PSL Cumulative
1/290
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
291 Terms
Metabolic reactions
Anabolic reactions are those that create larger molecules from smaller ones.
Applied in a fed state where glucose is used for energy.
Catabolic reactions are those that break down larger molecules into smaller molecules.
Applied in a fasting state where glucose and fats are used for energy.
When fed → glucose goes through glycogenesis → built into glycogen for glucose storage in the liver and muscle.
When fasted, that glycogen goes through glycogenolysis → broken down to glucose → glycolysis, TCA, and oxidative phosphorylation → ATP
When fed, fatty acids and glycerol go through lipogenesis → built into triglycerides in fat tissue.
When fasted, those triglycerides go through lipolysis → broken down to fatty acids and glycerol → beta oxidation of free fatty acids → ATP
When fed, amino acids go through protein synthesis → protein in the muscles.
When fasted, protein in the muscle goes through protein degradation → amino acids.
Glycerol and amino acids can also be turned to glucose through gluconeogenesis.
Pancreas
Releases exocrine secretions for digestion.
Beta cells secrete pro insulin → cleaved into insulin and a c peptide
Alpha cells secrete glucagon
Delta cells secrete somatostatin.
Glucagon vs Insulin
Both hormones bind to a receptor to activate a secondary messenger to phosphorylate proteins and cause a response that switches between feeding and fasting.
Insulin binds to a receptor enzyme
Glucagon binds to a GPCR.
When fasted, your glucagon levels are high to promote the breakdown of stored glucose for energy and your insulin levels are low to prevent any blood glucose from being converted to storage.
After you eat, your glucagon levels go down while your blood glucose levels go up → rising blood glucose promotes insulin release so insulin spikes → insulin conc slowly goes down as it pushes blood glucose into cells for storage.
Insulin goal: Take blood glucose into cells for storage.
Glucagon goal: Prevent hypoglycemia
Insulin properties
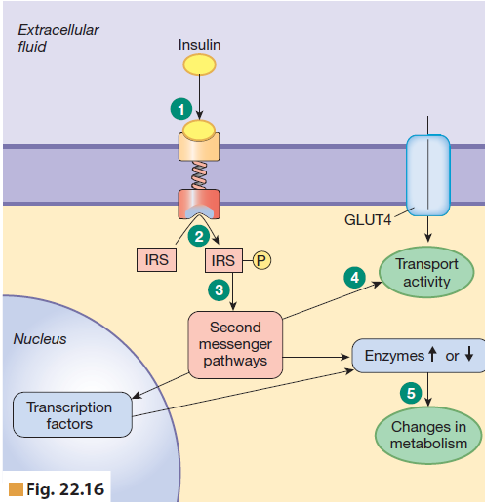
Made as a peptide hormone → binds to RTK → Insulin receptor substrates (IRS) are phosphorylated → secondary messenger pathways are activated →
Increased protein synthesis and enzymes → change metabolism
New GLUT4 transporters are made → Glucose can enter target cells
In the liver, glucose comes into the cell through GLUT2 transporters from an area of high conc int he ECF to lo conc in the cell → insulin activates hexokinase → phosphorylates glucose into G-6-P to trap it into the cell → keeps the concentration of pure glucose in the cell low → concentration gradient still active.
Insulin release process:
High blood glucose → binds to GLUT receptor in B cell → glycolysis and TCA activated → more ATP → potassium channels closed → less potassium leaves the cell → cell depolarizes cuz no more K → Ca channels open → Ca influx → exocytosis of insulin triggered → insulin released.
Activates:
glucose oxidation
glycogen synthesis
Lipogenesis
protein synthesis
Inhibits:
Glycogenolysis
Gluconeogenesis
Lipolysis
Beta oxidation
Also increase the transport of glucose into cells and the uptake of amino acids into muscle cells for protein synthesis
GLUT 4 transproter
When insulin levels are low, the GLUT4 receptor in muscle cells or fat tissues is dormant and inactive.
When there is high insulin and it binds to the receptor, the signal cascade activates the exocytosis of the dormant GLUT 4 receptor to the cell surface, allowing glucose to enter.
