Chapter 19: The Kidneys Part 1単語カード | Quizlet
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
What is the most important function of the kidney?
homeostatic regulation of water and ion content of the blood
(salt and water balance/fluid and electrolyte balance)
What are the six general areas that kidney function is divided into?
1. Regulation of extracellular fluid volume and blood pressure
2. Regulation of osmolarity
3. Maintenance of ion balance
4. Homeostatic regulation of pH
5. Excretion of wastes
6. Production of hormones
Kidney Function: regulation of extracellular fluid volume and blood pressure
ECF vol decreases, BP decreases
If ECF vol and BP fall too low, body can't maintain adequate blood flow to the brain/essential organs.
kidneys work with CV system to ensure that BP and tissue perfusion remain at homeostatic ranges
Kidney Function: Regulation of osmolarity
Integrates kidney function with behavioral drives (like thirst) to maintain blood osmolarity at 290-300 mOsm
related to plasma volume
Kidney function: maintenance of ion balance
kidneys keep concentrations of key ions within normal range by balancing dietary intake with urinary loss.
Na+ is the major ion involved in regulation of ECF volume and osmolarity.
K+ and Ca2+ concentrations are also closely regulated
related to plasma volume
Kidney function: homeostatic regulation of pH
pH of plasma is kept within a narrow range
if ECF is too acidic, kidneys remove H+ and conserve bicarbonate ions (buffers)
if ECF is too alkaline, kidneys remove bicarbonate and conserve H+
kidneys do not correct pH disturbances as quickly as lungs do
Kidney function: excretion of wastes
Kidneys remove metabolic waste products and xenobiotics (aka foreign substances like drugs/toxins)
Metabolic wastes include:
creatinine from muscle metabolism
nitrogenous wastes like urea and uric acid
urobilinogen from hemoglobin (gives urine the yellow color)
Some hormones
Kidney function: production of hormones
Kidneys are NOT endocrine glands, but play a role in 3 endocrine pathways
Kidney cells synthesize:
erythropoietin
- cytokine/hormone that regulates RBC synthesis
renin
- enzyme that regulates the production of hormones involved in sodium balance and blood pressure homeostasis
vitamin D production enzymes
help convert vit. D3 into a hormone that regulates Ca2+ balance
What structures does the urinary or renal system consist of?
Kidneys (2)
- paired
- have nephrons: hollow tubules where urine production begins
- involved in urine production
- retroperitoneal
Ureters (2)
- urine transport
- retroperitoneal
Urinary Bladder
- urine storage
