Reproductive 1 - Male Intro, Testes
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
Main functions of the reproductive system
Production of gametes, Organs for mating, Fertilization
What are the organs of the reproductive system
Gonads, Pathway of gamete transport, Accessory reproductive organs/glands
Function of gonad
Gamete production and sex hormone secretion
What are the male gonads
Testes
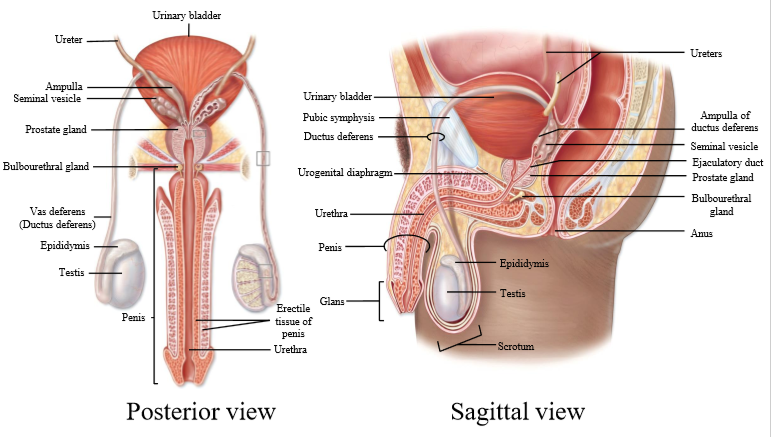
Where is the vas deferens?
The vas deferens is the tube which connects the epididymis to the ejaculatory duct, which the merges with the urethra.
What glands add secretions to the vas deferens
Prostate gland, seminal vesicle
What is the urethra
Channel that leads from bladder to outside the body
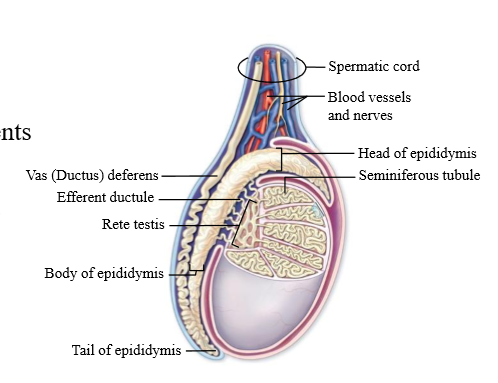
What is inside the Scrotal sac
Testes, blood vessels, Nerves, Slit from abdomen to scrotal sac, spermatic cord
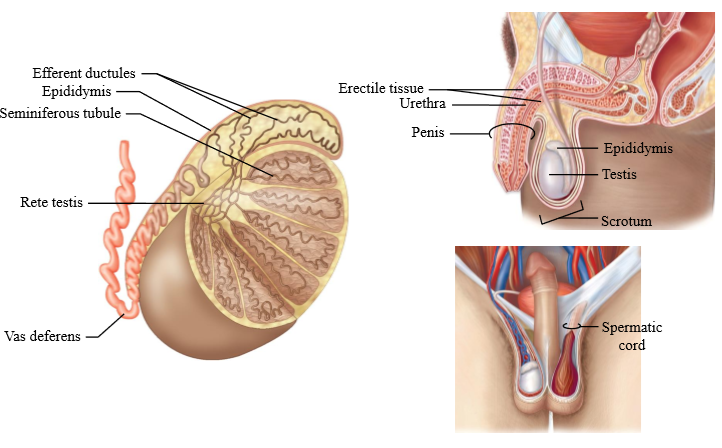
What is the spermatic cord
Combo of Vas deferens, nerves, blood vessels
What is countercurrent blood flow
Hairpin arrangement of the arterial and venous vessels, resembling the renal micro-vasculature, could produce a "countercurrent" flow system in which blood flow occurs in opposite directions.
What is the use of countercurrent blood flow in the scrotum
Testes must be colder than the body for optimal spermatogenesis. Counter current blood flow allows for the artery heat to diffuse to the veins (cools the blood)
Where are the testes located in gestation?
