Chapter 7 - Dealing with Disease
1/81
Earn XP
Description and Tags
Chapter 7 of U4 AOS 1 Biology 3/4
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
Antigen
Proteins on the surface of cells allowing immune system to recognise self cells.
Self Cells
Our own cells and tissues
Non Self Cells. Provide Examples.
NOT our own cells. Such as pollen, dust, pathogens.
What can antigens be made out of?
Most are protein based. Can also be made out of carbohydrates, lipids and nucleic acids.
What is MHC full form?
Major Histocompatibility Complex
MHC
Group of special proteins which display whether cell is healthy or infected. Does this by bringing antigens to the surface for immune cells to “read”
What are the types of MHC classes?
Class 1: Found on all nucleated cells
Class 2: Found on certain specialised cells within the immune system
What is an Autoimmune Disease? Provide an example.
An autoimmune disease occurs when the body’s immune system recognises self antigens as foreign. An example includes Type 1 Diabetes.
What is an allergen? What are typical antigens individuals might have an allergen for?
An allergen occurs when a strong immune response (e.g. sneezing, swelling) is initiated for relatively harmless antigens. Typical antigens include dust, pollen, peanuts.
Pathogens
Agents causing disease. Contain unique antigens which can be recognised by the immune system.
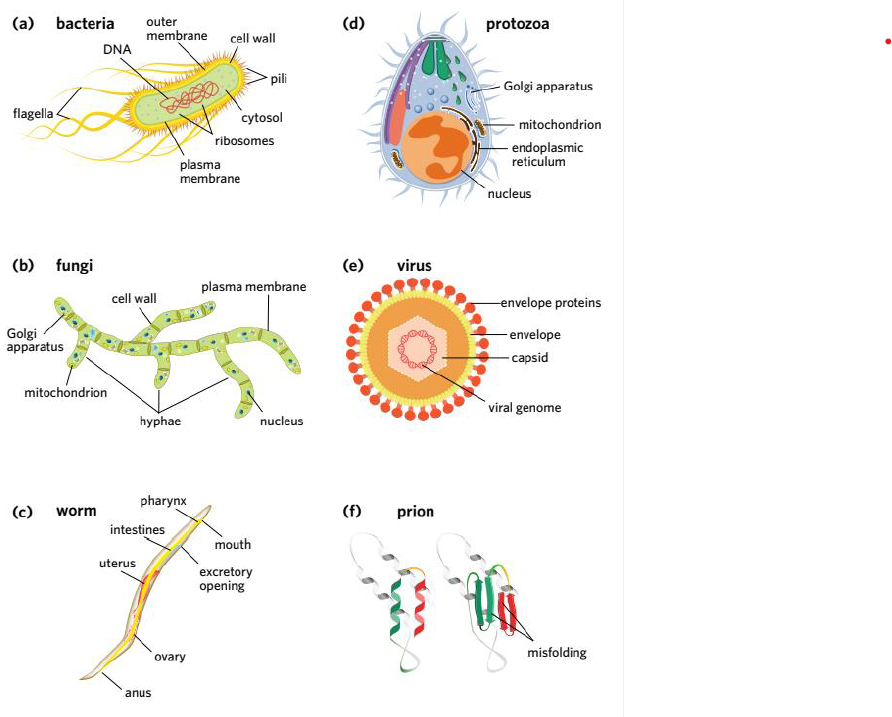
Pathogens can either be:
Cellular (1 or more cells) or Non Cellular (Not made up of cells, but viruses)
Cellular Pathogens are _____ and Non Cellular Pathogens are ______. Examples of both include:
Living. Non Living.
Living Pathogens include Bacteria, Fungi, Worms
Non Living Pathogens include Viruses, Viroids, Prions.
What are non infectious diseases caused by?
Factors such as Genetics, Lifestyle, Environment and Nutrition.
What are all the different types of pathogens?
What are the 2 types of Immunity? Where do defense lines 1-3 reside?
Innate Immunity (Non specific) and Adaptive Immunity (Specific). Lines 1 and 2 are Innate. Line 3 is Adaptive.
What is a physical barrier? Include examples.
A physical barrier blocks entry into the body.
Examples include: Leaves’ Waxy cuticles, Skin, Cilia
What is a chemical barrier? Include examples.