Incretin effect
Glucose that is consumed results in a lot more insulin release than that which is injected into the blood.
Called incretin effect.
An increase in insulin in response to intestinal glucose.
Gastrointestinal hormones (Gastritis inhibitory peptide (GIP) and glucagon-like peptide (GLP-1)) are responsible for this,
When there are nutrients or parasympathetic activity like digestion, GLP-1 gets activated and when there is glucose, fatty acids, or amino acids, GIP gets activated.
GIP increases insulin and decreases stomach acid while GLP increases insulin, decreases glucagon, increases beta cell growth to allow for more insulin release, and decreases stomach acid.
Regulation of insulin
Activator:
High plasma glucose
GLP-1 or GIP
Plasma amino acids
Parasympathetic nervous system
Inhibitor:
Sympathetic nervous system.
Glucagon properties
Works opposite to insulin.
Increases glycogenolysis, gluconeogenesis, and ketogenesis.
Glucagon binds to Gs receptor → Gs alpha activated → adenylyl cyclase activated → ATP turned to cAMP → PKA activated → phosphorylates phosphorylase B kinase → phosphorylates phosphorylase b to phosphorylase a → breaks down glycogen into G-1-P → broken down further to glucose.
When glucagon is present, the glucose concentration in the cell increases, disrupting the concentration gradient → now, glucose flows through GLUT2 receptors from an area of high concentration inside the cell to low concentration in the ECF.
Regulation of glucagon
Activators:
Low plasma glucose
high plasma amino acids
sympathetic nervous system’
Inhibitors:
GLP-1 cuz this hormone is present when there are nutrients in the small intestine → not fasted state, fed.
Diabetes
Type 1 diabetes
There is low to no insulin secretion
Can be treated by insulin injections or pumps
Type 2 diabetes
There is a defect in insulin secretion and cells are less responsive to it.
Treated by diet, exercise to cause GLUT 4 translocation, and pills.
Sulfonylureas can mimic the effects of ATP to close potassium ATP channels → depolarization → Ca influx → Insulin release to help with insulin secretion.
Both types result in high blood glucose.
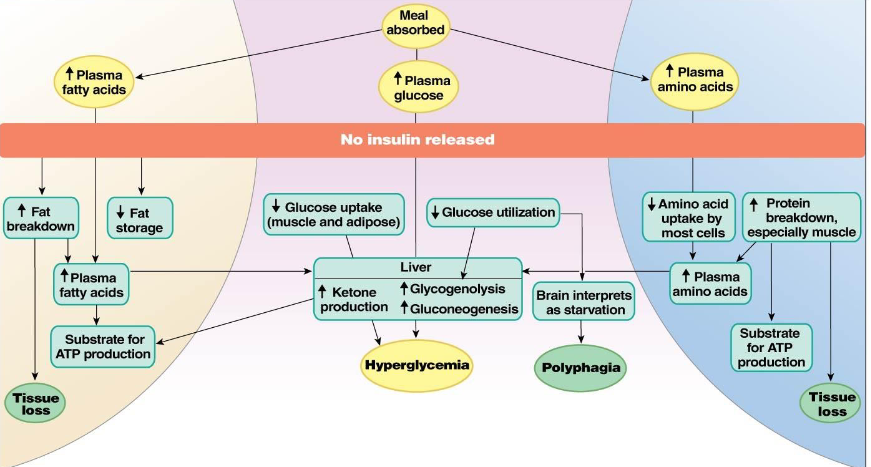
Uncontrolled type I diabetes
When type I diabetes is uncontrolled, it causes issues with fat, glucose, and protein metabolism.
Glucose metabolism:
Meal absorbed → increased plasma glucose → no insulin released →
glucose wont be taken up by the muscle and fat cells and glucose won’t be used as effectively → in the liver, high ketone production, glycogenolysis, and gluconeogenesis → hyperglycemia
glucose wont be used → brain thinks you’re starving → polyphagia (increased hunger)
Protein metabolism:
Meal absorbed → increased plasma amino acids → no insulin released →
decreased amino acid uptake by cells and more protein breakdown → plasma amino acids stays high → in the liver, high ketone production, glycogenolysis, and gluconeogenesis → hyperglycemia
High protein breakdown → tissue loss.
