Strand 10- Nerves and Muscles
1/127
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
128 Terms
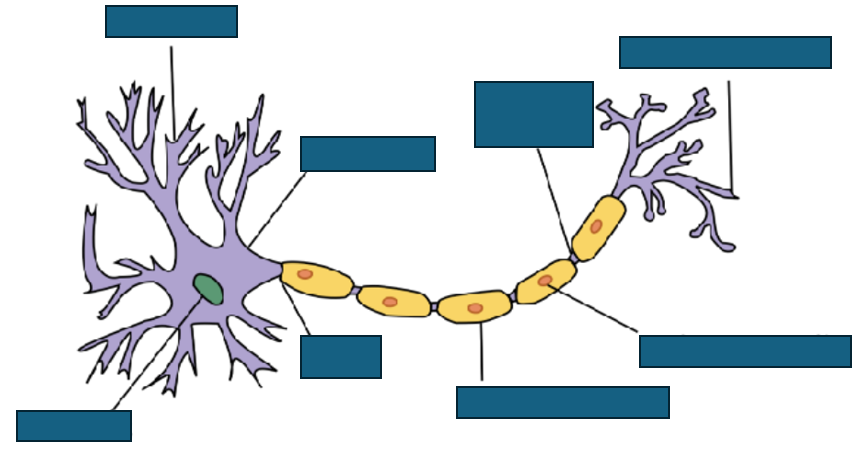
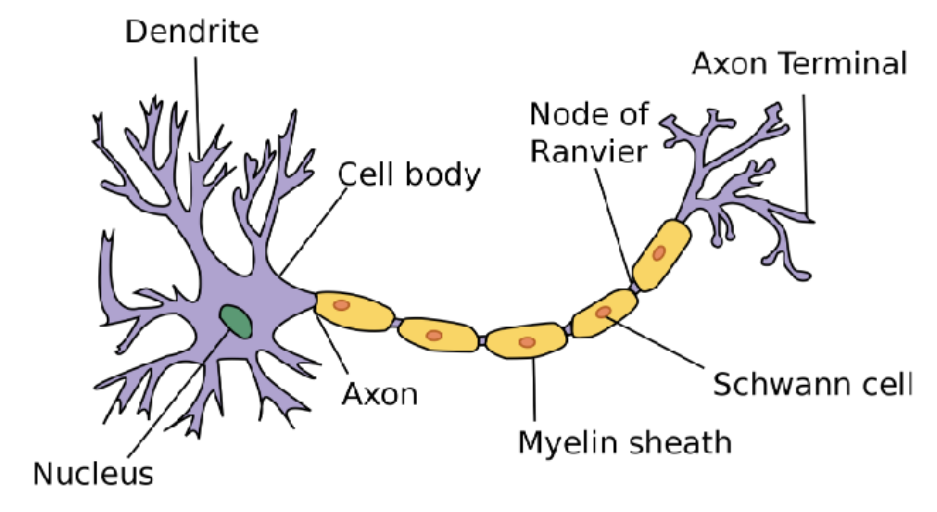
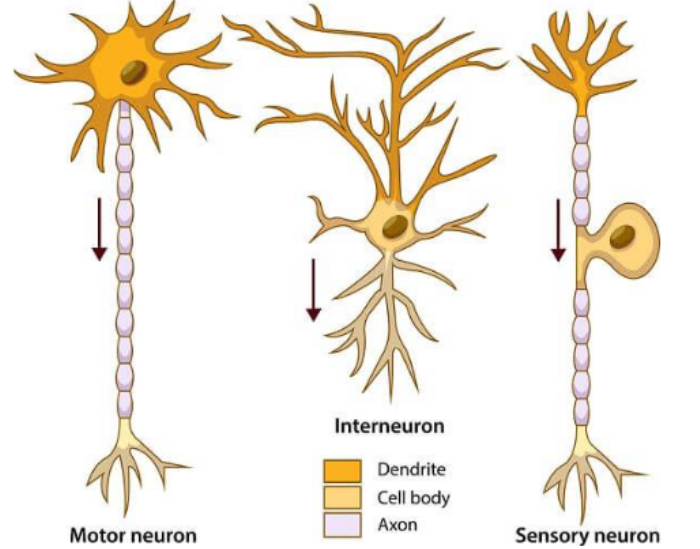
general neuron structure
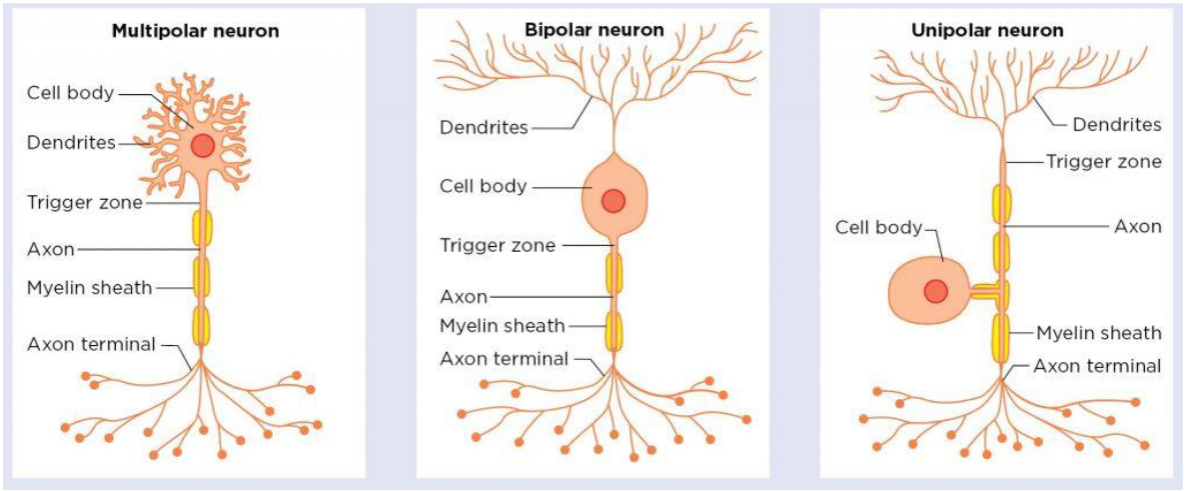
structural classification of neurones
describes relationship of cell body and processes
multipolar neuron→ cell body has lots of dendrites (processes)
bipolar neuron→ 2 main processes (axon and main dendrite)
unipolar neurone→ One process
functional classification of neurones
describes function of cell in system:
motor neuron→ carries to effectors
interneuron→ sit between sensory and motor neurons
sensory neuron→ detecting sensory stimuli
classification of nervous system
central nervous system:
Brain
Spinal cord
Peripheral nervous system:
Autonomic
sympathetic
parasympathetic
somatic
autonomic nervous sytem
regulates involuntary processes e.g. heart rate, respiration, digestion, pupil contraction
operates automatically without conscious direction
somatic nervous system
carriers sensory info from sensory organs to CNS and relays motor commands to muscle→ control voluntary movements
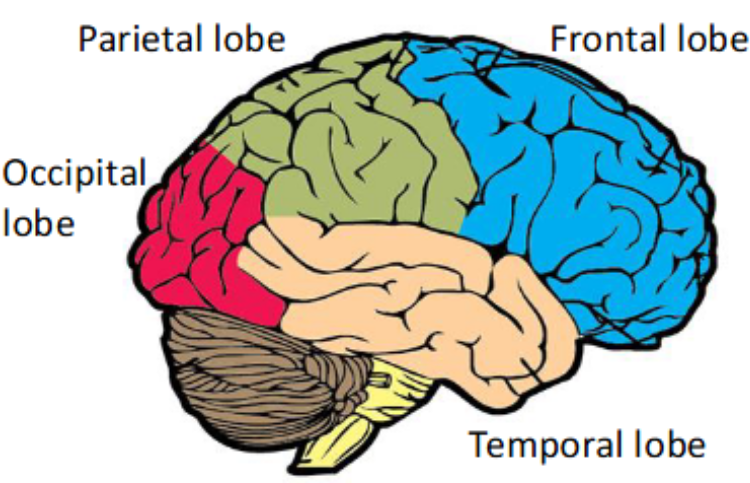
brain within the nervous system
divided into 3 major parts:
fore brain
mid brain
hind brain
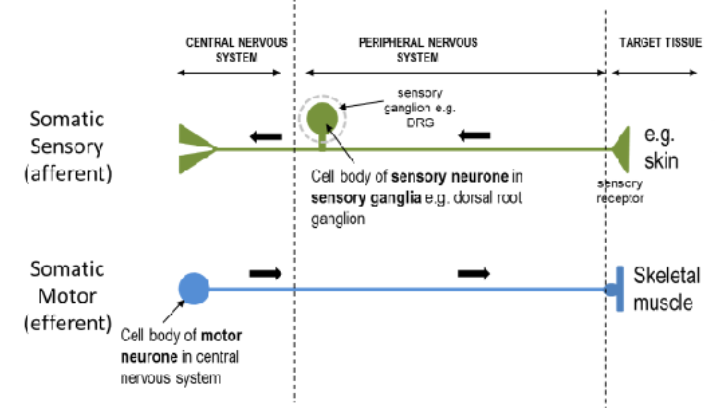
central vs peripheral nervous system
CNS→ brain and spinal cord
peripheral nervous system→ nerves and ganglia outside brain and spinal cord
PNS links CNS to rest of body
CNS- nuclei and tracts
neuronal cell bodies reside in nuclei and cortex→ grey matter
tracts contain axons→ white matter
CNS-meninges
3 membranes that overlie brain and spinal cord:
outer→ dura mater
mid→ arachnoid mater
inner→ pia mater
clinical relevance
infection (meningitis)
bleeds (extradural, subdural, subarachnoid)
tumours (meningioma, metastasis)
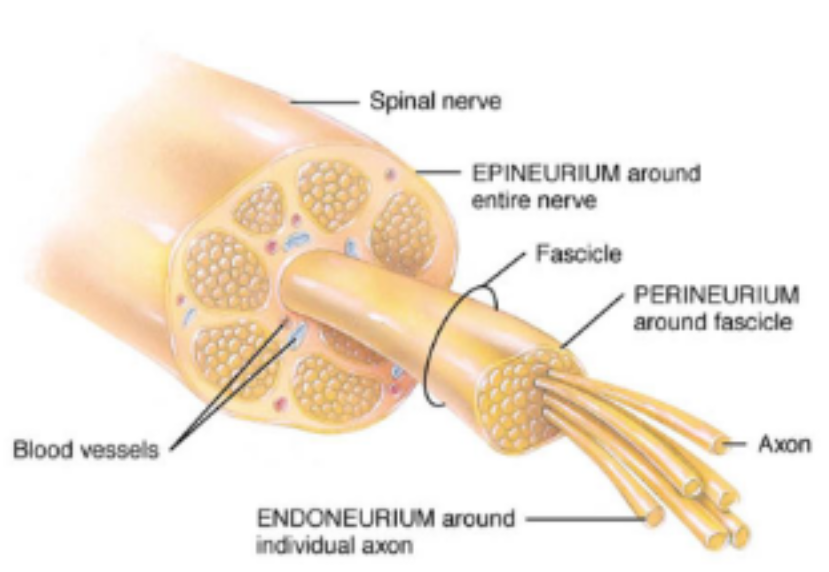
PNS- spinal nerves
31 pairs of spinal nerves:
cervical nerves→ C1-C8
thoracic nerves→ T1-T12
Lumbar nerves→ L1-L5
Sacral nerves→ S1-S5
coccygeal nerve→ C0
arrangement of nerves in spinal cord
cranial nerves
areas innervated by somatic nervous system
dermatones→ show areas of skin supplied by one spinal nerve
myotomes→ muscle groups innervated by one spinal nerve
somatic pathways
somatic sensory→ afferent:
target tissue to central nervous system
somatic motor→ efferent:
CNS to effector
sympathetic nervous system vs parasympathetic nervous system
sympathetic→ fight or flight
parasympathetic→ rest and digest
autonomic pathways
preganglionic neurone in CNS→ postganglionic neurone in PNS
preganglionic neurones:
thoracic and lumbar segments of spinal cord in sympathetic
sacral spinal cord and brain stem in parasympathetic
glial cells
non-neuronal cells in CNS and PNS
have different glia
Many roles:
myelin formation
nutritional support
structural support
some have immune functions
astrocytes
central nervous system
