Autonomic Nervous System
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Autonomic Nervous System
component of the peripheral nervous system
It regulates involuntary physiologic processes: HR, BP, pupil diameter, Respiration, Digestion and Excretion, Glandular activity, Renal function, Conversion glycogen to glucose
Some features include: High-level integration in the brain, the ability to influence processes in distant regions of the body, Extensive use of negative feedback
Controls Sympathetic Nervous System and Parasympathetic Nervous System
Preganglionic Fibers
The ANS consists of neurons that give rise to prepanglionic fibers and other neurons that give rise to postganglionic fibers
Originate from cells located in the brainstem or spinal cord and project to a ganglion
All preganglionic fibers use acetylcholine (ACh) as their neurotansmitter
Preganglionic gibers of the sympathetic NS exit the CNS from thoracic, lumbar, and sacral regions of the spinal cord
Preganglionic fibers of the parasympathetic NS exit the CNS via the cranial nerves, particularly nIII, nVII, nIX, and nX
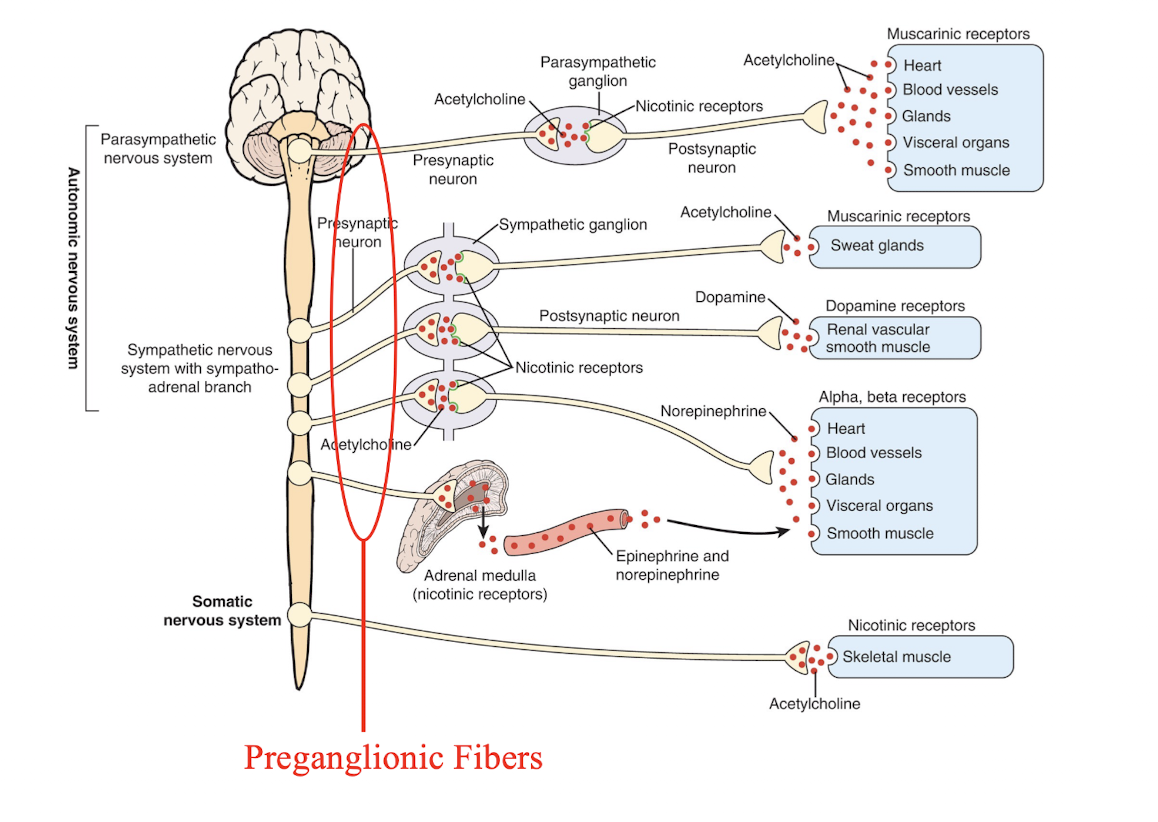
Ganglion
collection of nerve cell bodies
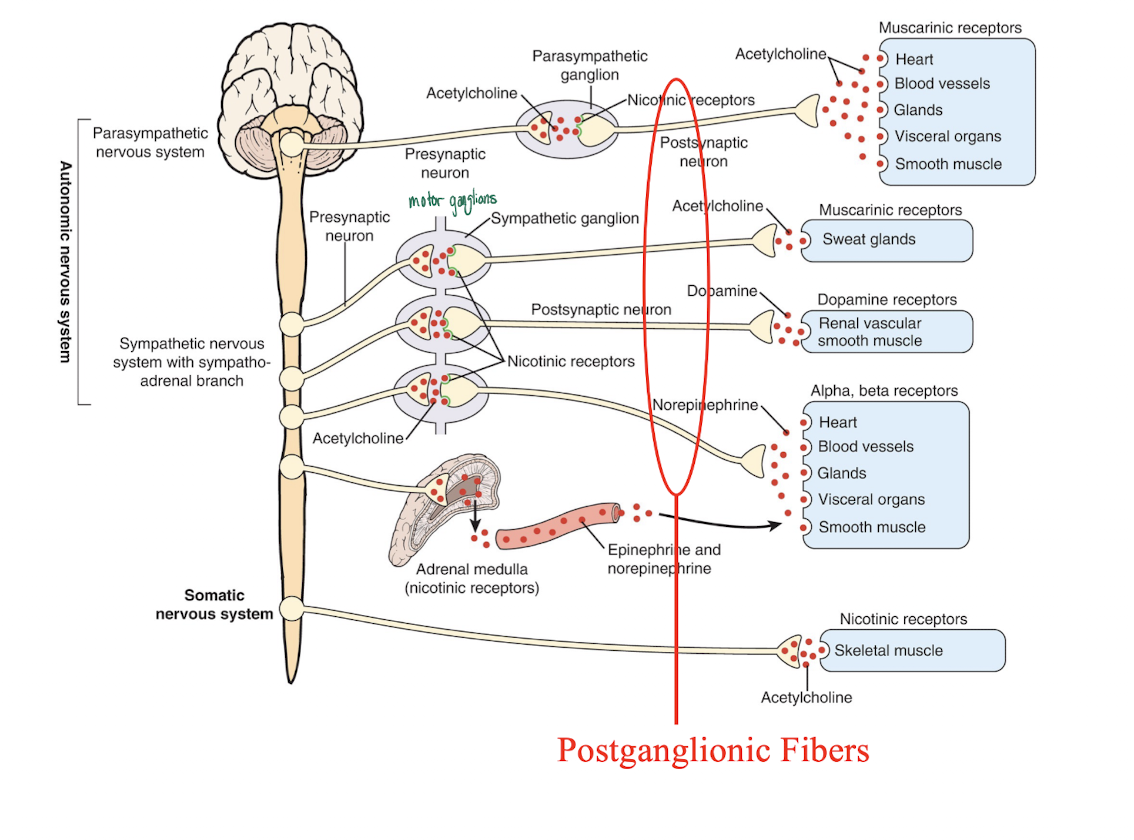
Postganglionic Fibers
Postganglionic fibers of the sympathetic NS originate from ‘ganglia’ located either in a ‘chain’ next to the spinal cord (paravertebral) or located along the midline in front of the heart and spinal column (prevertebral)
These fibers project to the end organs
Postganglionic fibers of the parasympathetic NS originate from cells located near the end organ
Anatomic and Neurotransmitter Features of Autonomic and Somatic Motor Nerves
The adrenal medulla, a modified sympathetic ganglion, receives sympathetic preganglionic fibers and releases epinerphrin and norepinephrine into the blood which goes the the tissue and muscles
Cholinergic nerves are shown in blue
Noradrenergic are shown in red
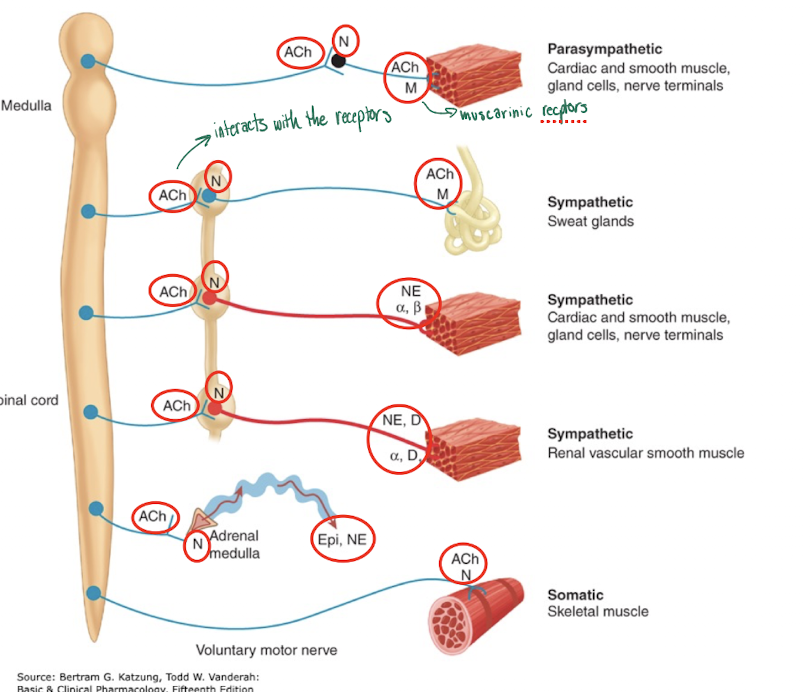
Parasympathetic: Cardiac and smooth muscle, gland cells, nerve terminals
acetylcholine goes to the nicotinic receptors which sends acetylcholine to the muscarinic receptors of the cardiac and smooth muscle, gland cells, nerve terminals
Sympathetic: Sweat glands
Spinal cords sends acetylcholine to the nicotinic receptors which sends acetylcholine to the muscarinic receptors of the sweat glands
Sympathetic: Cardiac and smooth muscle, gland cells, nerve terminals