Urethra
- urine transport
How much of the cardiac output do the kidneys receive?
20-25% even though they constitute only 0.4% of total body weight
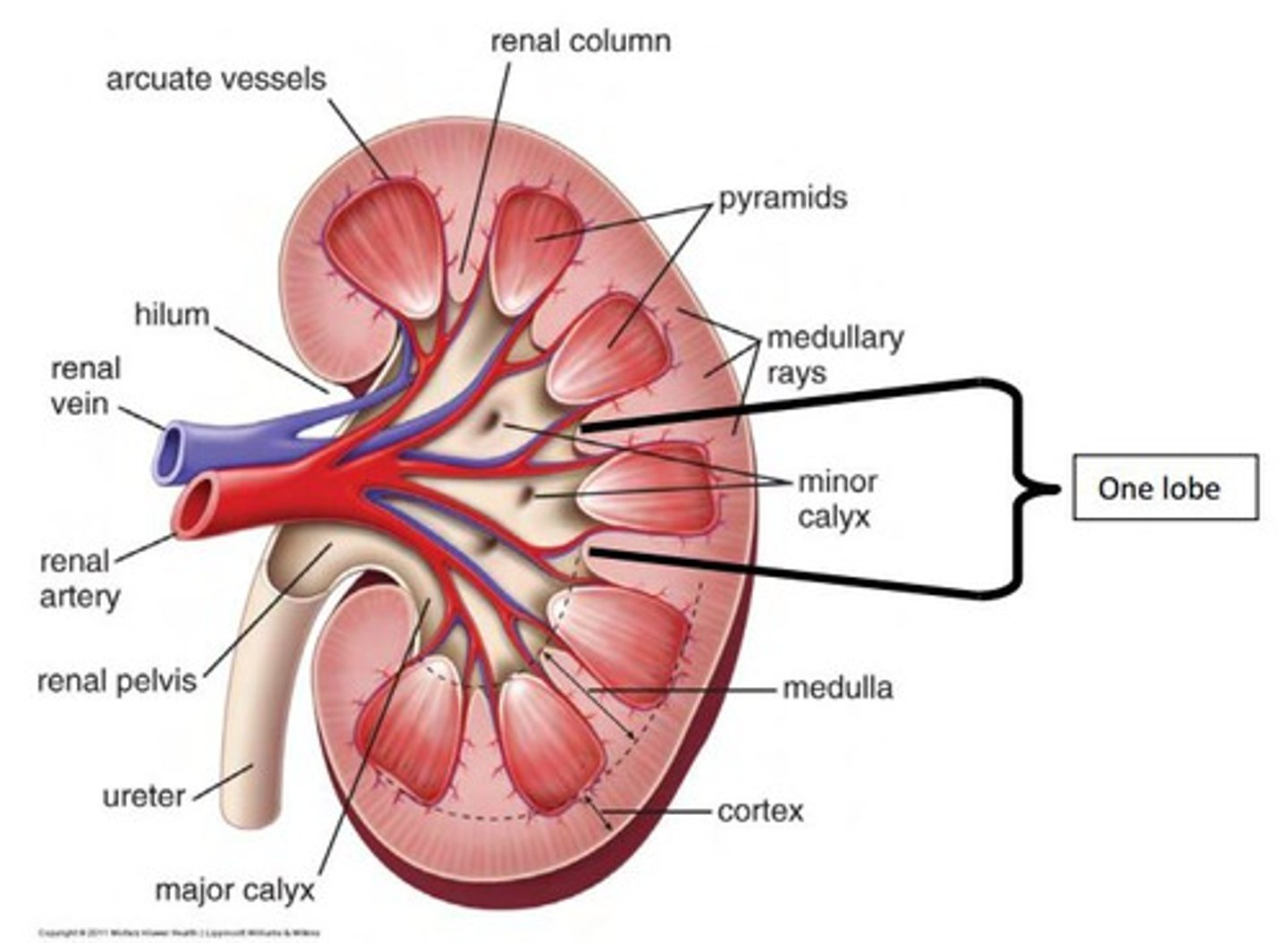
What are the structures of the kidney?
Renal capsule surrounds kidney
the interior is arranged into an outer cortex and inner medulla
- formed by the organized arrangement of nephrons
- 80% nephrons in kidney are in the cortex (cortical): efferent arteriole --> peritubular capillary
- 20% nephrons in kidney dip into the medulla (juxtamedullary): efferent arteriole --> peritubular capillary & vasa recta and collecting ducts
medulla contains renal pyramids
renal pelvis
What is the functional unit of the kidney?
the nephron
smallest structure that can perform all the functions of the kidney
1 million nephrons in kidney
nephrons are divided into sections, each section is closely associated with specialized blood vessels
Kidney blood vessels form a portal system, explain
blood flows from renal arteries into afferent arteriole. From afferent arteriole to the first capillary bed (glomerulus). Blood leaving the glomerulus flows into an efferent arteriole, then into the second set of capillaries, peritubular capillaries that surround the tubule. In juxtamedullary nephrons, the long peritubular capillaries are called vasa recta. Finally peritubular capillaries converge to form venules and small veins sending blood out of the kidney through the renal vein
renal artery --> afferent arteriole --> glomerulus --> efferent arteriole --> peritubular capillaries (vasa recta) --> venules --> renal vein
What is the function of the renal portal system?
to filter fluid out of the blood and into the lumen of the nephron at the glomerular capillaries, then to reabsorb fluid from the tubule lumen back into the blood at the peritubular capillaries
Where does the nephron begin?
in the Bowman's capsule: surrounds the glomerulus and is hollow/ball like
- endothelium of glomerulus is fused to the Bowman's capsule epithelium so that fluid filtering out of the capillaries passes directly into the lumen of the tubule.
glomerulus + Bowman's Capsule = renal corpuscle
From the Bowman's Capsule, where does filtered fluid flow?
into the proximal tubule, then into the loop of Henle (dips down toward medulla and back up)
Loop of Henle is divided into 2 limbs:
thin descending limb
ascending limb w/thick and thin segments
- contains the juxtaglomerular apparatus: where it passes between afferent and efferent arterioles
fluid then passes into the distal tubule
Where does fluid flow after it passes through the distal tubule?