Fat metabolism:
Meal absorbed → plasma fatty acids increase → no insulin released →
More fat breakdown (lipolysis) → tissue loss OR →
More plasma fatty acids → in the liver, high ketone production, glycogenolysis, and gluconeogenesis → hyperglycemia
Less fat storage.
If you get hyperglycemia → your renal glucose threshold will be too high → glucosuria, where your pee glucose is too high → Osmotic diuresis and polyuria, where you pee too much →
high osmolarity → thirst and ADH secretion → polydipsia where you drink a lot because of water loss in your body.
dehydration → polydipsia
dehydration → low blood volume and pressure → circulatory failure or attempted compensation by your cardiovascular system and then circulatory failure → coma or death OR anaerobic metabolism → lactic acid production → acidosis → high ventilation and acidic pee or death/coma.
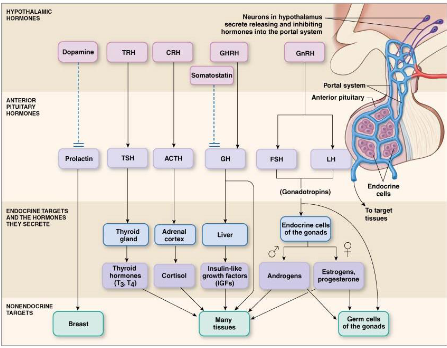
Hypothalamus pituitary route
Hormones are created by the hypothalamus and secreted by the pituitary gland.
Pituitary gland is separated into two sections
Posterior pituitary: Secretes neurohormones vasopressin and oxytocin
Neurohormone made in hypothalamus → packaged into neuron cell body → transported down the cell → stored in posterior pituitary → secreted into blood stream.
Anterior pituitary: Secretes endocrine hormones prolactin, thyrotropin, adrenocorticotropin, growth hormone, FSH, and LH.
Neurohormones made in neurons of hypothalamus → released into portal system capillaries → portal veins carry to anterior pituitary → act on endocrine cells → endocrine cell secretes peptide hormones into bloodstream →
Prolactin goes to boobs and is inhibited by dopamine if secreted by hypothalamus.
GHRH can stimulate GH → liver → stimualte insulin life growth factors (IGFs) → other tissues. Can be inhibited by somatostatin.
TRH can stimulate TSH → thyroid gland → thyroid hormones → other tissues
CRH stimulates ACTH → adrenal cortex → cortisol → other tissues
GnRH stimulates LH and FSH → endocrine cells of ovaries and testes → androgens and estrogen → other tissues or germ cells of gonads.
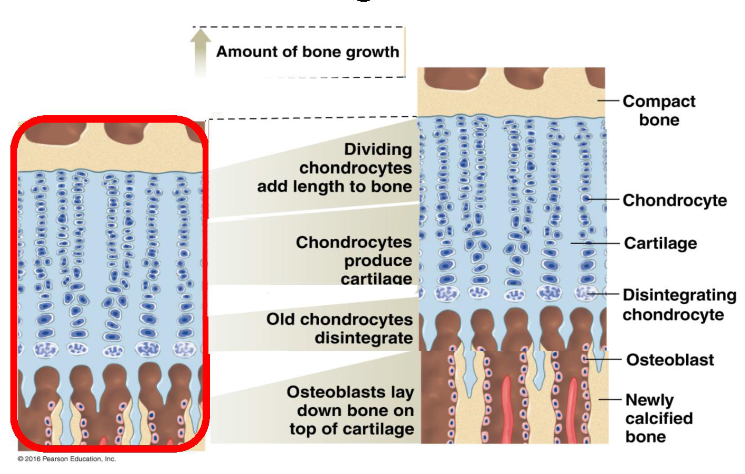
Bone growth
In utero, your bones start of soft, with your cartilage not fully ossified and active epiphyseal growth plates.
