Dermatology unito until 26/05
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
Which gene is most frequently associated with Acral Lentiginous Melanoma? (explain relevance in 1 sentence)
c-KIT gene. Treatment implication: targeted by Imatinib
List the most important drugs in treatment of metastatic melanoma
Tyrosine kinase inhibitors
BRAF/MEK inhibitors
c-KIT inhibitors
Immune checkpoint inhibitors
anti-CTLA4 monoclonal antibodies
anti-PD1 monoclonal antibodies
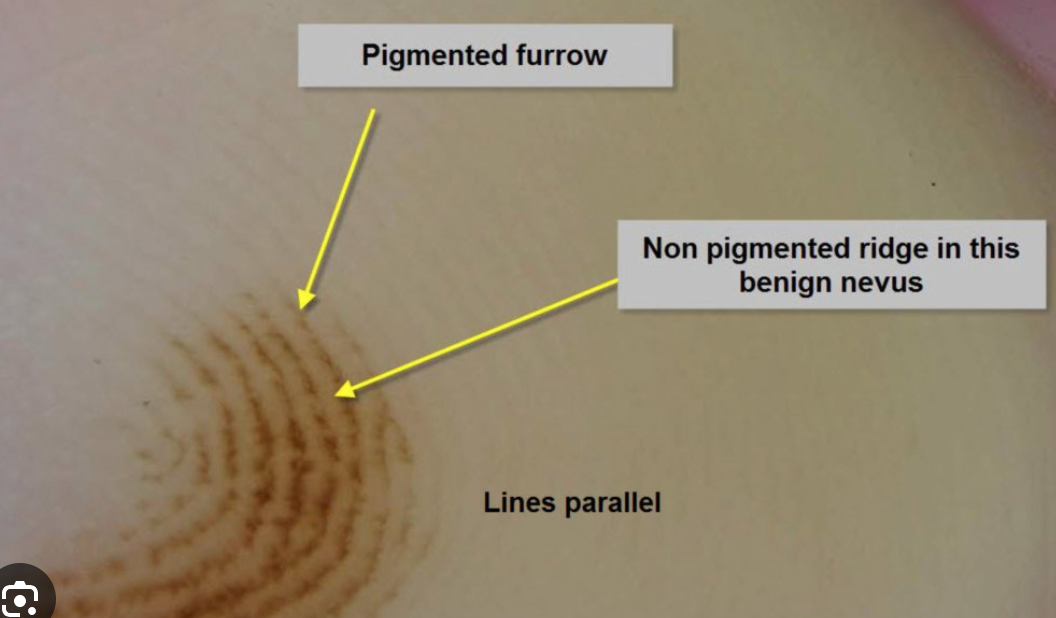
What are the typical dermoscopy features that enable us to distinguish between acral melanoma and acral nevus?
The presence of parallel ridge pattern (pigmentation on the ridges of acral skin) is a hallmark of acral melanoma
Explain the clinical progression to lentigo maligna melanoma
Chronic UV-radiation exposure leads to Lentigo Maligna (precursor/in situ lesion in the horizontal growth phase) presenting as a macula with suspicious features (ABCDE, ugly duckling sign, etc.) generally on the face, scalp and ears. When not excised, it progresses in 90-95% of cases to Lentigo Maligna Melanoma (invasive melanoma in vertical growth phase) typically presenting as a dark nodule over the macula.
Explain when Mohs micrographic surgery is preferred for treatment of basal cell carcinoma
Mohs micrographic surgery is preferred in the treatment of BCC in these cases:
Tumor is located in high-risk or cosmetic sensitive area (e.g. face, nose, eylids, ears)
Recurrent lesion
Aggressive histological subtype (morpheaform, infiltrative)
Poorly defined margins.
It gives the highest cure rate with maximal tissue preservation.
Which are the most common sites of seborrheic dermatitis and why?
The most common sites are:
Sternal area
Scalp
Face (forehead, paranasal/nasolabial region, chin, eyebrows, eyelids, jaw, beard area)
The reason is that in these regions there is a higher quantity of sebaceous glands.

