1.02 Non-Medical Sciences
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
What is the sick role?
-refers to the set of rights and obligations surrounding illness that could shape the behaviour of doctors and patients
Explain the importance of the sick role (2)
-allows individuals temporary exemption from their ordinary role obligations
-provides the mechanism for returning people to health and therefore to their normal role performance
What is a potential problem with the sick role?
-the sick role may become an attractive alternative to everyday pressures, providing a way of 'evading social responsibilities' and offering 'secondary gain' (interpersonal or social advantage attained by the patient as a consequence of the illness)
What are the rights and responsibilities of the sick role? (4)
-Rights: exempted from normal social roles e.g. work/family, is not responsible for their conditon
-Obligations: should try to get well, seek techinically competent help and cooperate with medical professionals
What are the limitations of the sick role in modern society? (6)
-now the unwell usually continue completely as normal in their jobs and social lives
-less clear about who's responsible for adopting the sick role
-patients will also be self-managing for most of their illness; requirement that they must seek + submit to medical care is looking unsound
-instead of wanting to get better (impossible in many chronic diseases), patients are more concerned w/ avoiding the sick role completely
-many illnesses e.g. arthritis, diabetes & asthma may never improve
-sick role may be rejected for illnesses that are poorly defined or not widely accepted as valid e.g. chronic migraine
What is qualitative research? (2)
-involves the application of logical, planned and thorough methods of collectiving data and careful/thoughtful analysis
-a way of doing research w/o counting because it doesn't set out to quantify or enumerate the social world or phenomena studied
Is qualitative research devoid of measurement or explanation?
-no, although qualitative research generally deals w/ speech, actions, and texts rather than numbers, you can analyse certain types of qualitative data quantitatively so qualitative analysis can offer profound and rich insights about aspects of health care and services that prove elusive to quantitative research
Give examples of qualitative approaches (2)
-if quantitative research asks 'how big is X or how many Xs are there?', qualitative research tackles questions such as 'what is X, and how do people's perceptions of X vary in different circumstances and why?'
-instead of counting the no. of suicides, which persumes that we already agree on the nature of suicide, the qualitative researcher many start by asking, 'what is suicide and how is it defined in this society?'
What is one of the key features of qualitative research?
-particularly suited to studying people in their day-to-day settings rather than in experimental or artificial ones
Outline the different qualitative methods of data collection (8)
-observing people in their own territory (non-participant observation)
-joining in (participant observation)
-talking to people (interviews, focus groups and informal chatting)
-reading what people have written (documentary analysis)
-examining objects, images and artefacts people create or use
-speech or behaviour can be collected using audio or video tapes
-textual analysis has been extended to include online conversations, forum threads and printed documents
-different qualitative methods can be combined to provide deeper insights
Outline the use of qualitative methods (5)
-qual. + quan. research can be used together-> insights provided by qual. research help to interpret/understand quan. data more fully
-can be used independently to uncover social processes
-especially valuable for understanding views and opinions eg. Morgan and Watkin's research on people's cultural beliefs on hypertension has helped to explain why rates of compliance w/prescribed medication vary significantly among and between white + afro-caribbean patients in south london
-provides rich detail about life and behaviours inside healthcare settings
-qual. methods are increasingly being used in studies of health service organisation and policy
What is a disadvantage of qualitative research?
-considerable skill is required by the researcher
What is a problem-focused approach to dealing with stress?
-targets the causes of stress in practical ways, tackles problem or stressful situation
Give examples of problem-focused approaches (3)
-problem-solving
-time-management
-instrumental social support
What are the advantages of a problem-focused approach? (2)
-provides a long term solution
-deals w/ root of the problem
When is a problem-focused approach not appropriate? (2)
-in some cases i.e. death -> emotion-support is a better approach
-doesn't work when it is beyond the person's control to remove the stress e.g. exams, work based stressors
What is an emotion-focused approach to dealing with stress? (2)
-often called palliative coping
-attempts to decrease emotional responses such as embarassment, fear or depression
Give examples of emotion-focused approaches (6)
-drugs that control emotion
-prayer
-meditation
-drugs/alcohol
-distraction
-relaxation
What are the advantages of an emotion-focused approach? (2)
-can be an effective way of managing brief clinical challenges e.g. minor invasive procedures
-certain types of palliative coping are important in adjusting to the longer-term challenge of chronic disease e.g. seeing onself as better off than other people -> downward social comparison might help w/ emotional adjustment
What is a potential problem with an emotion-focused approach?