Molecules which kill or neutralize pathogens using chemicals produced by the organism.
Examples include: enzymes and acids (animals), Plant toxins, Venom
What is a microbiological barrier? Include examples.
Use of microbes which crowd out or inhibit harmful pathogens.
Examples include: Gut Bacteria (Humans), Endophytes (Plants), Skin Flora (Human).
What does it mean for something to be non specific?
It means that 1 specific pathogen isn’t targeted. Instead, it reacts broadly and uniformly to a wide range of invaders (bacteria, viruses, fungi, etc.), regardless of their identity.
What does immunological memory refer to?
Refers to the immune system's ability to "remember" a specific pathogen after an initial exposure, allowing for faster detection in future.
What is a leukocyte? Where are they produced?
Defend the body against infectious disease, foreign invaders, and abnormal cells. AKA white blood cells. Made in Bone Marrow.
Protective Processes
Inflammation, Preventing Blood Loss, Fever
Defensive Cells
Phagocytes, Granulocytes, Natural Killer Cells
Defensive Chemicals
Interferons, Cytokines, Chemokines, Complement Proteins
Phagocytes
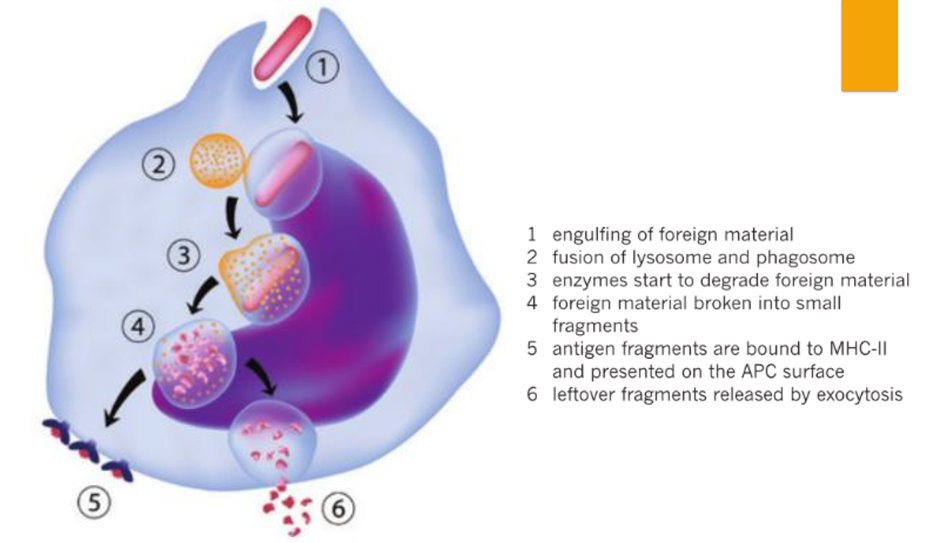
Leukocytes which are able to engulf and break down pathogens in phagocytosis. Some phagocytes also act as Antigen Presenting Cells (APCs).
Phagocyte Examples
Neutrophils, Macrophages and Dendritic Cells
Phagocytosis Steps
Granulocytes
Leukocytes containing many cytoplasmic granules, released during an immune response. Secrete range of defensive molecules during innate immune response.