many roles:
metabolic support for neurons
structural support
form blood-brain barrier with capillaries
repair following injury→ glial scar
oligodendrocytes
form myelin sheaths in CNS
one oligodendrocyte can myelinate multiple axons
clinical important as site of damage in demyelinating diseases such as multiple sclerosis
CNS- microglia
resident immune cells of CNS→ related to macrophages
respond to infectious agents
perform general maintenance:
clear up damaged neurons
prune unnecessary synapses
scavenge amyloid plaques
CNS- ependymal cells
lining cells of ventricular system of the brain and central canal of spinal cord
ciliated surface aids flow of cerebrospinal fluid
modified ependymal cells contribute to CSF production at choroid plexus in ventricles
PNS-schwann cells
support neurons in PNS
responsible for myelin formation in PNS
some Schwann cells provide support without forming myelin→ ‘non myelinating’ schwann cells
PNS- satellite cells
surround cell bodies in sensory, sympathetic and parasympathetic ganglia
suggested to regulate extracellular environment of neurons in ganglia
express various ion channels and transporters for neurotransmitters
myelination
increases conduction velocity→ allows saltatory conduction
Ion channels concentrated at nodes of Ranvier to regenerate signal
lowers total charge transfer needed to conduct action potential→ reduces work the neuron must do to maintain electrolyte balance
nerve fibre classification
Aα:
largest diameter
fastest transmission
sensory receptor: proprioceptors of skeletal muscle
Aβ:
second largest diameter
second fastest transmission
receptor: mechanoreceptors in skin
Aδ:
second smallest diameter
second slowest transmission
receptor: pain temperature
C:
smallest diameter
slowest transmission
receptor: temperature, pain, itch
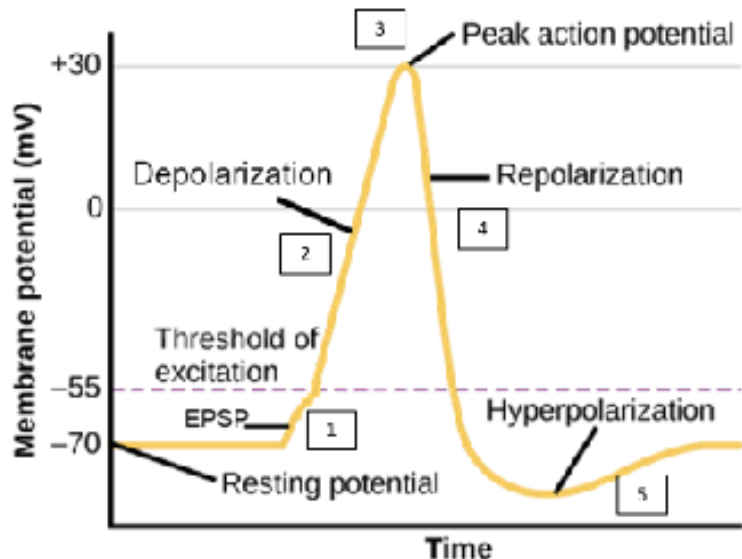
resting membrane potential
-70mV
what determines the resting membrane potential
difference in concentrations of Na+ and K+ ions:
very little Na+ moves into cell via leaky Na+ channels down EC gradient
a lot of K+ moves outside of cell via K+ leaky K+ ion channels
sodium potassium ATPase pump→ 3Na+ out, 2K+ in
action potential generation
excitatory stimulus depolarises membrane→ membrane potential increases
crosses threshold value→ -55mV
Voltage gate Na+ channels open allowing Na+ into cell→ more positive
results in depolarisation to about +30mV
voltage gates Na+ channels start to inactivate
At the same time, K+ VG channels open→ K+ out
membrane potential starts to decreases→ repolarisation
small overshoot due to excess K+ efflux causes hyperpolarisation
K+ channels close and Na+ channels closed
Na+/K+ ATPase restores Na+/K+ gradient across membrane
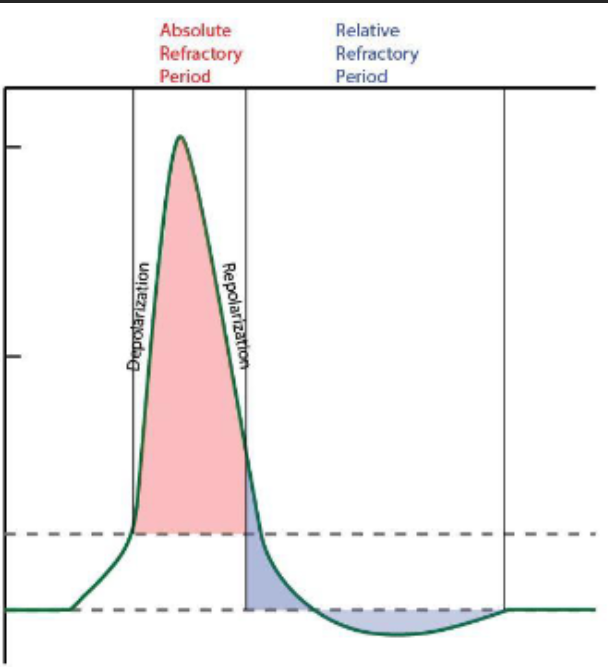
stages of voltage gated Na+ channel
3 stages:
open
closed
inactive
has inactivation gate that blocks Na+ influx shortly after depolarisation→ stays in this state until cell repolarises and enters closed state again