List and define what are the key histopathological features of the dermis and epidermis in psoriasis
DERMIS:
Dilation of blood vessels
Lymphocyte infiltration
EPIDERMIS:
Parakeratosis: thickening of the stratum corneum with presence of nucleated cells
Munro’s microabscesses: abscesses in the stratum corneum of the epidermis due to infiltration of neutrophils from the papillary dermis into the stratum corneum
Pustules of Kogoy: sterile collections of neutrophils in the stratum spinosum
Acanthosis: thickening of the whole epidermis
Hypogranulosis: decreased or absent granular layer in the epidermis
List the endogenous risk factors of melanoma (7)
MC1R gene variations
Germline mitations (CDKN2A, CK4)
Personal or family history
Individual with numerous nevi
Presence of atypical nevi
Congenital melanocytic nevus >20cm
Fair skin phototypes
List the exogenous risk factors of melanoma
Chronic UV radiaiton exposure
Sunburns
Artificial UV sources
Geographical and environmental factors
Iatrogenic immunosuppression (e.g. organ-transplant patients)
List the treatment used in actinic keratosis: those indicated for single lesions and those used for field cancerization.
TREATMENT FOR SINGLE LESIONS:
Cryotherapy
Curettage and cautery
Laser therapy
FOR FIELD CANCERIZATION:
Photodynamic therapy
Topical treatments, including
5-Fluorouracil (cream formulations, sometimes combined with salicylic acid)
Imiquimod
Diclofenac
Tirbanibulin
Define Kaposi sarcoma and list the types
Kaposi sarcoma is a low-grade angioproliferative tumor mainly associated with HHV-8 infection.
Classic Kaposi sarcoma
Endemic (African) Kaposi sarcoma
Epidemic (AIDS-related) Kaposi sarcoma
Iatrogenic (transplant-related) Kaposi sarcoma
What is the most important and quickest step in the diagnosis of gonorrhea?
Gram stain detects the gram-negative diplococci in urethral discharge.

What is the treatment of pubic lice?
Permetrhrin 1% cream or lotion
Benzyl benzoate (25% in oily solution)
Shaving
List at least 3 cutaneous diseases associated with type II hypersensitivity reactions
1) Pemphigus Vulgaris
2) Bullous Pemphigoid
3) Dermatitis Herpetiformis of Duhring
Clinical Case: A 58‐year‐old male with a history of mild hypertension and recently unexplained weight loss of 10 pounds over 2 months presents to the dermatology clinic with severe, painful oral erosions that have progressively worsened over the past month. The patient initially noticed persistent soreness and ulcerations on his buccal mucosa and tongue, which made eating and speaking difficult. Soon after, he developed polymorphous skin lesions that varied in appearance—ranging from flaccid bullae to erosive patches and papules with a lichenoid quality—distributed over his trunk, axillae, and extremities. Nikolsky sign is positive. He also recently has had trouble breathing. What is the most likely diagnosis?
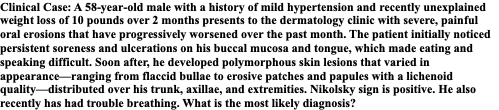
PARANEOPLASTIC PEMPHIGUS
What kind of treatments can be used for scarring management?
Peels
Microneedling
Laser therapy
Laser therapy + lipofiller
Punch excision
What are some of the pathologies that go in differential diagnosis with Erythematotelangiectatic Rosacea?
SLE
Acne Vulgaris
Contact dermatitis
Seborrheic dermatitis
Carcinoid syndrome
Photodermatitis
Define onycholysis and list 3 causes
Onycholysis is the separation of the nail bed from the nail plate.
Psoriasis
Repetitive trauma
Onychomycosis
What is the difference between true and apparent leukonychia?
In apparent leukonychia the whitish discoloration of the nail does not move with nail growth towards the free edge of the nail, while in true leukonychia it does.
Describe the timing of patch test and the crescendo reaction
The patch test is put on the patient at time zero. After 48h, it is taken off the patient and a first reading is done. If there are doubts, a second reading is done after 72h.
The crescendo reaction is the progressively intensifying skin reaction at the site of the test over time.
Which is the target of Dupilumab?
Dupilumab is a monoclonal antibody that targets the alpha subunit of IL-4 and IL-13 receptors.
Which are the criteria for the diagnosis of atopic dermatitis?
The criteria of atopic dermatitis are those proposed by Hanifin and Rajka in 1980 and include major and minor criteria. A diagnosis of atopic dermatitis is made when 3 or more of the four major criteria and 3 or more of the minor criteria are met.
The major criteria (4) are:
Pruritus,
Typical morphology and distribution
Chronic or chronically relapsing dermatitis
Personal/family history of atopy.
The minor criteria:
Xerosis,
Ichthyosis,
Keratosis pilaris,
Palmar hyperlinearity,
Positive skin prick test,
Elevated serum IgE,
Early age of onset,
Increased risk of infection,
Risk of non-specific hand or foot dermatitis,
Nipple eczema,
Cheilitis,————
Pityriasis alba
Recurrent conjunctivitis,
Dennle-Morgan infraorbital folds,
Orbital darkening
Increased risk of developing cataracts.
Wool intolerance,
Food intolerance,
Exacerbation by environmental or emotional stress,
White dermographism,
Anterior neck folds,
Facial pallor or erythema,

List 5 pathophysiological mechanisms leading to blister formation
1. Spongiosis
2. Acantholysis
3. Cytolysis
4. Subepidermal blister formation
5. Mechanical blister formation

Name at least 2 microbial cofactors in acne rosacea
Demodex folliculorum; Helicobacter pylori