During adolescence, the bones are fully ossified and the growth plates start closing near the end of puberty.
In adulthood, your growth plates are fully formed and you start to lose bone mass.
Women lose bone faster than men because of menopause.
How:
Near the top, Chondrocytes, cells of the cartilage, add length to the bone by dividing → the chondrocytes eventually produce cartilage in the middle → causes the epiphyseal growth plates to widen → old chondrocytes close to the bottom start to disintegrate → osteoblasts replace the chondrocytes and lay bone down on top of the cartilage to cause ossification.
Growth hormone
A peptide hormone that is released by the anterior pituitary
Mechanism:
Stimulus like circadian rhythm, stress, or cortisol → hypothalamus secretes GHRH (growth hormone releasing hormone) → signals GH release in anterior pituitary → can either go and be used for bone and tissue growth and rising blood glucose or go to the liver and other tissues → stimulate insulin like growth factor release → cartilage growth, bone growth, increased blood glucose.
Inhibition:
When enough IGF has been made, it acts in a negative feedback loop and inhibits the anterior pituitary to stop releasing GH and inhibits the hypothalamus to stop releasing GHRH.
Somatostatin can also be released by the hypothalamus to inhibit GH release.
IGF-1 is how GH actually causes growing.
With more IGF, there is more chondrocyte recruitment which means widened growth plate, more chondrocyte proliferation which means lengthened bone, and more chondrocyte matrix which means more cartilage.
GH has other catabolic actions
Can stimulate adipose cells to breakdown their stored fats to fuel growth.
Can increase a.a uptake from the blood and increase cell proliferation
Can stimulate liver to break down glycogen into glucose for energy.
Gigantism
Too much GH in childhood
Grow vertically since its before your growth plates fuse
Acromegaly
Too much GH in adulthood
Grow horizontally since its after your growth plates fuse
Thyroid hormone
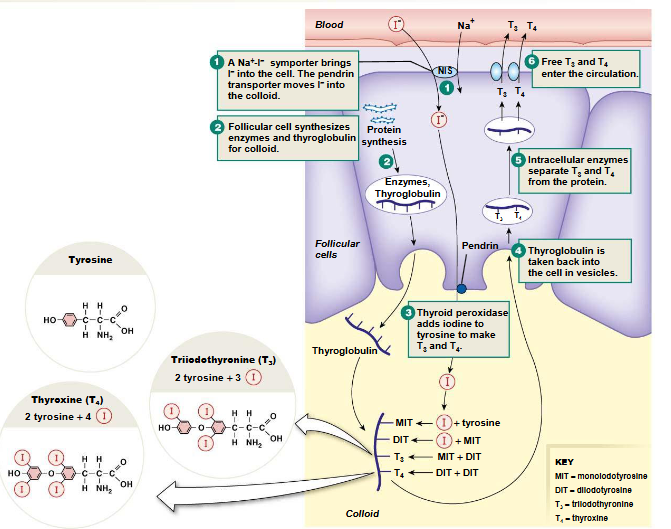
thyroid hormones are made in the thyroid gland from iodine and tyrosine and are stored in the colloid.
Iodine ion moves into the cell from a NIS (Na I Symporter) → The thyroid hormone precursor thyroglobulin is synthesized for the colloid → iodine and thyroglobulin in the colloid → thyroid peroxidase adds iodine to tyrosine → if one iodine is added, it is monoiodotyrosine (MIT) . If another iodine is added to MIT, it is called dioiodotyrosine (DIT). If MIT and DIT are added together, it is T3 or triiodothryonine. If DIT and DIT are added together, there is T4 or thyroxine → Once T3 and T4 are made, the thyroglobulin with them is taken back into the cell in a vesicle → Once in the cell, enzymes separate T3 and T4 from thyroglobulin → T3 and T4 enter the circulation → Since T3 is a lot more active than T4, T4 is converted to T3 in target tissues.
TSH, thyroid stimulating hormone, stimulates the creation of enzymes required for T3 and T4 synthesis.