In the abdominal cavity
Testes Descent
At 8 weeks, testes are in the abdominal cavity
- At 12 week, testes move to inguinal canal
- Between 7 and 9 months the testes pass into inguinal canal and sit into scrotum
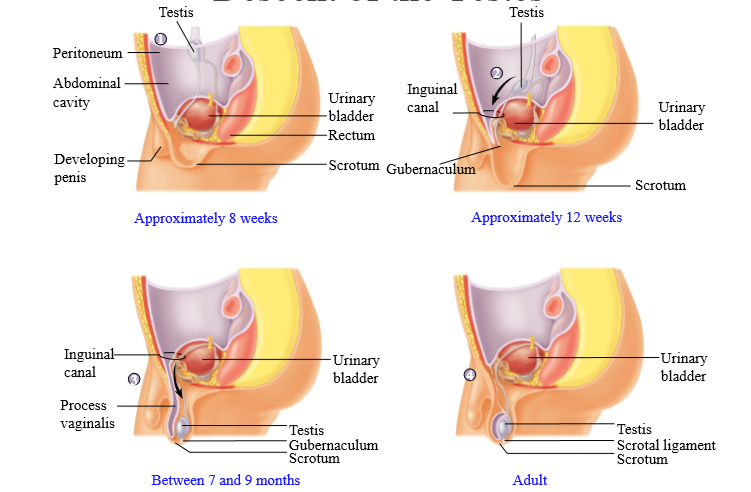
What happens if male babies are born premature?
Testes may not be descended: surgical procedure can correct for it
What is inside the testes
250-300 compartments with seminiferous tubules
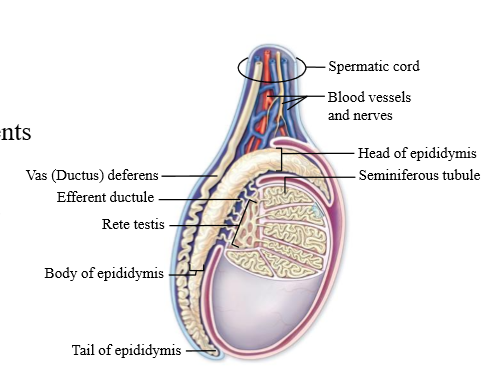
Rete testes
a set of tubules that the sperm enters after the seminiferous tubules. sperm then is carried to the epidiymis
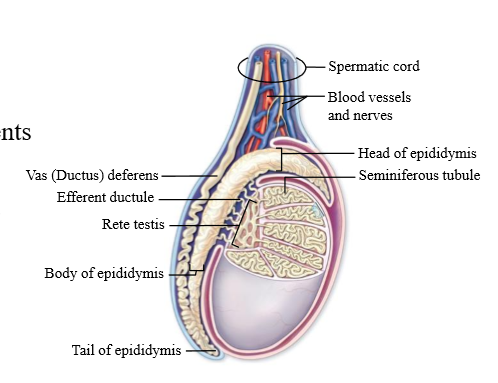
Efferent tubules
connection between the Rete Testes and the Epididymis
Role of seminiferous tubules
Site of sperm production
Cells of the seminiferous tubules
sertoli cells and spermatogenic cells
When does spermatogenesis begin?
Puberty
What virus can affect the seminiferous tubules
The mumps virus. Usually seminiferous tubules are well protected, but this virus can get in
How much sperm is ejaculated
400 million sperm per 3mL volume
What are the cell types of the testis
Leydig cells, Sertoli cells, Smooth muscle cells
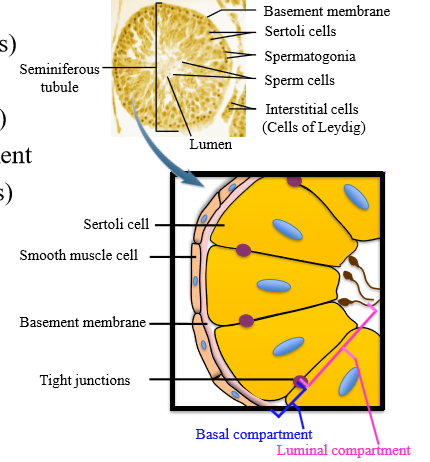
Leydig cells location + function
In the interstitial space, secrete testosterone
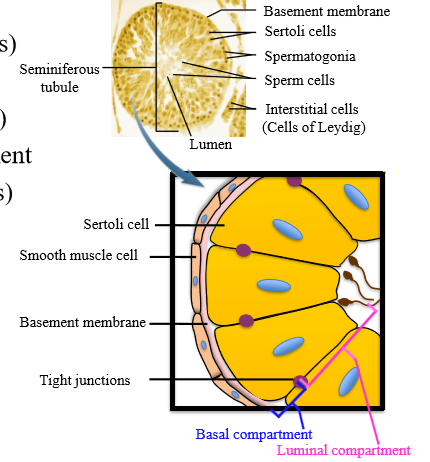
Sertoli cells role and location
Line the seminiferous tubule (epithelial), support sperm development
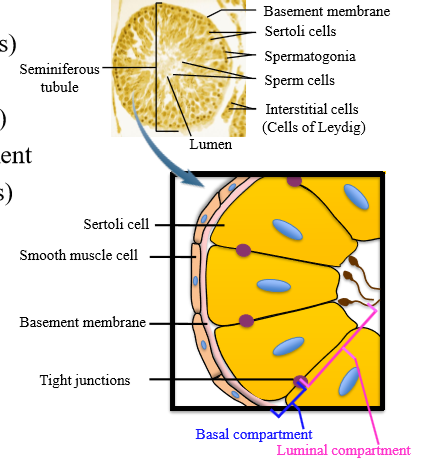