Name the two most commonly used Severity Score indices for psoriasis
PASI (Psoriasis Area Severity Index) and BSA (Body Surface Area)
What are the main risk factors for developing cutaneous squamous cell carcinoma?
1. Chronic UV exposure
2. Fair skin (Fitzpatrick 1 and 2)
3. HPV infection (16 and 18)
4. Immunosuppression (e.g. organ-transplanted patients)
5. Chronic wounds or scars (Marjolin ulcer)
6. Tobacco and alcohol use
7. Arsenic exposure
8. Genetic disorders (e.g. xeroderma pigmentosum).
Which are the topical antifungals used in seborrheic dermatitis?
Ketoconazole and ciclopirox
A 17-year-old boy presents with a 6-month history of small, itchy wheals appearing within minutes of exercise or hot showers. They resolve within an hour. He occasionally feels flushed and lightheaded during episodes. What is the most likely diagnosis, and how would you confirm it?
Cholinergic urticaria; clinical observation and provocation tests.

Give the 2 main nail signs of psoriasis
Onycholysis; Irregular pitting.

What are the worst complications in women affected by Chlamydia?
Urogenital complications, meaning pelvic inflammatory diseases which lead to ectopic pregnancies, chronic pelvic pain and infertility.
30-year-old man has recurrent blistering lesions located on both elbows and knees, persistent for around 2 years. He has T1DM and autoimmune thyroiditis. He hates hospitals since his childhood diagnosis of diabetes, and avoids medical facilities unless absolutely necessary. He sought medical attention due to intense pruritus which was intolerable and which is significantly affecting his daily activities. Family history: his grandfather was probably diagnosed with lymphoma (though the patient is unsure of the specific type). On examination, he appears pale, of short stature, and has a lean build. Nikolsky sign is negative. Multiple erythematous vesicles are observed in a symmetrical pattern on the medial aspects of his buttocks. Direct immunofluorescence testing reveals granular IgA deposits along the apical part of papillae at dermoepidermal junction. Most likely diagnosis?
DERMATITIS HERPETIFORMIS, a cutaneous manifestation of Celiac Disease
How is Breslow thickness measured and what is its significance in melanoma diagnosis?
Breslow thickness is reported to the nearest 0.1 mm. It is measured vertically in millimeters from the granular layer (or base of superficial ulceration) to the deepest point of tumor involvement. It is important because it is a prognostic factor: the thicker the melanoma, the worst the outcome 8= more likely to metastasize).
List the 4 conditions that all share nail curvature alterations
Parrot beak nails
Tile-shaped nails
Pincer nails
Clubbed nails.