The distal tubules of up to 8 nephrons drain into the collecting duct which pass from the cortex through the medulla and drain into the renal pelvis
from the renal pelvis, the filtered and modified fluid (URINE) passes into the ureter and is on its way to excretion.
Nephron blood supply comes from where?
renal corpuscle
- afferent arteriole
- glomerulus
- efferent arteriole
nephron tubules
- efferent arteriole
- peritubular capillary network
- cortical nephrons
- vasa recta
- juxtamedullary nephrons: speicialized - countercurrent exchange
What are the structures of the renal corpuscle?
glomerulus
- endothelium
- fenestrated capillaries
- basement membrane
Bowman's capsule
- parietal layer
- Bowman's space
- visceral layer
- podocytes: filtration slits
- basement membrane
Filtration membrane
- endothelium
- fused basal lamina
- podocytes
What is the juxtaglomerular apparatus?
Contains the Macula Densa: junction of ascending loop of Henle and renal corpuscles
contains juxtaglomerular or granular cells
- afferent arteriole
- produce renin
What are mesangial cells?
smooth muscle cells (modified)
- between and around loops of glomerular capillary
- regulate blood flow by contractile activity
- they contract and alter blood flow through the capillaries
- also secrete cytokines associated w/immune and inflammatory processes
What are the 3 basic process that take place in the nephron?
filtration, reabsorption, secretion
Urine formation
What is filtration or glomerular filtration?
the movement of fluid from blood into the lumen of the nephron.
Takes place ONLY in the renal corpuscle where the walls of the glomerular capillaries and Bowman's capsule are modified to allow bulk flow of fluid
What is the standard glomerular filtration rate or GFR?
for a 70 kg person
180L/24 hours
7.5L/hour
125mL/min
3L of plasma filtered sixty times per day
300 mOsm
Is all of the plasma filtered?
filtration fraction = 20%
is the percentage of total plasma volume that filters into the tubule
What are filtration barriers?
substances leaving the plasma must pass through 3 of them before entering the tubule lumen
- the glomerular capillary endothelium
- fenestrated capillaries w/large pores that allow most components of plasma to filter through
- pores are small enough to prevent blood cells from leaving the capillary though.
- a basal lamina: acellular layer of extracellular matrix
- excludes plasma proteins from the fluid that filters through it
- epithelium of Bowman's capsule
- podocytes: long foot processes that leave narrow filtration slits
After filtrate leaves Bowman's capsule, what happens?
it is modified by reabsorption and secretion.
What is reabsorption and where does it occur?
process of moving substances in the filtrate from the lumen of the tubule back into the blood flowing through the peritubular capillaries
filtrate to blood
- only reabsorbs good material
occurs in the Proximal tubule, loop of henle, and distal convoluted tubule
What is secretion and where does it occur?
selectively moves molecules from the blood and adds them to the filtrate in the tubule lumen
Blood to filtrate
occurs ONLY in the distal convoluted tubule
How much filtrate is removed from the body per day via secretion?
1.5L/day
at 50-1200 mOsm (lower or higher than normal)
removes unwanted material from the blood
Amount excreted equation
Amt excreted = amt filtered - amt reabsorbed + amt secreted
E = F-R+S
amounts vary w/physiological control
What does it mean when excretion>filtration?
glomerular filtration and tubular secretion
NO reabsorption
What does it mean when excretion
glomerular filtration and some tubular reabsorption
- no secretion
What does it mean when excretion = 0?
glomerular filtration and total tubular reabsorption
NO secretion
How do you calculate filtration of a solute?
filtration of solute = [solute] in plasma x GFR
What is the glomerular filtration rate?
amount of plasma filtered per time
70 kg person -
180 L/24 hrs or 7.5 L/hr or 125 mL/min
3 L of plasma filtered 60 times per day
What are 2 influencing factors of GFR?
Net filtration pressure: hydrostatic and colloid osmotic pressures
Filtration coefficient:
- surface area for filtration
--- glomerulus surface area
- action of mesangial cells
- permeability of the filtration membrane
--- size barrier: cellular components of blood, proteins, chemicals bound to proteins won't pass usually
--- permeability of the substanc
How does hydrostatic pressure influence blood flow through glomerular capillaries?
forces fluid through the leaky endothelium
averages 55 mmHg and FAVORs FILTRATION into Bowman's capsule
How does colloid osmotic pressure influence blood flow through glomerular capillaries?
it is inside the glomerular capillaries
higher than that of fluid in Bowman's capsule
avg 30 mmHg and Favors fluid movement BACK INTO THE CAPS
How does hydrostatic fluid pressure influence blood flow through glomerular capillaries?
opposes fluid movement into the capsule
avg 15 mmHg
opposes filtration
How do you calculate the net filtration pressure in the glomerulus? NFP
Pc = capillary hydrostatic pressure (filtration): 55 mmHg
Pf = glomerular capsule fluid hydrostatic pressure (absorption): 15 mmHg
πc = capillary colloid osmotic pressure (absorption):
NFP = Pc- πc - Pf
or
NFP = Pc - (Pf + πc)
Pc = out
Pf+πc = in
What is the net driving force pressure in the direction favoring filtration?