-can also include psychological defence mechanisms which can include potentially destructive responses such as venting frustration on other people or becoming angry w/ other people + can include denial
What is mortality rate?
-a measure of the frequency of death in a defined population during a specified interval
What must be specified in any mortality rate?
-time must be specified in any mortality rate
Write down the calculation that would be required to determine the annual all-cause mortality rate per 1000 population
No. of deaths from all causes in 1 year/number of people in the population at mid year (because population changes over time) x 1000
Write down the calculation that would be required to determine the annual mortality rate per 1000 population for adults 30-40 years of age
No. of deaths from all causes in 1 year in adults 30-40 years of age/ no. of 30-40 year olds at mid year x1000
Write down the calculation that would be required for annual mortality rate per 1000 from heart disease
No. of deaths from heart disease/no. Of people in the population at mid year x1000
Write down the calculation that would be required for the annual mortality (per 1000 population) from heart disease in adults 30-40
No. of deaths from heart disease in people 30-40 in 1 year/no. Of 30-40 year olds at mid year x1000
What is case-fatality rate?
-proportion of people who have a disease and who are dying from it in a specified time period
What is case-fatality a measure of?
-disease severity
What would be the calculation for determining the case fatality rate in heart disease patients?
No. of deaths during a specific time period after heart disease onset or diagnosis/ no. of people with heart disease in that specific period
What can case-fatality be useful in measuring?
-the benefits of a new drug or intervention
What is a potential limitation of the numerator (case-fatality)?
-numerator should be restricted to deaths from that disease though it is not always easy to distinguish between deaths from that disease and other causes
What should ideally be used as the beginning of a specified time period and why is this not always feasible? (case-fatality)
-the date of disease onset should be the beginning of the specified time period but date of disease onset is often hard to standardise since many diseases develop insidiously (without symptoms) over a long period of time -> more often, the date of disease diagnosis is used
What is proportionate mortality?(2)
-provides a quick look at relative contribution of the different causes of death
-by itself, it is not a measure of risk -> you need to know total mortality rate
Write the calculation that would be used to determine the proportionate mortality of heart disease
No. of deaths from heart disease/total deaths x 100
Outline what a cohort study is (2)
-compare exposed and unexposed people
-we compare the incidence of disease in exposed and unexposed individuals
What are the advantages of carrying out a cohort study? (3)