Granulocyte Examples
Neutrophils, Eosinophils, Mast cells
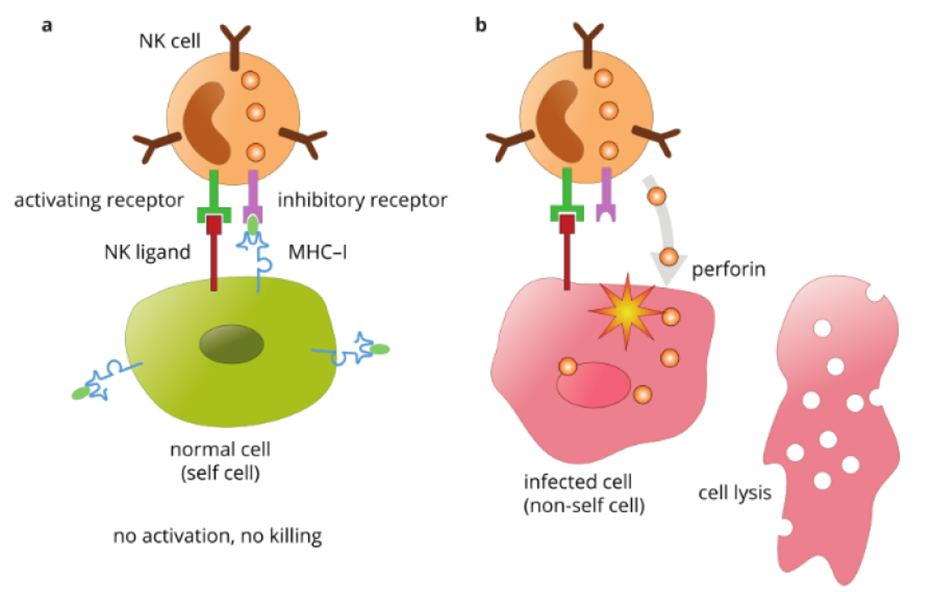
What is occurring in a)
NK cell recognises self cell due to presence of MHC-1 and does not elicit an attack.
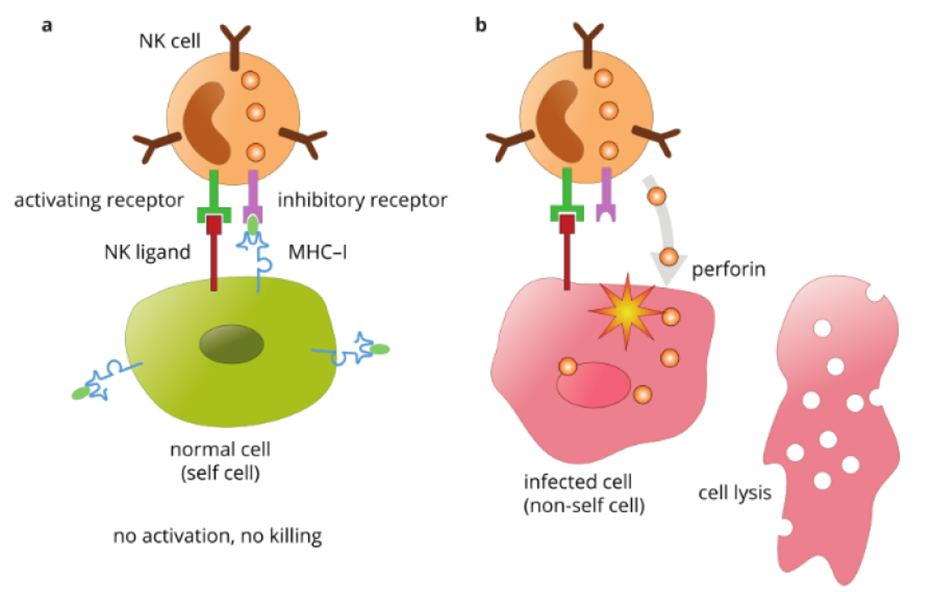
What is occurring in b)
MHC-1 is absent from cell’s surface. NK cell recognises it as damaged/infected. NK cell elicits response to destroy the cell.
Cytokines (+Example)
Small signaling proteins regulating immune responses (subtopic). e.g. Interferon. Secreted by virally infected cells, interacting with neighboring cell receptors causing changes, decreasing viral infection susceptibility.
Chemokines
Cytokine subtype which directs movement of immune cells to where they are needed.
Complement Proteins
Proteins which “complement” (enhance) ability of antibodies and immune cells to fight off pathogens.
What happens when complement proteins react with one another?
A complement cascade occurs. Can result in Oponisation, Chemotaxis or Lysis.