action potential refractory period
absolute refractory period→ cell is incapable of repeating an AP in that part of the membrane
ensures action potential travels in one direction
during relative refractory period, larger stimulus can result in action potential in this area of the membrane
nature of action potential
all or nothing:
nerve membrane has to be depolarised beyond threshold for action potential to be generated
further increase above threshold→ higher AP frequency not larger AP amplitude
a neurone either fires AP or does not, regardless of signal size→ all or nothing
propagation of action potential down non-myelinated neurones
in response to signal, soma end of axon becomes depolarised
depolarisation spreads down axon
meanwhile, first part of membrane depolarises:
Na+ and K+ channels are inactivated and additional K+ channels have opened→ membrane cannot depolarise again
action potential continues to travel down axon
propagation of action potentials down myelinated axons
Na+ channels locally open in response to stimulus→ generates action potential here
depolarising current passively flows down the axon
nodes of Ranvier are only areas where current can pass through membranes and only areas where membrane depolarises
impulse travels in jumps from one node to the next→ saltatory conduction
temporal and spatial summation
spatial→ signals coming from multiple simultaneous inputs from a number of presynaptic neurones
temporal→ comes from repeated inputs from presynaptic neurone
motor neurone disease
Amyotropic lateral sclerosis→ prevalent form
fatal disease of nervous system→ progressive voluntary muscle weakness and paralysis
selective for somatic neurones→ sensory and autonomic function remains intact
mind and memory unaffected
starts with degradations of upper and lower motor neurones→ messages that originate in motor cortex don’t reach muscles to trigger voluntary contractions
nerve death causes innervating muscles to shrink and waste away
cause of motor neurone disease
exact cause unknown
excessive levels of glutamate (neurotransmitter) in synapse cause motor neurones to become overexcited→ damage and death
build up of glutamate is doe to loss of glutamate transporters (EAAT2)→ ‘mop’ up glutamate in synapse
toxicity due to Ca2+ flooding the cell
prolonged Ca2+ inside cell causes damage and can activate programmed cell death
myelination
myelin→ insulating layer around nerve axon in CNS and PNS
consists of protein and fatty substances→ speeds up transmission along axon
In CNS→ oligodendrocyte is responsible for myelination of axon:
cells extend processes that wrap around the axons to form myelin sheath
one can myelinate 3-50 neurones
PNS→ myelin sheath formed by Schwann cells→ one Schwann cell provides myelination for one axon
demyelinating disease
results in damage to myelin sheath
nerve impulses slow/stop→ deficiency in sensation, movement, cognition, other functions