What's the clinical sign that helps differentiating Pemphigus Vulgaris from Bullous Pemphigoid? Explain how it is elicited
The clinical sign is Nikolsky sign, which is elicited by applying lateral pressure in the perilesional skin area.
If the sign is positive, the epidermis should dislodge/sheer off when pressure is applied; this occurs in intraepidermal blisters —> sign is positive in Pemphigus Vulgaris.
The sign is negative in subepidermal blisters --> negative in Bullous Pemphigoid.
Briefly explain what (1) pale (scar-like) areas and (2) nodular appearance refer to in the setting of Superficial Spreading Melanoma?
Pale (scar-like) areas refer to remission of the lesion (with the risk of underestimating the Breslow thickness);
The nodular appearance is a sign of deeper invasion (= progression to the vertical growth phase).
What are the two main classes of Epidermolysis Bullosa?
Acquired AND Inherited. Inherited further subdivided into simplex, junctional and dystrophic.
A 32-year-old male presents with a sudden onset of numerous small, droplet-shaped, erythematous papules and plaques on his trunk and proximal extremities. He reports a recent history of a streptococcal throat infection two weeks prior. He has no significant past medical history and no family history of psoriasis. The lesions are mildly pruritic but not painful. He denies any joint pain or other systemic symptoms. On physical examination, the patient has multiple small, erythematous, scaly papules and plaques distributed primarily on his trunk and proximal limbs. The lesions are well-demarcated and measure 1-10 mm in diameter. There is no evidence of nail involvement or joint swelling. Which type of psoriasis is presented in this case?
Guttate psoriasis
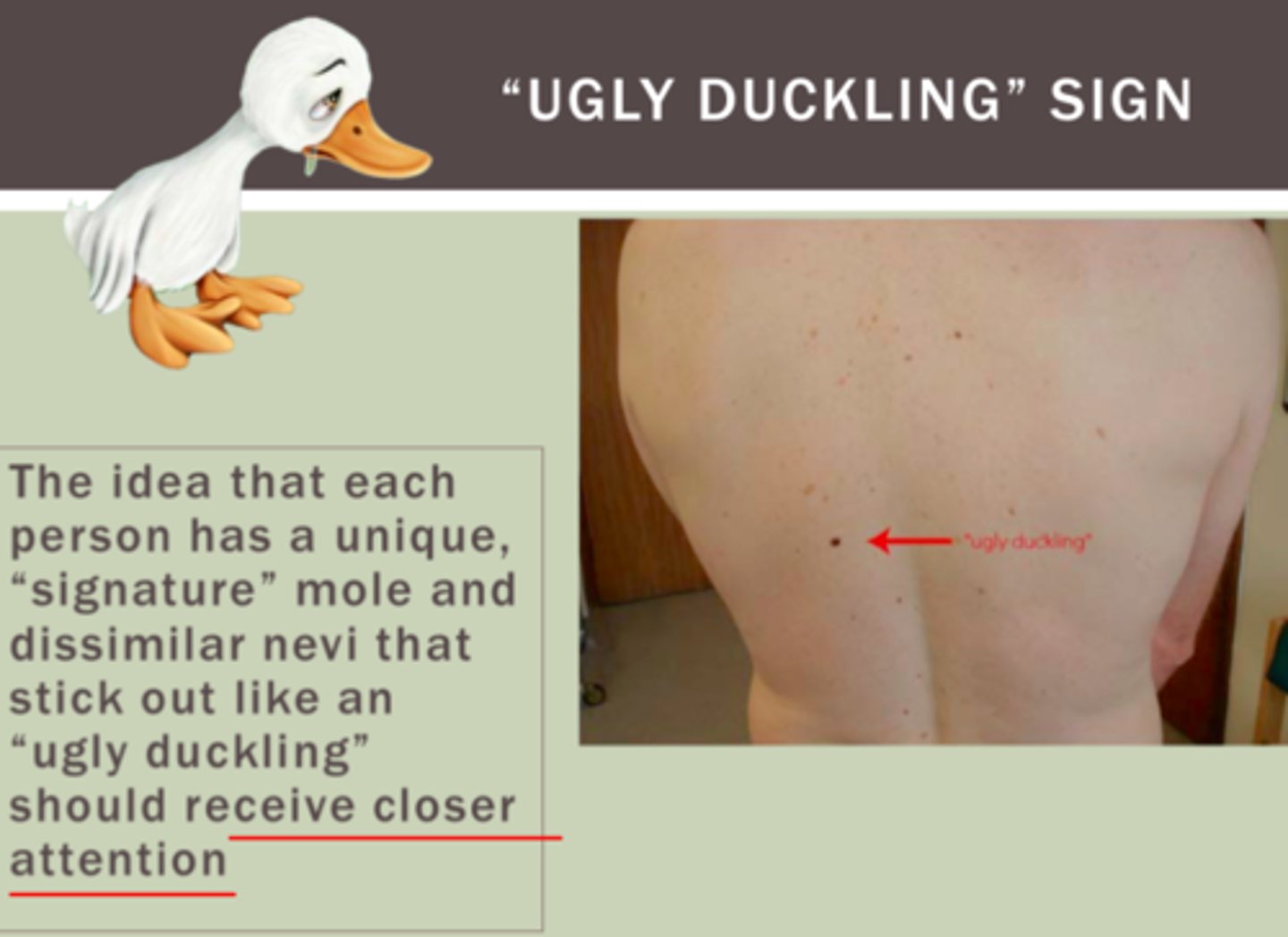