Spinal cord sends acetylcholine to nicotinic receptors which send norepinephrine to adrenergic receptors on cardiac and smooth muscle, gland cells, nerve terminals
Sympathetic: Renal vascular smooth muscle
Spinal cord sends acetylcholine to nicotinic receptors which send norepinephrine and dopamine to adrenergic receptors on renal vascular smooth muscle
Neurotransmitters
Preganglionic fibers of both the SNS and PNS use acetylcholine as their neurotransmitter. The ACh acts on nicotinic receptors located on the ganglion cells
Most postganglionic fibers of the SNS use norepinephrine (NE) as their neurotransmitter. NE acts on adrenergic receptors located in the end organs. One exception is SNS innervation of sweat glands which uses ACh
Postganlionic fibers of the PNS use ACh as their neurotransmitter. The ACh acts on muscarinic receptors located in the end organs
Neurotransmitter Receptors
Each neurotransmitter can bind to multiple receptor subtypes
Subtypes are organized into families and are classified as ‘type’ according to pharmacological effects and mechanism of action
Ionotropic Receptors
Form ion channel, activation alters membrane conductance, will cause ion channel to open changing membrane potential
Metabotropic Receptors
Act through G-proteins, Can activate or inhibit second messenger systems, also can be associated with an ion channel
Adrenergic Receptors
All are metabotropic receptors, act through G-protein
Have multiple receptor subtypes
Subtypes of Adrenergic Receptors
The natural ligand for adrenergic receptors is norepinephrine
The 2 main groups of adrenergic receptors, alpha and beta and at least 9 subtypes in total
All are metabotropic
Alpha receptors are divided into alpha1 (Gq-coupled) and alpha2 (Gi-coupled)
Alpha1 has 3 subtypes- a1A, a1B, and 1D
Alpha2 has 3 subtypes- a2A, a2B, a2C
Beta receptors are divided into b1, b2, and b3
All couple with Gs, but b2 and b3 also can couple with Gi
Mechanism of Action of Adrenergic Receptors
Epinephrine or norepinephrine are receptor ligands to either a1, a2, or b adrenergic receptors
a1- Smooth muscle contraction, increases BP
a2- Inhabitation of NE, release/sympathetic tone
b- Heart muscle contraction, smooth muscle relaxation, glycogenolysis
b1- Increase cardiac output, BP
b2- Smooth muscle relaxation
Alpha-1 receptor
Vasoconstriction
Increase peripheral resistance (blood flow)
Increase BP
Mydriasis
Increase Closure of bladder sphincters
Norepinephrine is more potent than epinephrine
Alpha-2 receptors
Inhibits Norepinephrine release
Inhibits acetylcholine release