Works through adenylyl cyclase
Thyroid hormones have diff functions
Metabolic: change metabolic rate, oxygen consumption, heat production, protein degradation, lipolysis.
Nervous system: Can enhance speech, reflexes, and thinking.
Growth
Cardiovascular: Enhances heart rate, blood flow, increases beta adrenergic receptors.
Muscular
Hyperthyroidism
Too much thyroid hormone.
Causes tumors and thyroid stimulating immunoglobulins.
Symptoms are goiter, nervous, insomnia, anxious, high heart rate, weight loss.
Treated by taking away thyroid gland or blocking T4 T3 synthesis with drugs or blocking conversion of T4 to T3.
Grave’s Disease
Too many antibodies against TSH receptors.
Caused by hyperthyroidism
Hypothyroidism
Not enough thyroid hormone
Caused by underactive thyroid gland or not enough iodine in diet.
Symptoms are goiter, low heart rate, slow speech, fatigue, less growth, weight gain.
Treated by adding T4
Hormonal control of reproduction
LH (Luteinizing hormone) and FSH (Follicle-stimulating hormone) are the main ones involved in reproduction.
A stimulus in the CNS causes secretion of GnRH (gonadotropin releasing hormone) in the hypothalamus → stimulates release of LH and FSH in the anterior pituitary →
LH in both genders goes to the endocrine cells → steroid and peptide hormones produced → gamete production.
LH in females is responsible for signaling theca cells to secrete androgens
LH in males is responsible for signalling Leydig cells to secrete testosterone
FSH goes to promote gamete production
FSH in females is responsible for the differentiation of follicles and for signalling granulosa cells to convert androgens to estrogen.
FSH in males is responsible for signalling Sertoli cells to secrete ABP and to develop the testes.
Steroid and peptide hormones can act in a negative or positive feedback loop on the anterior pituitary and hypothalamus.
GnRH can be inhibited in a negative feedback loop by hormones in the anterior pituitary.
GnRH secretion
GnRH is secreted from the hypothalamus in electrical pulses.
When there is a low frequency pulse, FSH will be signaled for.
When there is a high frequency pulse, LH will be signaled for.
These frequencies change at different life stages, allowing for control of hormonal response.
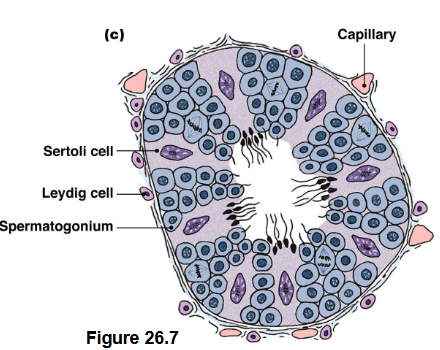
Sperm production
Sperm is produced in the testis of males.
Sperm is surrounded by its external environment.
The scrotum and capillaries maintain the temperatures of the sperm, allowing it to be at 2-3 degrees lower than body temperature.
Sertoli cells or sustentacular cells support sperm development.
Since developing sperm in the seminiferous tubules can't access blood nutrients directly, Sertoli cells give the sperm their nutrients and take away their waste.
Also provide tight junctions to create the blood-testis barrier → prevents immune cells from detecting developing sperm cells and killing them.
Leydig cells or interstitial cells secrete testosterone.
FSH and LH have roles in male reproduction.