axonal degradation and often cell body degeneration
usually secondary to inflammation
classification of demyelinating diseases
classified on basis of cause
demyelinating leukodystrophic diseases- primary:
myelin is abnormal and degenerates→ genetics responsible
demyelinating myelinoclastic diseases- secondary:
healthy myelin destroyed by toxin, infectious agent, chemical or autoimmune substance
multiple sclerosis
most common demyelinating disease of CNS→ sensory and motor neurones affected
autoimmune degenerative nerve disorder→ immune system attacks myelin sheath
results in multiple areas of scarring (sclerosis)→ impedes nerve signalling
symptoms vary widely from person to person and can affect any part of the body:
difficulty walking
blurred vision
numbness or tingling in parts of body
problems with balance and coordination
problems with thinking, learning and planning
cause of multiple sclerosis
exact cause is unknown
viruses trigger autoimmune attack in susceptible individuals via molecular mimicry
structural similarity between foreign and self molecules of mammalian host
resulting in production of autoreactive T cells and antibody producing B cells which attack host as well as foreign body
Guillain-Barre syndrome
demyelinating disease of PNS
myelin and schwann cells around sensory and motor neurones destroyed:
conduction block and axonal degeneration
autoimmune disease often triggered by preceding viral/bacterial infection e.g. cytomegalovirus, Epstein-Barr virus, COVID
symptoms: symmetrical ascending muscle weakness and paraesthesia in arms and legs, loss of sensation, autonomic dysfunction
stimulus detection
sensory receptors→ modified nerve ending of sensory neurones
tuned to detect specific signals→ sensory modalities
types of receptors
Mechanoreceptors→ touch, pressure, vibration, stretch
thermoreceptors→ hot, cold, temperature change
photoreceptors→ light
chemoreceptors→ chemicals
nociceptors→ pain (usually chemicals)
pacinian corpuscle
found around the ends of sensory neurones→ pressure detectors
consists of layers of connective tissue with gel in between→ gel has Na+ ions
sensory neurone ending contains stretch mediated Na+ ion channels→ open when corpuscle is deformed by pressure
when open→ Na+ from gel can flow into neurone, generating small depolarisation in sensory neurone ending- generator potential
If large enough, receptor potential leads to action potential being generated and fired off along the sensory axon towards the CNS
receptor potentials (generator potentials)
graded potentials→ size determined by size of stimulus
can summate to give rise to an action potential in the neurone
depolarising event resulting from an inward current flow e.g. Na+
influx of current can bring membrane potential of sensory receptor towards threshold for triggering action potential
muscle proprioreceptors
sensory receptors in muscles
muscle spindle located within muscle and stimulated when muscle is passively stretched
