonary artery
45
New cards
atrial fibrillation
when atria start to contract out of time, contractions rapid and unsynchronised
46
New cards
atrial kick
topping up of the ventricles by contraction of muscle in walls of atria at end of diastole (ventricle receives 85% of blood from diastole and 15% from atrial systole but this increases with age)
47
New cards
elderly people
age where topping up of ventricles increases to closer to 35%
48
New cards
cardiac muscle
contains many mitochondria to produce ATP for contraction
49
New cards
myogenic
property of cardiac muscle where it doesn’t require nerve impulses from neurone to initiate contraction
50
New cards
control rate of contraction
by frequency of nerve impulses in accelerator and vagus nerves and by hormones like adrenaline
51
New cards
2, 5, 6, 1, 3, 7, 4, 8
order statements for coordination of heart action:
1. atrioventricular node (AVN) in septum between the atria, detects the electrical impulse
2. sinoatrial node (SAN) or pacemaker, in the wall of the right atrium, initiates the heart-beat
3. After a short delay (to allow atria to contract), the electrical / nerve impulse travels down the bundle of His (through Purkyne tissue) in the septum to the base of the ventricles
4. Both ventricle walls contract together from the bottom upwards so blood is pushed upwards and out of the heart
5. SAN initiates an electrical / nerve impulse that spreads across the walls of both atria causing them to contract together
6. A band of non-conducting collagen fibres prevents the random conduction of the electrical / nerve impulse to the ventricles
7. The Purkyne fibres branch from the bundle of His and transmit the electrical / nerve impulse to the muscle in the walls of the ventricles
8. Purkyne fibres also carry electrical / nerve impulse to the papillary muscles, which contract to keep the chordae tendinae taut and prevent the atrioventricular valves inverting
1. atrioventricular node (AVN) in septum between the atria, detects the electrical impulse
2. sinoatrial node (SAN) or pacemaker, in the wall of the right atrium, initiates the heart-beat
3. After a short delay (to allow atria to contract), the electrical / nerve impulse travels down the bundle of His (through Purkyne tissue) in the septum to the base of the ventricles
4. Both ventricle walls contract together from the bottom upwards so blood is pushed upwards and out of the heart
5. SAN initiates an electrical / nerve impulse that spreads across the walls of both atria causing them to contract together
6. A band of non-conducting collagen fibres prevents the random conduction of the electrical / nerve impulse to the ventricles
7. The Purkyne fibres branch from the bundle of His and transmit the electrical / nerve impulse to the muscle in the walls of the ventricles
8. Purkyne fibres also carry electrical / nerve impulse to the papillary muscles, which contract to keep the chordae tendinae taut and prevent the atrioventricular valves inverting
52
New cards
Coronary heart disease
when arteries carrying blood to the heart muscle become narrowed or blocked
53
New cards
low density lipoproteins
responsible for narrowing of artery lumen, contain cholesterol, deposited in artery wall underneath endothelium
54
New cards
atherosclerosis
process when low density lipoproteins (LDLs) are engulfed by macrophages, accumulating forming a fatty plaque called atheroma which narrows the artery
55
New cards
angina
sever chest pain from coronary heart disease
56
New cards
blood clot
formed from the atheroma breaking through endothelium, exposing collagen fires
57
New cards
heart attack
otherwise called a myocardial infraction, where a blood clot block the coronary artery, causes part of the tissue to be deprived of oxygen and dies, can cause death to individual
58
New cards
streptokinase
given intravenously to dissolve blood clots, it hydrolyses plasminogen to plasmin which breaks down fibrin and dissolves blood clots
59
New cards
stent
inserted to artery to widen lumen to treat coronary heart disease, inflated by a balloon when in place
60
New cards
diet
increase chance of CHD as high salt intake increase blood pressure, increased saturated fat/cholesterol intake increases its deposition in artery wall
61
New cards
hypertension