Inhibits insulin release
Inhibits neurotransmitters
Decreases sympathetic, put brain sleep
Epinephrine is more potent than Norepinephrine
Beta-1 receptors
Increase HR
Increase lipolysis
Increase myocardial contractility
Increase Renin
Located mainly in the heart
Activation of SNS
Increase BP
Increase vasoconstriction
Epinephrine is equal to norepinephrine in potency
Beta-2 Receptor
Vasodilation
Decrease Peripheral resistance, blood flow
Increase Glycogenolysis, muscle and liver
Bronchodilation- smooth muscle relaxes
Increase Glucagon release
Relaxes uterine smooth muscle
Epinephrine is more potent than Norepinephrine
Sympathomimetic Agents
mimic activation of the SNS by increasing adrenergic receptor activity, cause release of NE
Direct agonists- directly interact and activate adrenoceptors (NE, Epi, isoproterenol (b), albuterol (b2)
Direct a2 antagonist- Yohimbine, helps to put the brain to sleep
Indirect Agonists- dependent on ability to enhance the actions of endogenous catecholamines, don’t directly with the receptors
By enhancing release from nerve terminals (reserpine, amphetamines, tyramine)
By blocking re-uptake/removal of the transmitter (cocaine, methylphenidate)
By preventing enzymatic degradation of the neurotransmitter (MAOIs, COMT inhibitors)
Sympatholytic Agents
reduce activation of the SNS by reducing adrenergic receptor activity, by blocking the actions of NE and Epi on adrenergic receptors
Beta blockers (propranolol, metoprolol, atenolol) Lower BP
a1 antagonists (prazosin), a2 agonists (clonidine)
Effects of SNS Activation
Increase HR, arterial BP, and cardiac output
Increased blood flow to brain, heart, and skeletal muscles
Increased blood glucose
Pupil dilation
Increased rate of cellular metabolism
Increased rate and depth of respiration
Reduced saliva production
Reduced gut motility and urine flow
Sympathomimetic and Sympatholytic drugs are very important because they are used in so many conditions
Cardiogenic shock
Anaphylactic shock
Hypotension
Congestive heart failure
Bronchial asthma
Nasal decongestion
Narcolepsy
ADHD
Hypertension
Diuretics
Beta-blockers (atenolol, metoprolol, propanolol) to reduce strength of contractions
ACE inhibitors
Angiotensin II receptor blockers
Calcium channel blockers
Alpha blockers (praxosin- a1 blocker) relaxes smooth muscles of blood vessels
Alpha-2 receptor Agonists (clonidine) relaxes smooth muscles of blood vessels
Combined alpha and beta-blockers (carvediolol, labetalol, dilevalol)