when a muscle is passively stretched the spindle is activated and initiates a reflex causing the muscle to contract
protects muscle being overstretched
golgi tendon organ
located in the tendon→ responds to excessive tension (stimulated when associated muscle contracts)
when stimulated, it causes its associated muscle to relax by interrupting its contraction
prevents tendon from tearing and muscle damage
reflex arc
autonomic and rapid response to stimulus→ minimises damage to body from potentially harmful conditions
components of a reflex arc
receptor
sensory neuron
interneuron
motor neuron
effector
muscle spindle- stretch reflex
stretching of muscle activated spindle→ increased discharge of sensory afferent (1a) neurone
results in increased firing of motor neurone to muscle that is stretched→ contracts
no spinal neurone involved
contraction usually accompanied by simultaneous reflex inhibition of antagonistic muscle
effect→ dampens stretch of muscle to protect it
muscle spindle reflex- maintaining muscle tone
weight of fluid in glass→ bicep stretches
afferent signals from muscle spindle relayed to motor neurone in spinal cord
efferent signals sent back to muscle to cause it contract
since muscles are always under some degree of stretch, reflex circuit normally responsible for steady state level of tension in muscles→ muscle tone
golgi tendon reflex
excess tension in tendon caused by muscle contraction is detected in golgi tendon organ
GTO sends sensory signals along sensory afferent (1b) to CNS
results in reflex inhibiting the muscle from contracting
usually accompanied by reciprocal contraction of antagonistic muscle
effect is to reduce tension in tendon→ protects it
golgi tendon reflex in action
amount of tension generated in tendon by bicep increases with each increasing weight→ rate of GTO firing increases
at some point, excessive GTO firing occurs→ indicated no more force should be generated by muscle otherwise tendon connecting muscle to bone might tear
GTO reflex interrupts contraction causing muscle to relax
synapses
neurones communicate via synapses
two types:
electrical
chemical
electrical synapse
direct physical connection between pre and post synaptic neurone
connection takes form of channel→ gap:
allows current (ions) to flow directly from one cell into another
transmit signals more rapidly than chemical synapses
bidirectional transmission
enable synchronised activity of groups of cells→ epileptogenic
gap junction
formed by coming together of subunits called connexons→ present in both pre and post synaptic membranes
pores of channels connect to one another, creating electrical continuity between two cells
connexons themselves are made of 6 protein units→ connexins
chemical synapse
connections between two neurones or between neuron and non-neuronal cell e.g. muscle cell at NMJ
one neuron releases chemical substance→ neurotransmitter