increases chance of CHD as it increases damage to endothelium in arteries and therefore increases chances of atheroma developing
62
New cards
exercise
decreases chance of CHD by lowering blood pressure, blood cholesterol and chance of developing obesity
63
New cards
smoking
increases chance of CHD by raising blood pressure, increasing atheroma formation and chance of blood clots
64
New cards
genetics
some ethnic gropes are at higher risk of CHD eg afro-caribbeans
65
New cards
male
one is more at risk of CHD until menopause when there the same
66
New cards
heart rate
number of beats per minute (bpm)
67
New cards
stroke volume
volume of blood pumped out of the left ventricle each cardiac cycle (typically 60-80cm3)
calculated by = volume at end of ventricular diastole - volume at end of ventricular systole
calculated by = volume at end of ventricular diastole - volume at end of ventricular systole
68
New cards
cardiac output
volume of blood pumped out left ventricle each minute (4-8dm3min-1)
calculated by stroke volume x heart rate
calculated by stroke volume x heart rate
69
New cards
ultrasound
able to measure volume of blood in left ventricle at 2 points in cardiac cycle, the end of ventricular diastole (most blood) and end of ventricular systole (least blood)
70
New cards
pulse rate
due to expansion of artery wall during ventricular systole and elastic recoil of artery wall as blood pressure drops during diastole
71
New cards
radial or carotid
artery in wrist and neck where pulse rate can be measured done for 15 seconds then multiplied
72
New cards
thumb
not used to measure heart rate as contains own pulse
73
New cards
age
effects heart rate as children have a faster heart rate
74
New cards
genetics
some people inherit a tendency to have a lower or higher heart rate or inherited diseases like cystic fibrosis
75
New cards
physical activity
heart rate increases in excursive and recovery, sustained her long term it can reduce heart rate as it becomes stronger
76
New cards
smoking
nicotine stimulates release of noradrenaline which increases heart rate
77
New cards
diet
eating fruit and veg is believed to be beneficial to heart rate
78
New cards
strenuous exercise
increase heart rate and stroke volume so therefore cardiac output
79
New cards
starlings law
during excursive blood Is returned to heart quicker as contracting muscle compresses veins
greater volume of blood enters ventricles during diastole stretching muscular walls of ventricles
cardiac muscle contracts more forcefully causing a greater volume of blood to be pumped out the heart
greater volume of blood enters ventricles during diastole stretching muscular walls of ventricles
cardiac muscle contracts more forcefully causing a greater volume of blood to be pumped out the heart
80
New cards
increases heart rate
due to more frequent nerve impulses along accelerator nerve to SAN
81
New cards
very high heart rate
decreases cardiac output as there is insufficient time for blood to enter ventricles during diastole so stroke volume decreases
82
New cards
training
used to achieve a lower resting heart rate as stroke volume and cardiac output increase due to stronger more efficient cardiac muscle
83
New cards
investigate heart rate
by measure pulse rate before and after exercise at a give intensity, evaluate data with a paired
t-test, at least 10 similar age participants, ensure no health conditions
t-test, at least 10 similar age participants, ensure no health conditions
84
New cards
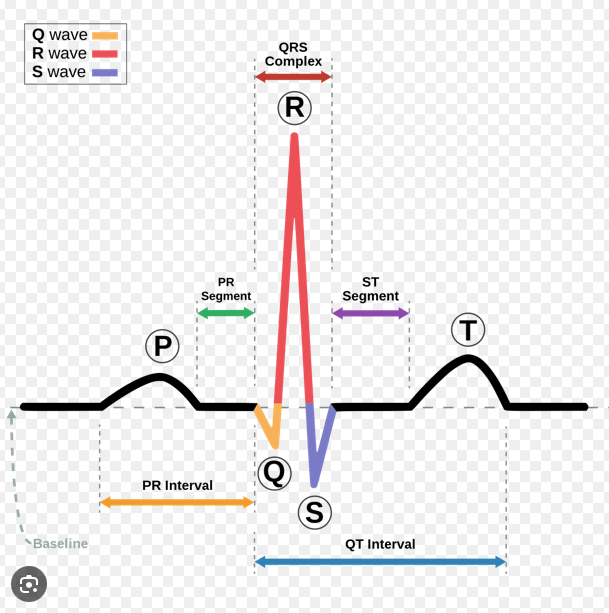
electrocardiography
shows changes in heart during cardiac cycle, displayed as an ECG
85
New cards
t wave
recovery from electrical activity in ventricles, atria and ventricles relax, small hump at end of ECG
86
New cards
QRS complex
detection of electrical impulse by AVN, transmission of impulse down septum and through ventricle walls that then contract, 2 dips and a big peak on ECG
87
New cards
p wave
spread of electrical impulse from SAN through atrial walls that then contract, small hump at start of ECG
88
New cards
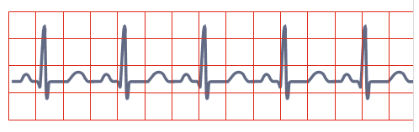
bradycardia
very slow resting heart rate (40-60bpm) gap between each peak in race is long, causing a long gap between T wave and P wave
89
New cards
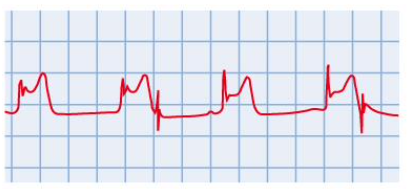
tachycardia
high resting heart rate (above 100bpm) ECG shows little gap between one t wave and next p wave