10 mmHg
GFR is relatively constant over a wide range of blood pressures...explain.
As long as mean arterial blood pressure remains between 80 and 180 mmHg, GFR averages 180L/day
What is GFR primarily controlled by?
regulation of blood flow through the renal arterioles
if overall resistance of renal arteriole increases, renal blood flow decreases, and blood is diverted to other organs.
Effect of increased resistance on GFR depends on WHERE the resistance change takes place.
What is the general rule for GFR in the afferent arteriole?
it has a direct relationship with NFP
increase blood flow into glomerulus --> increase GFR
decrease blood flow into glomerulus --> decrease GFR
why?
NFP = PC - (PF + πC)
Alter capillary hydrostatic pressure (PC)
What happens if you vasodilate the afferent arteriole?
Vasodilate afferent → ↓ resistance → ↑ flow in afferent → ↑ pressure (PC) → ↑ filtration rate
What happens if you vasoconstrict the afferent arteriole?
Vasoconstrict afferent → ↑ resistance → ↓ flow in afferent → ↓ pressure (PC) → ↓ filtration rate
blood follows the path of least resistance and pressure dissipated in overcoming resistance
What is the general rule for GFR for the efferent arteriole?
indirect relationship with NFP
decreased blood flow out of glomerulus --> increased GFR
increased blood flow out of glomerulus --> decreased GFR
Why?
NFP = PC - (PF + πC)
Alter capillary hydrostatic pressure (PC)
What happens if you vasoconstrict the efferent arteriole?
↑ resistance → ↓ flow in efferent → ↑ pressure (PC) → ↑ filtration rate
- Blood backs up
What happens if you vasodilate the efferent arteriole?
Vasodilate efferent → ↓ resistance → ↑ flow in efferent → ↓ pressure (PC) → ↓ filtration rate
- Blood drains
What is autoregulation of glomerular filtration rate?
local control process in which the kidney maintains a relatively constant GFR in the face of normal fluctuations in BP.
(maintains GFR w/MAP variability: 80-180mmHg)
myogenic response
tubuloglomerular feedback
What is the myogenic response?
intrinsic ability of vascular smooth muscle to respond to changes
same as any arteriole
↑ blood flow → ↑ smooth muscle stretch → ↑ Ca2+ influx
if BP decreases, contraction disappears and arteriole becomes maximally dilated....but vasodilation is not as effective at maintaining GFR as vasoconstriction because normally the aff. arteriole is fairly relaxed.
Consequently, when MAP drops below 80 mmHg, GFR decreases - which helps body conserve blood volume
What is Tubuloglomerular feedback?
paracrine signaling mechanism through which changes in fluid flow through the loop of Henle influence GFR
the macula densa monitors Na+ in filtrate as a measure of GFR
↑ Na+ in filtrate → ↑ paracrine release → afferent arteriole vasoconstriction → ↓ GFR
How does the sympathetic system control GFR?
through the use of NE and E and alpha adrenergic receptors
Smooth muscle contraction → vasoconstriction → ↓ GFR
What hormones control GFR?
angiotensin II
prostaglandins
atrial natriuretic peptide (ANP)
How does Angiotensin II control GFR?
Causes Vasoconstriction → ↓ GFR
↓ filtration coefficient → ↓ GFR
How do prostaglandins influence GFR?
Vasodilation → ↑ GFR
↑ filtration coefficient → ↑ GFR
How does ANP influence GFR?
Vasodilation → ↑ GFR
↑ filtration coefficient → ↑ GFR
What is the process of reabsorption?
basic processes of nephron = remove then absorb
Filtration: 180L/day, 300 mOsm
excretion: 1.5L/day, 50-1200 mOsm
Why go so overboard?
- filtration is fast
- reabsorb to homeostatic balance
- only reabsorb what is needed, excrete the rest