neurotransmitter binds to receptors on postsynaptic cell and depending on nature of neurotransmitter it can excite or inhibit post synaptic cell
neurotransmitters cleared from synapse by:
enzymatic digestion
reuptake by specific transporters on presynaptic cell or adjacent glial cell
diffuse out of synapse
types of post synaptic receptors
ionotropic
metabotropic
ionotropic receptors
transmembrane ion channels
open/close in response to binding of neurotransmitter
ligand gates ion channels
fast acting
cause immediate change in membrane potential
e.g. nAChR
metabotrpic receptors
require G proteins
G-protein coupled receptors
second messengers to indirectly modulate ionic activity in neurones
generally slower, more persistent response
e.g. mAChR
neurotransmitters
substance that is released at a synapse by one neurone that affects another cell, either neuron or effector organ in a specific manner
classified either by structure or function
types of neurotransmitters
excitatory→ promotes AP generation in post-synaptic cell e.g. glutamate, ACh
inhibitory→ reduce electrical excitability at post synaptic membrane, preventing generation and propagation of AP e.g. GABA, Glycine
chemical groups of neurotransmitters
acetylcholine
biogenic amines
peptide neurotransmitters
amino acid neurotransmitters
biogenic amines
serotonin
dopamine
adrenaline
noradrenaline
histamine
peptide neurotransmitter
endorphins
substance P
amino acids neurotransmitters
glutamate
gamma-aminobutyric acid (GABA)
glycine
other neurotransmitters
nitric oxide
ATP
CO
function of acetylcholine
found in motor neurones at NMJ
involved in body movement, learning, memory
involved in parasympathetic NS
Glutamate
major excitatory neurotransmitter
involved in learning, memory
gamma-aminobutyric acid
major inhibitory neurotransmitter
plays major role in controlling nerve cell hyperactivity (often occurs in stress, anxiety, fear)
dopamine
reward and pleasure pathways
noradrenaline
cardiovascular system
alertness
arousal
decision making
attention
adrenaline
fight or flight response
homeostasis
serotonin
sleep
appetite
mood regulation
components of a motor unit
motor unit→ all the skeletal muscle fibres innervated by a single motor neurone
when motor neurone fires AP, all muscle fibres that it innervates contract within the unit at the same time
size of motor unit dependant on function of muscle
how do motor units differ in different sites of the body
most fibres= most force
thigh muscles can have thousands of muscle fibres in each motor unit
smaller muscles have few muscle fibres in each motor unit→ enables fine precision
synapse between motor neurone and muscle cell→ neuromuscular junction
a motor neurone innervating several muscles cells will have many axon terminals forming NMJs
neuromuscular junction
chemical synapse between motor neurone and muscle fibre
site of transmission of action potentials from nerve to muscle
1:1 transmission→ ensures that every presynaptic action potential results in a postsynaptic one