90
New cards
heart attack
blood supply to part of heart muscle is blocked trough and peaks become less distinct and not as regular, S-T portion of ECG is higher (S-T elevation)
91
New cards
atrial fibrillation
wall of atria contract in unsynchronised manner that prevents filling of ventricles, unclear p wave

92
New cards
heart attack symptoms
heavy crushing pressure in chest spreading to jaw, neck and arm s
breathlessness, discomfort in stomach, profuse sweating, cold ashen looking skin, blue lips
rapid, weak irregular pulse, nausea, vomiting and unexpected collapse
breathlessness, discomfort in stomach, profuse sweating, cold ashen looking skin, blue lips
rapid, weak irregular pulse, nausea, vomiting and unexpected collapse
93
New cards
4, 1, 5, 3, 2,
number statements for treatment of heart attack
1. Sit the person in **W** position (sitting up with knees bent)
2. Reassure and monitor breathing rate / pulse rate until help arrives
3. Assist patient with any personal medication for angina (tablets or spray)
4. Call 999 and tell them you suspect heart attack
5. Give them 300mg aspirin tablet if available (check allergy, must be over 16)
1. Sit the person in **W** position (sitting up with knees bent)
2. Reassure and monitor breathing rate / pulse rate until help arrives
3. Assist patient with any personal medication for angina (tablets or spray)
4. Call 999 and tell them you suspect heart attack
5. Give them 300mg aspirin tablet if available (check allergy, must be over 16)
94
New cards
cardiac arrest
when the heart is no longer performing any useful function to circulate blood around the body, either ventricular fabulation (no effective movement of blood out heart) or atrial fibrillation (insufficient filling of ventricles)
95
New cards
treat cardiac arrest
lie down and perform CPR until emergency services arrive, a trained first aider can use a defibrillator to shock the heart out of fibrillation
96
New cards
6, 3, 8, 7, 9, 1, 2, 4, 8
order the process of CPR:
1. After each compression release all the pressure on the chest without losing contract between the hands and the sternum
2. Aim for a rate of about 100 compressions per minute (count out loud)
3. Check for breathing by tilting the head backwards
4. Do 30 compressions then give mouth-to-mouth resuscitation, also known as Expired Air Resuscitation (EAR), twice
5. Continue 30:2 procedure until help arrives
6. Immediately ring for help, don’t leave patient and constantly reassure them
7. Keep your elbows straight and press down vertically, bring your bodyweight over your hands to make it easier
8. Place heel of one hand in the centre of the victim’s chest and heel of the other hand on top of the first interlocking your fingers together.
9. Press down firmly and quickly to about 4 to 5 cm downwards, relax and then repeat the compression.
1. After each compression release all the pressure on the chest without losing contract between the hands and the sternum
2. Aim for a rate of about 100 compressions per minute (count out loud)
3. Check for breathing by tilting the head backwards
4. Do 30 compressions then give mouth-to-mouth resuscitation, also known as Expired Air Resuscitation (EAR), twice
5. Continue 30:2 procedure until help arrives
6. Immediately ring for help, don’t leave patient and constantly reassure them
7. Keep your elbows straight and press down vertically, bring your bodyweight over your hands to make it easier
8. Place heel of one hand in the centre of the victim’s chest and heel of the other hand on top of the first interlocking your fingers together.
9. Press down firmly and quickly to about 4 to 5 cm downwards, relax and then repeat the compression.
97
New cards
expired air resuscitation
process of; laying erosion on back, tilting their head back and lift their chin, gently pinch soft part of nose closed, open mount keeping chin lifted, take a deep breath and place lips around person mouth, (get a good seal), breath out and watch chest rise and fall and repeat
98
New cards
defibrillator use
place the two pads on chest in a diagonal line with the heart in the middle, machine reading will show if heart is fibrillating, an electric shock is applied to momentarily to stop chaotic electrical activity and heart can recover coordinated rhythm