Please define the ugly duckling sign and what it is used for
The ugly duckling sign refers to a nevus that stands out and looks different from all the other nevi on the body of a person. It should be approached with a high index of suspicion. It is used as a clinical feature indicative of malignancy in a nevus.
State how blister location differs in the mucosal-dominant PV versus the mucocutaneous type PV. Which autoantibodies profile do you expect in these two subtypes?
In the mucosal-dominant PV, we find blisters and erosions in the deep layers of the mucosae, especially the oral mucosa. We expect positivity to anti-Desmoglein 3 IgG, since this glycoprotein is most abundantly expressed at this level.
In the mucocutaneous type of PV we find blisters in the deep layers of the mucosa and also in the epidermis; since it is an overlap between the mucosal type and the cutaneous type PV, in this case we have autoantibodies against both desmoglein 1 and 3.
What is the treatment of choice for urticaria?
2nd generation H1 antihistamines; corticosteroids;
2nd line: Cyclosporin;
3rd line: Omalizumab.
List at least 5 triggers of thermal urticaria.
Warm or cold environmental temperature;
Hot or cold water temperature when bathing or showering;
Hot or cold drinks or foods;
Fever;
Warm sunlight;
Local warming of the skin (heating pads);
Generalized overheating
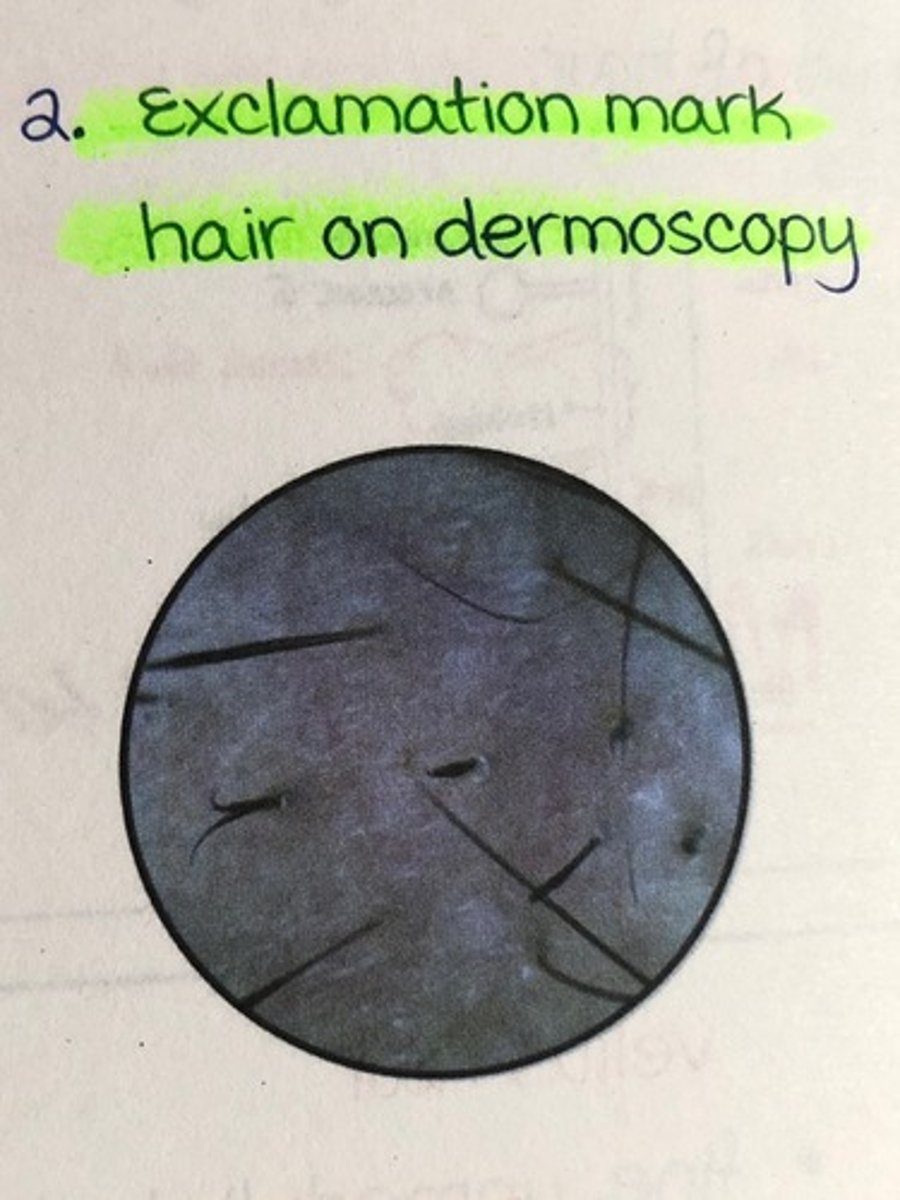
What is a typical clinical finding in alopecia areata?
Exclamation point hair + yellow dots
What are the least cancerogenic serotypes of HPV?
6, 11, 42, 43, 44
What are the diagnostic hallmarks of psoriasis on dermoscopy?
Red dotted vessels (due to dilation of capillaries within the dermal papillae)
White scales (due to proliferation of keratinocytes and cornified cells leading to thickening of the stratum corneum)