FSH → Sertoli cell receptor → signaling cascade → production of cell products → Androgen binding proteins (ABP) → help concentrate androgens in the testis. The cell products can also → inhibin instead →inhibits FSH release
LH → Stimulates Leydig cells → secrete testosterone → has secondary effects in the body + goes to sertoli cells. Testosterone can also inhibit LH and GnRH
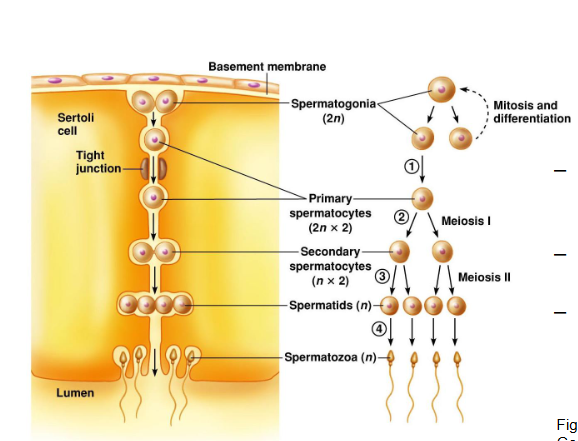
Spermatogenesis
Spermatogonia, sperm precursors, are formed during fetal development and go through mitosis → One of them continues to go on to meiosis while the other continues to do mitosis, creating a pool of sperm precursors for backup → The one that will be going through meiosis becomes a primary spermatocyte and goes through tight junctions to go further down the cell → goes through meiosis I → 2 secondary spermatocyte → goes through meiosis II → 4 spermatids → as they mature, they will lose their cytoplasm and gain a tail, turning them into spermatozoa.
Spermatozoa anatomy
Has an acrosome in the tip that is derived from the Golgi apparatus.
Contains hyaluronidase and acrosin which break down the zona pellucida which is a glycoprotein that covers the oocyte to allow for fertilization.
Acrosome → nucleus → centrioles → mitochondrial spiral → microtubules that make the tail.
What is semen
Made 1% of permatozoa and mostly secretions foa ccessory glands.
Has water
Has lubricants for movement (Mucous)
Has buffers that neutralize the acid of the female reproductive tract
Made by the prostate gland and bulbourethral gland
Has nutrients
Fructose
citric acid
vit c
carnitine
Has enzymes and zinc.
Has prostaglandins to allow for muscle contractions.
Hypogonadism
Less functioning testes
Lower production of androgens, inhibin, and sperm.
Primary is in the gonads
More GnRH production → More LH and FSH production → damage to testis → less testosterone
Secondary is in the hypothalamus
Damage to hypo → Less GnRH production → Less LH and FSH or maybe equal FSH → less testosterone.
Testosterone functions
Sex specific
Promotes spermatogenesis
Maintains secretions from prostate
Maintains repro tract
Reproductive
more sex drive
Negative feedback on GnRH and LH
Secondary
Balding
5 alpha reductase can be inhibited by finasteride to prevent balding
Muscle growth
Nonreproductive
Protein synthesis
more agression
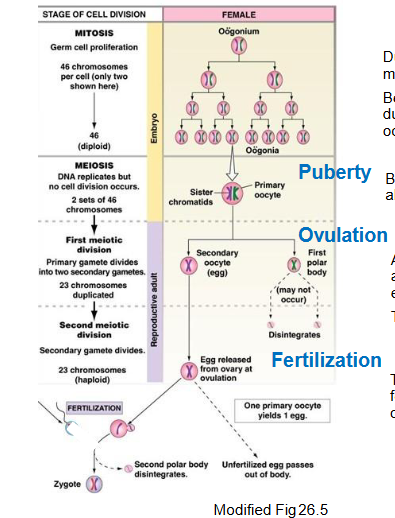
Oogenesis
The production of oocytes.
During fetal life, the germ cells go through mitosis multiple times to form oogonia → before the girl is born, meiosis I will occur to duplicate the DNA → birth → 1-2 million primary oocytes with sister chromatids → until puberty, these oocytes naturally die, leaving 300,000 of them at puberty → After puberty, one one primary oocyte goes to finish meiosis I and go through meiosis II, making it the secondary oocyte. This happens every 28 days. → Secondary oocyte is released during ovulation.
If the secondary oocyte gets fertilized, it will go through meiosis II. If not fertilized, it will die.