Role of myoid cells
smooth muscle cells to contract to push sperm and testicular fluid through tubules
What creates the blood testes barrier
tight junctions between sertoli cells
Basal compartment of testes
Area between tight junctions and basement membrane
Luminal compartment of testes
Area between tight junctions and the lumen
Functions of the sertoli cells (7)
1. Support sperm development
2. Secrete luminal fluid for sperm housing
3. Secrete androgen-binding protein
4. Act as target cells for testosterone and FSH
5. Secrete inhibin
6. Phagocytosis of old and damaged sperm
7. Site of immunosuppression (blood testis barrier)
Role of androgen-binding protein
Helps maintain steady androgen concentration in lumen
How do sertoli cells act as target cells for test and FSH
Testosterone permeates and binds to androgen binding protein. Test + FSH acts on sertoli cells to secrete paracrine factors for spermatogenesis
Role of inhibin
Influenced by FHSG, it regulates the hypothalamic pituitary testes axis
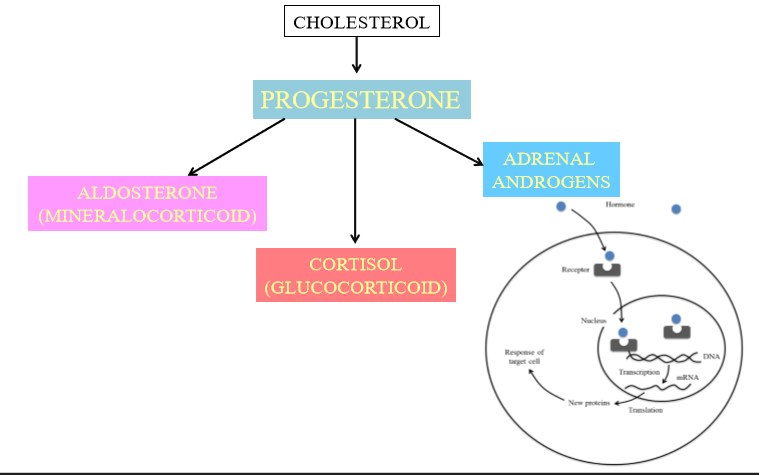
What is the precursor substance of testosterone
Cholesterol
Where is testosterone produced?
testes (leydig cells) and adrenal glands
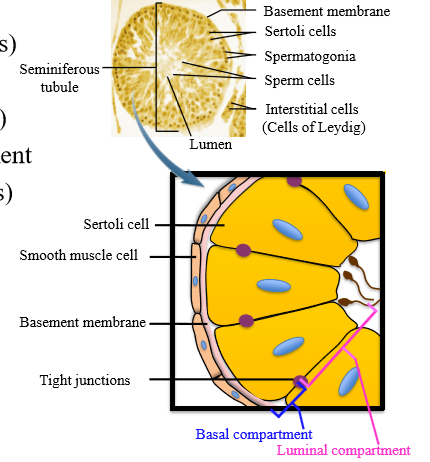
Where progesterone synthesized and what is its role
Synthesized in adrenal cortex, can form mineralocorticoids (aldosterone), glucocorticoids (cortisol), and androgens
Where are testosterone receptors located?