A 16-year-old male complains of itching of the face. He has a personal and family history of atopy (allergic rhinitis and asthma). The dermatologic examination revealed an erythema with small vesicles at the level of the armpit, consistent with eczema. A previous treatment with topical corticosteroids had temporary results. The patient is otherwise fine and has no other complaints.
Which is the most plausible diagnosis in this patient?
Atopic dermatitis

Name at least 3 different types of acne.
1. Acne vulgaris
2. Acne keloidalis
3. Acne conglobata
4. Adult acne
5. Acne fulminans
6. Acne excoriée
7. Infantile acne

What are the main areas of presentation of rosacea?
Forehead, nose, upper cheeks, chin.
Most often symmetric presentation

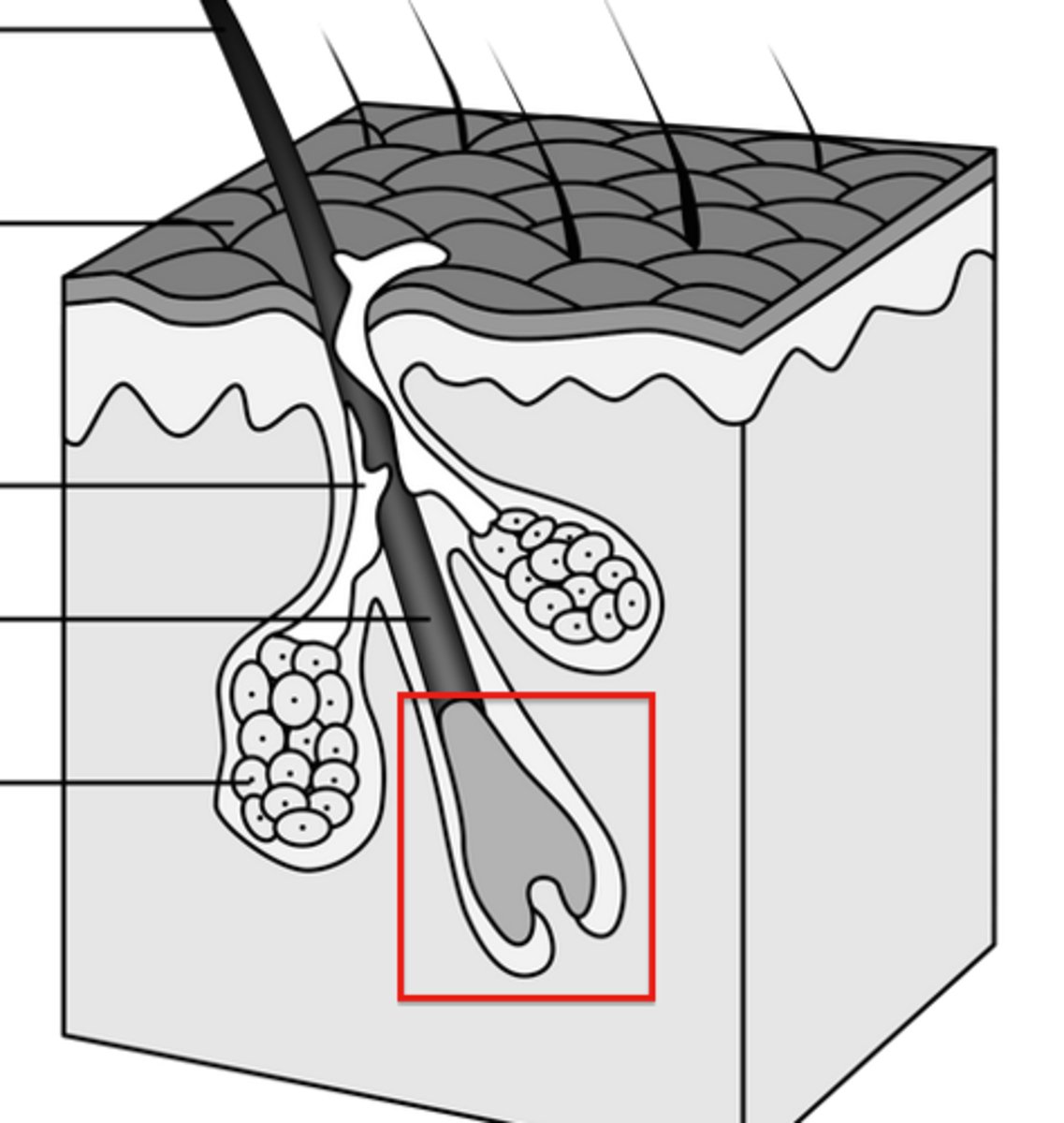
Which structure of the hair follicle contains matrix cells responsible for hair shaft production?
Hair bulb
List at least 3 cutaneous diseases associated with type I hypersensitivity reactions
Urticaria; Angioedema; Anaphylaxis

An 18-year-old male presents to the emergency department with a skin lesion that he has noticed for about two weeks. He describes the lesion as a red, scaly area on his scalp, with well-defined edges. On physical examination, the lesion has a "ring-like" shape with a clear center and red borders. No signs of enlarged lymph nodes or fever. The patient has no other symptoms but reports itching in the affected area. He has no significant history of skin diseases, although he has recently engaged in sports and shared equipment with other teammates. What is your diagnosis? Which kind of test would you use to confirm the diagnosis?
TINEA CAPITIS;
Gold standard: fungal culture and microscopic examination

State one form of a NON autoimmune pemphigus and explain why
Hailey Hailey disease is a form of a non-autoimmune pemphigus caused by an autosomal dominant mutation in the ATP2C1 gene which codes for a calcium channel.
List the exogenous risk factors of melanoma
1. UV radiation exposure
2. Sunburns
3. Geographical and environmental factors
4. Iatrogenic immunosuppression (e.g. organ-transplanted patients)
5. Artificial UV sources