-desirable when the exposure of interest is rare -> in a case-control study we are unlikely to identify a sufficient no. of exposed people when we are dealing with a rare exposure
-incidence in both exposed and unexposed groups can be calculated so we can directly calculate relative risk
-time sequence can be calculated
What are the disadvantages of carrying out a cohort study? (4)
-usually require large populations
-greater potential bias for assessing the outcome is present in comparison to case-control studies
-becomes impractical when the disease under study is rare
-high cost
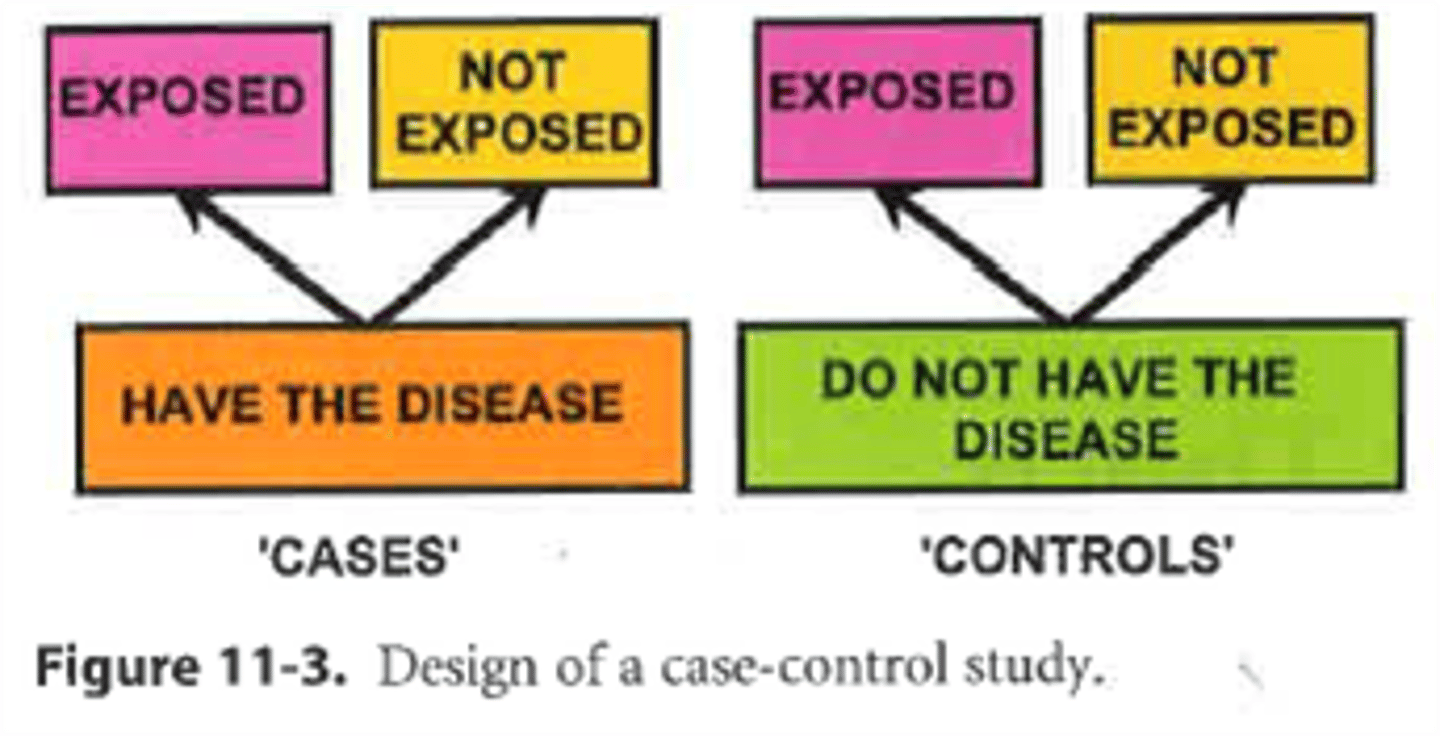
Outline what a case-control study is? (2)
-people with the disease (cases) and without the disease (controls) are compared
-we compare the proportions exposed in people with the disease and in people without the disease
What are the advantages of a case-control study? (4)
-relatively inexpensive
-require a relatively small no. of subjects for study
-desirable when disease occurrence is rare- if a cohort study were performed in such a circumstance, a tremendous no. of people would have to be followed to generate enough people with the disease for study
-we begin with cases and controls so we can study more than one possible etiologic factor and we can explore interactions among the factors
What are the disadvantages of a case-control study?
-often require data about past events or exposures
-selection of an appropriate control group is difficult
-in most case-control studies we can't calculate disease incidence in either the total population or the exposed and unexposed groups without supplemental information
What is a cross-sectional study design?
-takes a selected population and measures health information in a given point in time, giving you a snapshot of their health
What does a cross-sectional study usually involve? Example?
-usually involves asking participants a series of questions using a questionnaire eg. health surveys that collect health information about people in a population
Why is a cross-sectional study also called a prevalence study?
-it often measures how many people have a disease at a particular point in time
What is it important to ensure regarding the selected population in a cross-sectional study?
-that the selected population is representative of the total population
What are the advantages of cross-sectional studies? (3)
-data on both exposure and disease outcomes are collected simultaneously from each subject
-relatively inexpensive
-assesses health needs
What is a disadvantage of carrying out a cross-sectional study?
-information is collected at a single point in time so it can't be used to determine whether a particular exposure caused the disease or not
What is an audit?
-measures current practice against defined standards
Why do health professionals use clinical audits?
-to assess, evaluate and improve care of patients in a systematic way
What does clinical audit form part of?