Intracellular, as testosterone is lipophillic
Leydig cell testosterone metabolism
Cholesterol is converted into pregnenolone. Pregnenolone can be converted into progesterone, which can be converted to androgens (test). Pregnenolone can also be converted directly to androgens
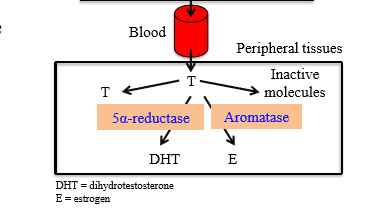
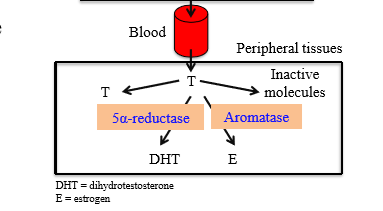
Role of testosterone in the blood stream
Can act on testes, be converted to dihydrotestosterone, be converted to estrogen, or be broken down into inactive molecules
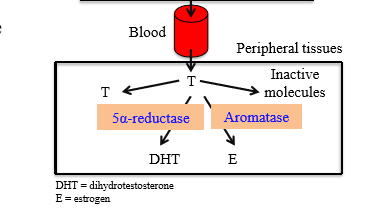
What enzyme converts Testosterone to DHT
5 alpha reductase
Role of Dihydrotestosterone
Maintainss sexual characteristics and prostate gland. Also causes receding male hairline.
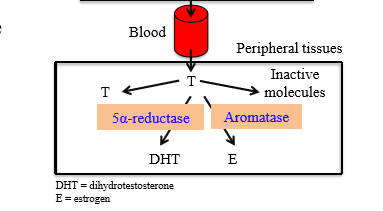
Enzyme + Location of Testosterone conversion to estrogen
Aromatase in the liver, adipose, and brain
When does male puberty start, and what does it develop
Around 10-14 years, and lasts 5 years. Develops sexual maturation, reproductive organ maturation, develops secondary sexual characteristics
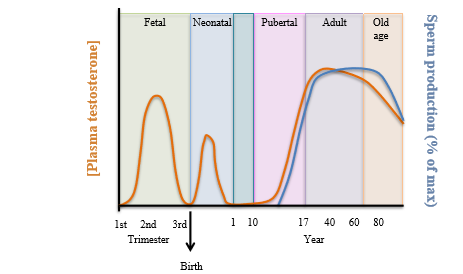
Pattern of testosterone production over lifespan
- High amount of testosterone in gestation, and then decreases at birth.
- Neonates have high peak of testosterone which decreases at age 1. - Testosterone is low for childhood years, and ramps up in puberty and remains high for adult years
- Starts to lower around age 40
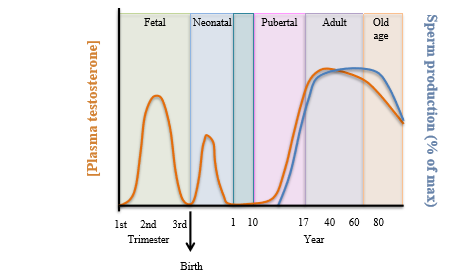
Pattern of Sperm production over lifespan
Rises at puberty, maintains at age 45, then declines. Parallels with andropause
How is testosterone regulated
Hypothalamic-Pituitary-Leydig Cell axis. Higher centers can send signals to hypothalamus. The hypothalamus releases GnRH to anterior pituitary. Anterior pituitary releases LH to leydig cells for testosterone secretion. FSH stimulates sertoli cells
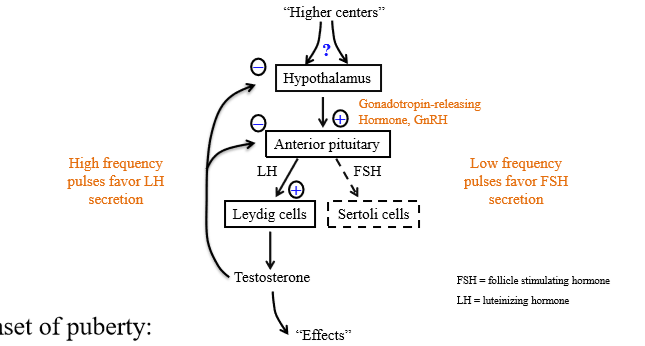
Role of pulsatile secretion of GnRH from hypothalamus and anterior pituitary
Constant GnRH will make the pituitary non-responsive. It controls the responsiveness of the pituitary gland
What cells secrete FSH and LH
Gonadotrophs
What type of regulation does testosterone provide
Negative feedback reguator. Dampens the amplitude of hypothalamus pulsatile secretion and causes decreased response to GnRH = less LH and FSH
What are the secondary sexual characteristics seen at male puberty
Hair growth, deepening of voice, rapid growth in height
Effects of Androgens on the body (6)
- Stimulate spermatogenesis
- Promotes development of secondary sex characteristics during puberty and maintenance of these characteristics in adult life
- Increase sex drive
- Promote protein synthesis in skeletal muscle (anabolic)
- Stimulates growth hormone secretion, permitting bone growth in adolescence
- Promote development of male reproductive structures during embryonic life