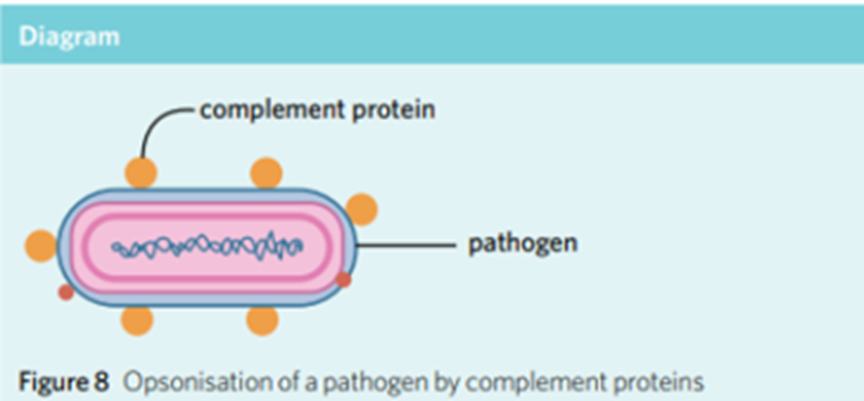
Oponisation
Complement proteins stick on outside surface of pathogens, assisting cells (e.g. Phagocytes) to recognise as foreign.
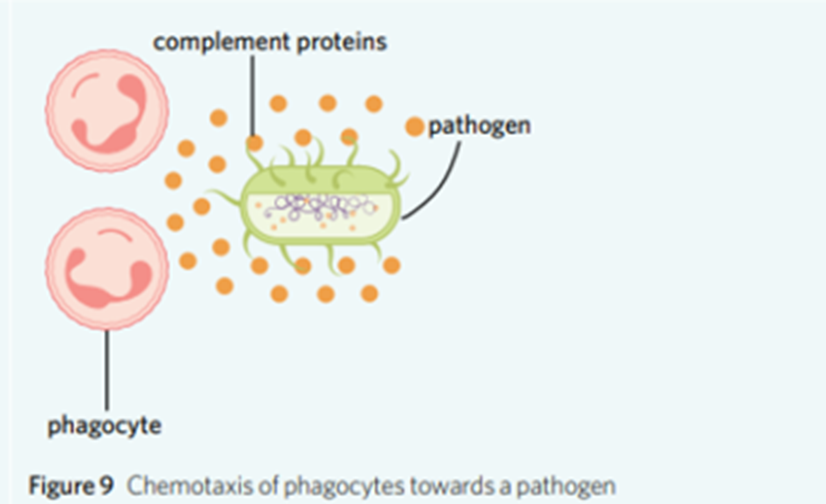
Chemotaxis
Complement Proteins gather near the pathogen, attracting phagocytes, to increase likelihood of being destroyed.
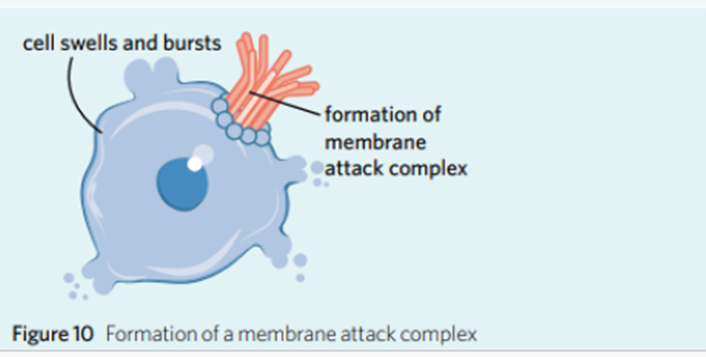
Lysis
Complement proteins join together on pathogen surface, forming membrane attack complex (MAC), creating pores in membrane. Sudden influx of fluid into pathogen causes pathogen to burst.
Fever
Increase of body temperature (b/c of inflammatory cytokines) to slow bacteria/viruses by shifting temperature away from optimal range. Also, allows increase in leukocyte activity.
Inflammation
Accumulation of fluid, plasma proteins and leukocytes that occurs when tissue is damaged or infected. Results in heat, pain, swelling, loss of function.
How is Inflammation initiated?
When tissue becomes damaged, damaged cells release substances.
Inflammatory Response Steps
Pathogens breach the first line of defense (such as through wound in skin)
Injured cells release cytokines attracting neutrophils (X) and mast cells which release histamine
Vasodilation increases, allowing leukocytes and fluid with complement proteins to enter infected tissue. Platelets clot at site of wound.
Neutrophils migrate towards cytokines and are activated, causing neutrophils to recruit macrophages and secrete factors, such as defensins and hydrogen peroxide, degrading and killing pathogens.
Macrophages activate and secrete cytokines and neutrophils, phagocytosing pathogens and debris at infection site. Can lead to pus production.
Response continues until pathogen eliminated and wound has healed.