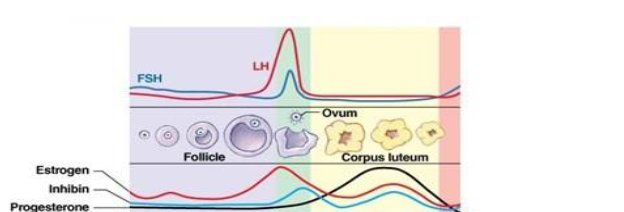
Menstrual cycle
Made of the ovarian cycle in the ovaries and uterine cycle in the uterus.
Ovarian cycle:
Made of the follicular phase (Days 1-14) and the Luteal phase (Days 14-28).
Follicular Phase:
During this phase, only one dominant follicle is selected from the ovary and the rest die through atresia.
Small number of primordial follicles around the oocyte → Primary follicle with granulosa cells and theca cells → Secondary follicle → tertiary follicle with an antrum which has fluids with hormones and enzymes → dominant or Graffian follicle with secondary oocyte and even more fluid in the antrum → Ruptured follicle → Ovulation.
Theca cells produce androgens and Granulosa cells turn them into estrogens.
Ovulation:
The mature oocyte is released into the abdomen → Fimbriae has a wave-like motion and uses its fingers to take the oocyte into the fallopian tube.
There is a surge in LH to cause follicular cells to release collagenase → digests connective tissue. Also causes release of progesterone → smooth muscle contractions.
Luteal Phase:
The theca and granulosa cells of the follicular cells left behind when the oocyte leaves become luteal cells → whole cell becomes fatty corpus luteum which releases progesterone and estrogen → if there is no fertilization, corpus luteum degenerates and forms corpus albicans. If there is fertilization, the corpus luteum will continue to secrete its hormones.
Uterine Cycle
Uterus is super muscular to allow for contractions during child birth.
The endometrium is important for the growth of blood vessels.
Menses:
Blood vessels that supply the endometrium get constricted and lose their lining because of declining progesterone and estrogen.
The blood is this shedded layer.
Day 1-5
Proliferative phase:
Rise in estrogen from the ovaries → signals endometrium to grow again → endometrium lining thickens → cells proliferate
Days 5-14
Secretory phase:
Glands in the endometrium secrete more viscious fluid and lipids and glycogen in the cytoplasm in response to progesterone and estrogen.
This is just in case the oocyte becomes fertilized.
Hormonal control of mensturation
During early to mid follicular phase:
Low amounts of FSH and LH but rising amounts of estrogen.
GnRH → LH is secreted → theca cells produce androgens.
GnRH → FSH is secreted → granulosa cells to convert androgens to estrogen.
FSH → Granulosa cells to make AMH which prevents recruiting more follicles.
Estrogen made → inhibits GnRH in negative loop→ Less FSH and LH release → that is why they are low levels.
Estrogen made → activates more granulosa proliferation in positive loop → even more estrogen.
Late follicular phase and ovulation:
Follicular cells secreting LH, FSH, estrogen, inhibin, and progesterone.
Inhibin → Inhibits FSH in a negative loop → Lower FSH levels.
Secreted progesterone makes pituitary more sensitive to GnRH while estrogen increases GnRH release → LH Surge but no FSH surge because of inhibin.
LH surge → complete Meiosis I and do ovulation.
Early to mid luteal phase:
Corpus luteum secretes progesterone, inhibin, and estrogen cuz of LH and FSH.
All hormones negative loop to inhibit GnRH → decreasing LH and FSH levels.
Progesterone and estrogen decrease GnRH pulses.
Late luteal phase:
Low everything.
FSH causes new follicles to develop.
If no fertilization, corpus luteum dies and estrogen and progesterone levels drop.
Estrogen synthesis and function
Cholesterol → desmolase turns it to progesterone → 21 hydroxylase turns it to androstenedione → aromatase turns it to estrone → estradiol.
Sex specific
Follicular development and ovulation
Growth of endometrium
maintain reproductive tract
Reproductive
Inhibit GnRH LH and FSH
Sex drive
Secondary
Grow breast tissue
pubic and axillary hair
Non reproductive
fat deposition around hips and thighs
Menopause
End of reproductive cycle
Ovaries can respond to FSH and LH anymore
Estradiol and progesterone levels drop
LH and FSH rise.