-clinical governance which aims to ensure patients receive best quality of care
What can audits assess? (3)
-structure of care eg. presence of a dedicated stroke unit
-process of care eg. waiting times in clinic
-outcome of care eg. blood pressure reduction is response to therapy
Why do doctors have to carry out audits? (2)
-GMC states that doctors are required to take part and respond constructively to audits
-doctors in the UK are asked to perform an audit during their first two post graduate years
Outline the stages of an audit (5)
-Preparing an audit: clinical team has to prioritise topics in terms of high volume of work, high risks and high cost of care. Also have patients recommended topics + is good evidence available to inform standards?
-selecting criteria for audit review: use recommendations from clinical practice guidelines
-measuring level of performance: collect data, compare performance with criteria, conclude how well standards were met/ if not then why
-making improvements: implement change
-sustaining improvements: repeat audit, discuss results+ agree on recommendations for change with rest of team. If improvements are sustained, some form of monitoring should replace a full audit. If performance deteriorates then full audit should be reactivated.
What is the purpose of the NHS values?
-provides framework to guide everything we do within the NHS
Where were the NHS values derived from?
-from extensive conversations with staff, patients and the public
Outline the NHS values (6)
-working together for patients: patients come first
-compassion: respond with humanity and kindness to each person's pain, distress, anxiety or need
-commitment to quality of care
-respect and dignity: value each person as an individual, understand their priorities and needs
-improving lives: strive to improve health and wellbeing + people's experiences of the NHS
-everyone counts: maximise resources for the benefit of the whole community and make sure no one is excluded, discriminated against or left behind
What is the NHS constitution? (3)
-published by department of health in 2011
-first document in the history of the NHS to set out what patients, the public and staff can expect from the NHS and what the NHS expects from them in return
-cannot be altered by the government without full involvement of staff, patients+ the public -> protects NHS against political change
Outline the changes implemented by the Health & Social Care act 2012 (5)
- a move to clinically led comissioning: CCGs now control most of NHS budget
-an increase in patient involvement in the NHS: Healthwatch ensures voice of consumer is strengthened and heard
-a renewed focus on the importance of public health: PHE (public health england) was created
-a streamlining of 'arms-length' bodies: act conferred additional responsibility on NICE to develop guidance and set quality standards for social care + HSCIC (health and social care information centre) for collecting, analysing and presenting national health & social care data
-allowing healthcare market competition in the best interest of patients: allow fair competition for NHS funding to independent, charity & third-sector healthcare providers to give greater choice and control to patients
What is the Department of health?
-government department responsible for funding and coming up w/ policies to do w/ healthcare in the UK
What is NHS England?
-Umbrella body that oversees healthcare. Independent body so department of health can't interfere directly w/ its decisions
What are CCGs? (3)
-Clinical commissioning groups
-responsible for comissioning healthcare for their local area
-run by GPs, nurses + consultants who assess local healthcare needs & comission the services to meet them -> in charge of 60% of the NHS budget
What are NHS foundation trusts?
-provide the care that the CCGs commission
eg. hospital, ambulance, mental health, social health & primary care services
What is private healthcare?
-made up of hospitals and clinics which are run independently of the NHS -> normally run by a commercial company, although some may be run by charities or other non-profit organisations
What are the two types of private healthcare? (2)
-Type 1: patients pay for healthcare directly or through private health insurance
-Type 2: healthcare remains public but services are outsourced to private firms
Compare private and public healthcare in terms of the following: waiting times, choice, comfort, breadth, cost
-waiting times: priv. lower for referrals so seen faster and receive treatment more promptly; pub. can take 2 weeks or longer to see a GP
-choice: priv. more choice of hospitals, consultants, and GPs; people have 'right to choose' but not as much about: who treats them, where they're treated + when
-comfort: priv. nicer facilities
-breadth: priv. not as wide a range of treatments covered-> depends on insurance, some niche drugs are only available privately; pub. better breadth of care + wider range of conditions treated
-cost: priv. very suitable + not suitable for emergencies; pub. free at the point of access
What are the ethical implications of private healthcare? (positive) (3)
-eases burden on NHS if patients go private- reduces waiting times so other patients can be seen, quicker recovery and increase in QoL sooner -> justice + beneficence
-heavily regulated- no queue jumping and most doctors don't comprimise ethics