Inadequate Heart Function
Hypotension
NE, phenylephrine- causes vasoconstriction which increases BP
Cardiogenic shock or acute heart failure
Dopamine, dobutamine- for inotropic effect (increase force and speed od cardiac output)
Cardiac arrest
Isoproterenol, epinephrine- increases strength of contractions and causes vasoconstriction
Asthma
Direct b2 agonists- to relax smooth muscles in airways, bronchodilation
Albuterol
b2 agonist
Levalbuterol
Metaproterenol
Terbutaline
Inhaled corticosteroids
Anaphylaxis
Epinephrine
b1- increase cardiac output
b2- relaxes constricted bronchioles
a1- constricts capillaries and increases BP
Glaucoma
Beta blockers- betaxolol- lowers pressure by reducing aqueous humor production
Now mostly replaced by prostaglandins
Nasal Congestion
Oxymetazoline- a1 and a2 agonist in arterioles of nasal mucosa- vasoconstriction
Phenylephrine- a1 agonist in arterioles of nasal mucosa- vasoconstriction
Pseudophedrine- acts on both a and b receptors to cause vasoconstriction
Cholinergic Receptors
Receptors are classified as nicotinic or muscarinic, based on whether they have high affinity for nicotine or muscarine
Nicotinic receptors are ionotropic- ion channel
Muscarinic receptors are metabotropic
There are multiple subtypes of each subclass of receptor
Nicotinic Receptors
They are ionotropic and form a sodium channel
Nicotinic receptors are ionotropic and pentomeric (made up of 5 subunits), consisting of alpha, beta, gamma, delta, epsilon subunits
There are multiple isoforms of alpha and beta subunits
There are 4 transmembrane domains
Primarily act as sodium channels, Can also increase permeability to Ca
Muscarinic Receptors
Metabotropic
2 subtypes
M1 (includes M1, M3, and M5 receptors) proteins that have been identified and cloned
M2 (includes M2 and M4 receptors)- proteins
Location and Function of M1 receptors
GI tract
glands- secretion
Location and Function of M2 receptors
Heart
SA node- decrease HR- negative chronotrophy
AV node- decreased conduction velocity- negative dromotropy
No effects on ventricles, purkinje system
Location and Function of M3 receptors
Eye
Sphincter- Contraction- miosis
Ciliary muscle- Contraction- accommodation for near vision
Lungs
Bronchioles- Contraction- bronchospasm
Glands- secretion
GI tract
Stomach- Increased motility- cramps
Intestine- Contraction- diarrhea, involuntary defecation
Bladder
Contraction, relaxation, voiding, urinary incontinence
Sphincters
Relaxation, except lower esophageal which contracts
Glands