What is the 4-step model of melanoma progression?
1. A driver mutation (i.e. BRAF mutation) makes the cell hyperactive in growth signaling
2. Escaping primary senescence (i.e. CDKN2A loss). Loss of CDKN2A allows cells to escape the natural aging stop signals
3. Overcoming apoptosis (i.e. TP53 mutation)
4. Immortalization (i.e. TERT-p mutation): mutations in TERT-promoter switch on telomerase, making the cell immortal
What is the main clinical distinguishing point between acne and rosacea?
The absence of comedones and presence of facial flushing in Rosacea.
Which patients most commonly present with Muehrcke's lines?
Patients with hypoalbuminemia / liver cirrhosis

.
In which condition can Pautrier microabscesses be observed?
MYCOSIS FUNGOIDES

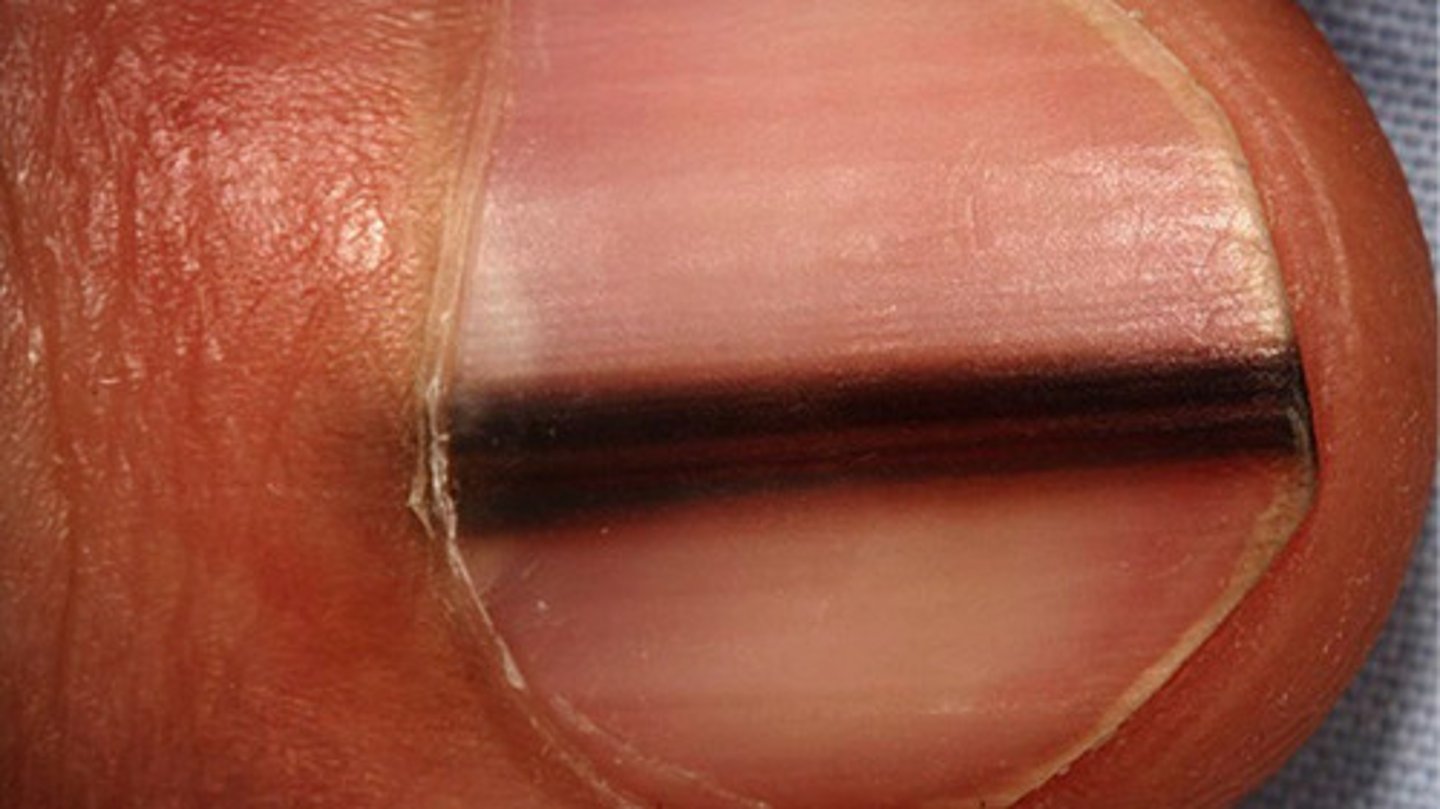
What is the key sign that allows us to distinguish between subungual melanoma vs. a benign melanocytic nevus of the nail matrix? (define in 1 sentence)
Hutchinson's sign = melanonychia with a necessary extension into the perionychium
A 52-year-old man presents with sudden, painless tongue and facial swelling without urticaria. He has been on ramipril for hypertension for 3 years. C4 is low. What is the diagnosis?
ACE-I INDUCED ANGIOEDEMA
How to differentiate Urticaria from Urticarial Vasculitis?
Based on the DURATION OF THE LESIONS:
- Urticaria: <24h
- Urticarial vasculitis >24h
List the 6 clinical main subtypes of basal cell carcinoma
1. Nodular BCC
2. Pigmented BCC
3. Superficial BCC
4. Morpheaform (sclerodermiform) BCC
5. Uncus rodens (ulcerated BCC)
6. Pinkus tumor