unidirectional process
has inherent time delays
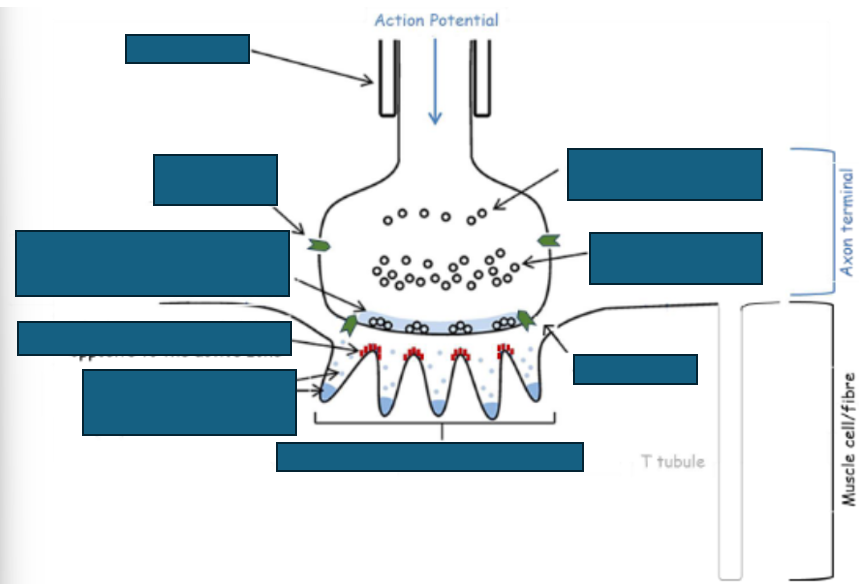
functional anatomy of neuromuscular junction
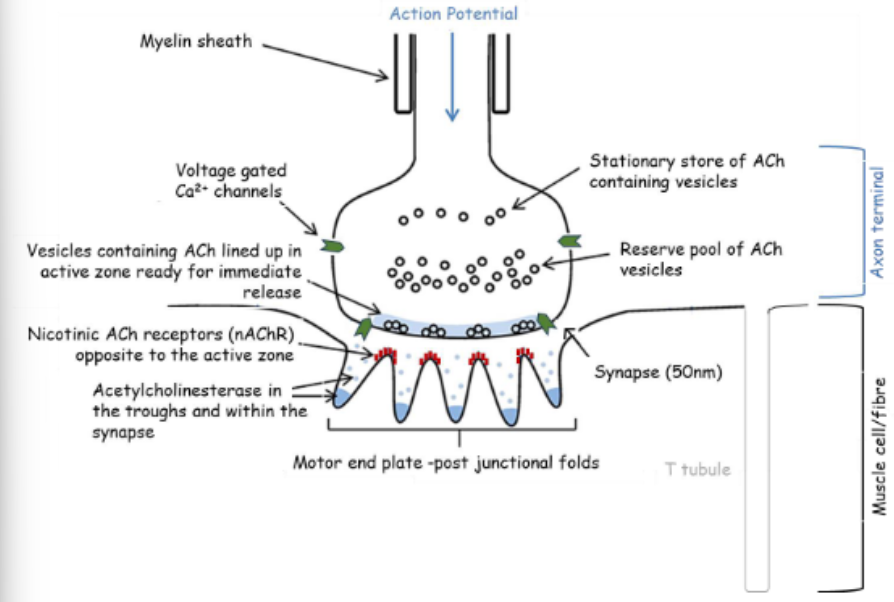
resting neuromuscular junction
once every second, one synaptic vesicle randomly fuses with presynaptic terminal and release its content of ACh into synapse
ACh binds to nAChR opening up Na+ channels
entry of Na+ across muscle membrane produce small depolarisation (0.4 mV)→ MEPP
activated neuromuscular junction
arrival of AP causes depolarisation of axon terminal
voltage gated Ca2+ channels open
Ca2+ enter causing fusion of vesicles with presynaptic terminal and release of ACh
several quanta of ACh release into synapse where they activate numerous nAChR
Na+ channels and depolarisation of muscle membrane
each quantum can generate MEPP in muscle membrane, several quanta will lead to EPP forming
if EPP can depolarise muscle membrane to threshold, it triggers AP
excitation contraction coupling
links excitation of muscles by nervous system to their mechanical contraction
EPP triggers AP in the muscle membrane
AP propagated along muscle membrane→ depolarisation passes down T-tubules
within T tubules depolarisation is sensed by DHP receptors
once activated, DHP receptors stimulate opening of ryanodine receptors (RyR) on sarcoplasmic reticulum→ Ca2+ released into cytoplasm
Ca2+ causes muscle contraction
removal of acetylcholine from the synapse
ACh binds briefly to nAChR on postsynaptic cell
following dissociation from receptor, ACh is rapidly hydrolysed by acetylcholinesterase
hydrolyses ACh to acetate and choline
choline recycled back into presynaptic terminal to make more ACh
acetate diffuses into surrounding medium
some ACh will just diffuse out of synaptic cleft
SARIN
acetylcholinesterase inhibitor
acetylcholine cannot be broken down
strcuture of nicotinic acetylcholine receptor (nAChR)
ACh-gated Na+ channel
made up of 5 polypeptide subunits:
2 alpha subunits
one beta subunit
one gamma subunit
one delta subunit
2 ACh molecules required to stimulate receptor→ binding surface of receptor appears to be primarily on the alpha subunits near outer surface of molecule
ACh binding to receptor causes Na+ influx→ membrane depolarisation
nAChR at autonomic ganglia and in brain have different subunit composition
neuromuscular blockade
many drugs produce muscle paralysis by affecting ACh receptors e.g. succinylcholine
used during surgery
use of muscle relaxants requires patient to be artificially ventilated
selective neuromuscular blockade
several compounds which selectively block NMJ
botulinum toxin prevents exocytosis of ACh from synaptic vesicles→ no ACh released and muscle does not contract
toxin marketed as botox
can be used to help patient with strabismus (cross eye), blepharospasm (eyelid spasms) or cerebral palsy
cosmetic uses helps reduce appearance of fine lines and wrinkles
myasthenia gravis