-better working conditions, employment benefits and financial benefits which increases doctors' morale and increases standards of patient care and safety
What are the ethical implications of private healthcare? (negative) (3)
-only wealthy can afford private healthcare -> disadvantaging vulnerable people
-can be argued that private healthcare is financially driven rather than altruistic -> may result in a commerical doctor-patient relationship which can result in harm-> doctors may recommend unnecessary examinations to receive more money -> non-maleficence
-reduces time given to NHS if consultants ae working in the private sector to supplement their income eg. may leave an NHS clinic early to get to a private clinic
Outline what the GMC says regarding maintaining boundaries w/ patients: doctor-patient relationship
-patients should be able to trust that doctors will behave professionally during consultations and will not see them as a potential sexual partner
Outline what the GMC says regarding maintaining boundaries w/ patients: current patients
-doctors must not pursue a sexual/improper emotional relationship w/ a current patient; if a patient tries to treat them politely and considerately and try to re-establish a professional boundary + if necessary to end professional relationship, follow guidance available
-you must not end a professional relationship w/ a patient solely to pursue a relationship w/them
Outline what the GMC says regarding maintaining boundaries w/ patients: former patients
-personal relationships w/ former patient: docs may be inappropriate depending on factors such as: the length of time since the professional relationship ended, nature of previous professional relationship, vulnerability at time of professional relationship + now, whether you are still caring for other members of the patient's family
Outline what the GMC says regarding maintaining boundaries w/ patients: timing
-timing: not possible to specify length of time after which it would be acceptable to begin a relationship w/ a former patient, duration of professional relationship may be relevant eg. relationship w/ a patient you treated over a no. of years more inapprop. than patient from a single consultation
Outline what the GMC says regarding maintaining boundaries w/ patients: vulnerable patients (2)
-more vulnerable patient= incr. likelihood of relationship being an abuse of power eg. if you're a psychiatrist or a paediatrician
-whatever specialty-> do not pursue a relationship if former patient is still vulnerable, if was but isn't anymore ensure patient's decisions aren't influenced by previous relationship w/ you and you're not/ couldn't be seen to be abusing your professional position
Outline the GMC guidelines regarding the use of social media (6)
-privacy: patients, your employer + potential employers may able to access your personal info
-benefits: can enagage people in public health + policy discussions, can be used to establish national and professional networks, can help patients access info about health and services
-maintaining boundaries: if patient consults you about professional matters you have to inform them that you can't mix social and professional relationships
-maintaining confidentiality: don't discuss individual patients or their care, don't care identifiable information about patients n professional social media sites
-respect for colleagues: don't bully/ harass people online
-anonymity: if you identify yourself as a doctor in publicly accessible social media, also identify yourself by your name
Describe the concept of duty of care (2)
-duty of care is defined simply as a legal obligation to:
always act in the best interest of individuals and others
not act or fail to act in a way that results in harm
act within your competence and not take on anything you do not believe you can safely do
-seeing a patient once, may or may not provide HCPs w/ sense of ongoing duty of care -> transitory
-when a therapeautic
What are some constraints to beneficence? (3)
-the need to respect the autonomy of those whom one intends to help ie. what he or she actually wants one to do
-duty of beneficence needs to be tempered by the duty of non-maleficence
-duty of beneficence needs to be tempered by the duty of justice e.g. if a patient ants an expensive drug when there's a cheaper one that's just as effective
What were the lay perceptions of hospitals in the past? (3)
- a place that was trusted to make you better
-highly-appreciated - almost a refuge
-something seen as a luxury- you needed to be able to afford it before the NHS
-a place of being told what to do + order- matrons ran wards + were v. strict
What were the lay perceptions of HCPs in the past? (2)
-HCPs were "the keeper of knowledge" + highly respected
-opinions and decisions were never questioned- God's involvement
What are the lay perceptions of hospitals now? (4)
-place that creates fear and anxiety- what will I contract in hospitals? corona virus, MRSA
-still a place of refuge- get free meals + looked after (elderly in particular)
-a human right - based on clinical need and not the ability to pay
-a place of chaos and uncertainty
What are the lay perceptions of HCPs now? (2)
-still highly respected however, they are not the "keepers of knowledge" due to patients ability to google, people are generally more informed etc.
-can be questioned if not trusted eg. can ask for second opinions + refuse advice