Secretion- sweat, salivation, and lacrimation
Blood vessels
Dilation (via NO/endothelium- derived relaxing factor)- no innervation, no effects of indirect agonists
Parasympathomimetic agents
mimic activation of the PNS by increasing muscarinic cholinergic receptor activity
Direct agonists- directly interact with and actiavte muscarinic cholinergic receptors (ACh, methacholine, bethanechol, muscarine, pilocarpine
Indirect agonists- Enhance ACh effects by inhibiting cholinesterase thereby blocking degradation (neostigmine, physostigmine, donepezil, galantamine, rivastigmine)
Parasympatholytic Agents
reduce activation of the PNS by
Blocking the actions of ACh on muscarinic receptors (atropine, scopolamine, and other muscarinic receptor antagonists)
Effects of PNS Activation
Decreased HR, arterial BP, and cardiac output
Decreased blood glucose
Pupil constriction
Increased sweating and tearing
Increased saliva production
Increased gut motility and urine flow
Decreased rate of cellular metabolism
Bronchoconstriction
Cholinergic mimetic drugs are very important because they are used to treat so many conditions
GI and Urinary tract (urinary retention, atony or paralysis of the stomach or bowels after surgery) Treated with bethanechol or neostigmine
Dry mouth (to stimulate salivary secretions) Treated with pilocarpine or cevimeline
Dysfunction at the neuromuscular junction (Myasthenia gravis which is associated with reduced nAChR function) Treated with cholinesterase inhibitors like pyridostigmine
As antidote to overdose of tricyclic antidepressants
Memory disorders associated with AD, and PD (cholinesterase inhibitors like donepezil, galantamine, rivastigmine)
Parasympatholytic (anti-muscarinic) drugs treat a variety of disorders
Atropine
Prototypical non-selective antimuscarinic agent
Used to treat bradycardia, to reduce salivation and bronchial secretions before surgery, and as antidote for overdose of cholinergic drugs
Methantheline
Dries salivary secretions
Propantheline
Reduces GI motility
Diphenhydramine
In addition to blocking muscarinic cholinergic receptors, also blocks H1 histamine receptors
Dries nasal secretions
Antiemetic effects
Sedation
Atropine Poisoning
Atropine is a relatively safe drug in adults; however poisoning can occur with extreme doses
Symptoms include:
Dry mouth
Mydriasis
Tachycardia
Hot and flushed skin
Elevated body temperature
Agitation
Delirium for as log as 1 week
Think: Dry as a bone, blind as a bat, red as a beet, mad as a hatter