List at least 3 cutaneous diseases associated with type III hypersensitivity reactions
1. SLE
2. Leukocytoclastic vasculitis
3. IgA vasculitis
Define Pustule and list the names of 4 diseases that appear with this lesion
PUSTULE: circumscribed, raised papule containing visible pus.
1) Acne vulgaris
2) Acne fulminans
3) Palmoplantar pustular psoriasis
4) Impetigo

Erysipelas: definition, pathogenesis and manifestations
Erysipelas is an acute bacterial dermal and subdermal infection characterized by red, shiny, raised, spreading plaques with well-demarcated edges. It is caused by Streptococcus group A and it needs a portal of entry for the infection, which can be a small skin lesion or tinea pedis. The classical sign is the step sign, which refers to the characteristic sharp separation between the healthy skin and the infected skin area, which has well-demarcated borders. Touching the plaque, it is possible to feel a palpable raised plaque.

List and explain 3 possible environmental triggers for psoriasis
Infections: Streptococcal throat infections are a well-known trigger for guttate psoriasis.
Trauma: physical injury or trauma to the skin (e.g., cuts, sunburn, or scratches) can trigger the onset or worsening of psoriasis in a phenomenon known as the Koebner phenomenon.
Vitamin D deficiency: Vitamin D has both significant immunomodulatory effects and anti-inflammatory effects. It promotes the differentiation of regulatory T cells (T-reg), which help maintain immune tolerance and prevent excessive inflammatory responses and is also expressed in keratinocytes, regulating their proliferation and differentiation. Vitamin D exerts anti-inflammatory effects by downregulating pro-inflammatory cytokines such as IL-17, IL-22, and TNF-α and thus is used as a drug in psoriasis.
Illustrate treatment of herpes zoster
High-dose acyclovir (800 mg 5 times daily for 7 days) within 72h of the onset of the eruption.
If the eye is affected/there is nerve compression: intravenous acyclovir (5 mg/kg every 8h for 5 days) should be considered, and patients may require systemic steroids (prednisolone 40–60 mg daily) to prevent nerve paralysis in severe cases.
Vitamin B supplements to reduce the risk of post-herpetic neuralgia (PHN).
Why does pityriasis versicolor leave vitiligoid spots that disappear at the end of the treatment and sun re-exposure (after treatment)?
Malassezia produces azelaic acid, a compound that inhibits tyrosinase, the enzyme responsible for melanin production. This leads to temporary hypopigmentation in affected areas, and in fact, Pityriasis versicolor becomes initially apparent as pale spots that fail to tan in the sunlight. This effect is temporary, and melanocytes gradually resume normal function after treatment.
Write the differential diagnosis between Erythrasma and Tinea cruris in their etiology, clinical appearance and diagnostic tests
TINEA CRURIS:
Dermatophytes
Yellowish-brownish, scaly patches with well-defined, raised borders and central clearing.
It’s often bilateral and symmetric.
Wood’s lamp: positive for yellow-green fluorescence.
Culture: can identify dermatophytes.

ERYTHRASMA:
Corynebacyterium minutissimum (gram-positive)
Coral red patches with poorly defined margins and fine scaling.
Often unilateral and asymmetric.
Wood’s lamp: positive for coral red fluorescence
Gram stain and culture: can confirm Corynebacterium minutissimum

List at least 3 cutaneous diseases associated with type IV hypersensitivity reactions
Allergic contact dermatitis
Atopic dermatitis (overlapping with type 1)
Psoriasis (innate immunity with type 4)
What are the possible clinical skin manifestations of type I/II/III/IV hypersensitivity reactions?
Type I: wheals
Type II: blisters
Type III: erythematous macula that does not disappear under pressure
Type IV: eczema
What is the main germline mutation of melanoma?
The main germline mutation in melanoka affects the CDKN2A locus on chromosome 9p21. When CDKN2A is mutated or deleted, there is a loss of function of its two tumor suppressor proteins p14 and p16, which normally act as negative regulators of cell cycle progression. With this mutation, as a result, there is unchecked cell proliferation and tumor development.
What distinguishes scarring from non-scarring alopecia?
Irreversible follicle destruction and replacement with fibrous tissue (in scarring alopecia)
During which phase of the hair cycle does apoptosis-driven follicular regression occur?
Catagen phase.