autoimmune response→ antibodies competitively inhibit nAChR on motor end plate→ NMJ less responsive to ACh→ muscle weakness
Symptoms:
Muscle weakness that increase during periods of activity and improves after rest
eye related issues as initial symptom:
ptosis→ eyelid drooping
diplopia→ double vision
symptoms involving face and throat muscles:
altered speech
difficulty swallowing (dysphagia), chewing
loss of facial expression
20-25% of patients with thymoma also have myasthenia gravis
pathology at NMJ for myasthenia gravis
antibodies against ACh receptor block receptors on postsynaptic membrane
also get accelerated degradation of nACh receptor
reduction of nACh receptors at motor endplate and flattening of postsynaptic folds reduced EPP even though normal amounts of ACh released
reduced neuromuscular transmission→ reduced AP production on motor end plate
treatment of myasthenia gravis
long term acting anti-cholinesterase→ prevent breakdown of ACh- more ACh available in synapse to compete with antibodies
immunosuppressives→ steroids
surgical thymectomy
lambert-eaton myasthenic syndrome
autoimmune disease
antibodies formed against voltage-gated Ca2+ on presynaptic nerve terminal at NMJ- prevent ACh release
many people also have small lung cancer
symptoms:
weakness in muscle limbs
fatigue
autonomic dysfunction (e.g. dry mouth, blurred vision)
symptoms almost always precede detection of cancer
pathology of lambert-eaton at NMJ
antibodies disrupt function of Ca2+ channels on presynaptic neuron→ block Ca2+ influx
Ca2+ entry during depolarisation important for ACh release into synapse
Reduced Ca2+ influx→ reduces ACh release from presynaptic membrane→ reduced muscle activation→ muscle weakness
treatment of lambert-eaton
treatment of underlying malignancy resolves symptoms
use immunosuppressants
use K+ channel blocker e.g. amifampridine:
blocks VG K+ channels on presynaptic nerve
delays repolarisation→ prolongs depolarisation of presynaptic membrane→ enhances Ca2+ entry through channel into terminal→ facilitates ACh release
types of muscle
skeletal
smooth
cardiac
skeletal muscle
striated
multinucleated
attached to skeleton→ involved in movement
controlled voluntarily by somatic NS
smooth muscle
not striated
single nucleus
found in walls of organ, glands and blood vessels→ controlled involuntarily by ANS
cardiac muscle
striated
generally uninucleated
branched network
controlled involuntarily by ANS
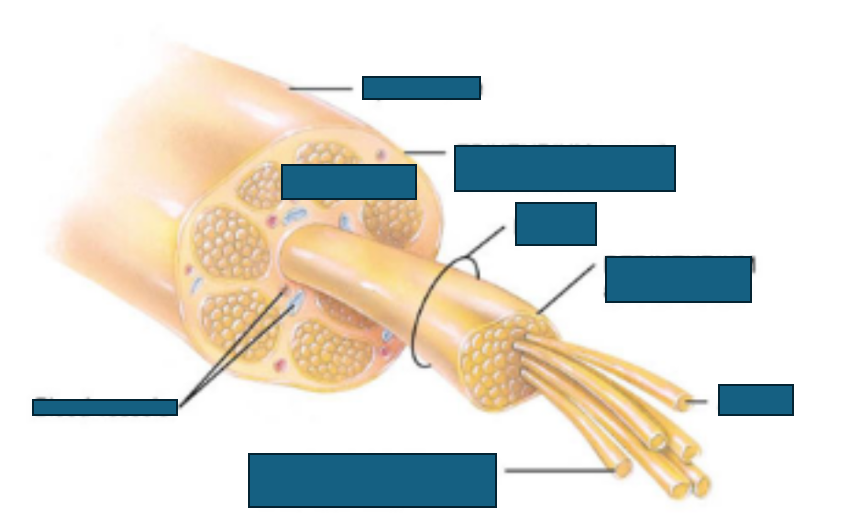
structure of skeletal muscle
3 layers of connective tissue:
epimysium→ covers entire muscle
perimysium→ around each fasciculus
endomysium→ within each fasciculus
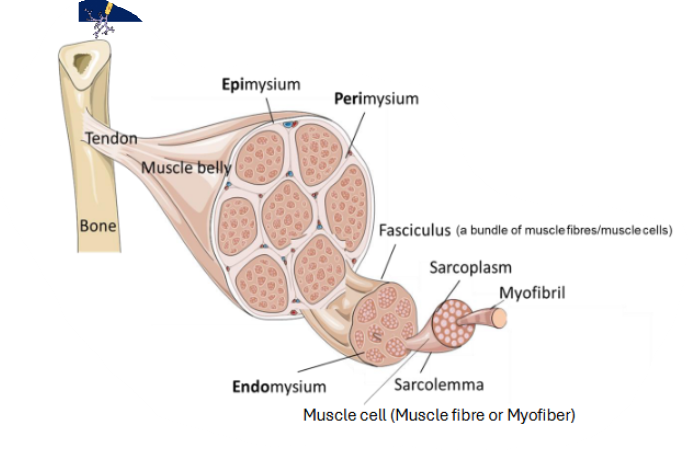
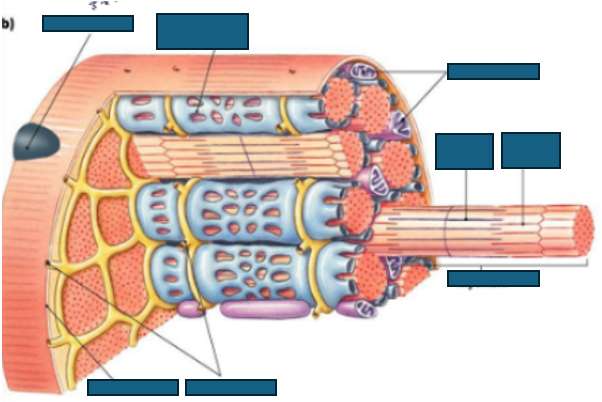
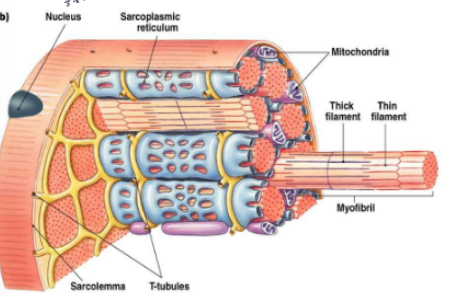
structure of a skeletal muscle fibre
sarcolemma→ muscle plasma membrane
sarcoplasmic reticulum→ smooth endoplasmic reticulum in muscle fibre- stores Ca2+
transverse tubules→ carry action potentials deep into muscle fibre