Capacitation
Sperm needs to be capacitated before it can cause fertilization.
Allows it to swim fast as well.
Happens in the female reproductive tract so in artificial pregnation, the sperm needs to be artificially capacitated.
Albumin, enzymes, and lipoproteins bind to the sperm to remove the glycoprotein coat, cause intracellular changes, and cause a whip-like motion → allows sperm to pass through cervical mucous.
The contractions during sex also allow this to happen.
Fertilization
100 sperm reach the oocyte for fertilization and are guided by chemotaxis which is progesterone of cumulus cells.
The sperm tunnels through the barriers using the acrosomal enzymes on its head → docks on the oocyte membrane using sperm-binding proteins → depolarization of oocyte triggered → cortical granules (the oocyt’’s intracellular vesicles) fuse with outer membrane → oocyte is fertilized and has a coated outside to prevent penetration by other sperm.
After fertilization
Zygote travels down the fallopian tube and undergoes cell division → becomes a blastocyst → goes into the uterus and implants.
Blastocyst contains trophoblast on its exterior which secretes hCG, the fertilization hormone.
Prevents the next menstrual cycle by taking over the pituitary and maintaining the corpus luteum so it doesnt die.
Corpus luteum secretes progesterone to keep the endometrium intact and estrogen and inhibin to prevent negative feedback loop.
Placenta
The trophoblast becomes the placenta.
Important for digestion, respiration, and the renal system of the uterus.
Exchanges nutrients for waste, oxygen for carbon dioxide, and proteins.
Placental circulation
The fetus and mom vasculation are not physically linked, they’re just intertwined.
Cholesterol in mothers blood → placenta can either become progesterone and go back to mother’s blood or continue → fetal blood → fetal adrenal cortex → DHEA in fetal adrenal cortex → fetal blood → placenta → estrogen in placenta → estrogen in mother’s blood.
Placenta hormones
hCG
Maintains corpus luteum and stimulates fetal testis
Progesterone
Suppresses uterine contractions, cervical plug, and mammary gland development.
Estrogen
Uterine development, breast duct development
Human placental lactogen
related to growth hormone and prolactin
high in the mom low in the baby
less maternal uptake of glucose
more maternal lipolysis
maternal adaptations to pregnancy
renal
more vasopressin to have more blood volume
More RAS sodium and fluid retention
Cardiovascular
more output
Immune system
partially surpressed
calcium homeostasis
calcium transferred to fetus
more calcitonin so bone doesn’t move.
trigger of labour
Relaxin released from ovary → placenta loosens ligaments in pelvic bone → cervix softens → fetus drops to lower uterus → cervical stretch → oxytocin from posterior pituitary → uterine contractions or prostaglandins released first → more cervical stretch → repeat until baby is out.
Triggered by
high estrogen and oxytocin
fetus cortisol
CRH
Prostaglandins
breast milk
estrogen and progesterone develop your mammary glands but inhibit milk production → levels drop after birth so you can produce milk
Prolactin stimulates milk production by epithelial cells.
Oxytocin stimulates contraction of myoepithelial cells, leading to milk ejection
regulation:
stimulus of crying baby or sucking → hypothalamus release of dopamine inhibited → anterior pituitary secretes prolactin cuz no longer inhibited by dopamine → milk secretion. posterior pituitary releases oxytocin → muscle contractions → milk ejected.
Fetus development
At 6 weeks, the bipotential primordium will start to develops into different things depending on the chromosome.
If there is no functional Y chromosome, it will start to go down the female development pathway:
Bipotential primordium → ovary → Mullerian duct → fallopian tube + uterus + upper vagina.
At 10 weeks, the gonadal cortex will become the ovary IF no functional SRY protein. AND the Wolffian duct will degenerate if there is no testosterone
At birth, the Mullerian duct will become the fallopian tube, uterus and upper vagina IF no anti-Mullerian hormone.
If there is a functional Y chromosome, it will start to go down the male development pathway:
Bipotential primordium → testis → wolffian duct → epididymis + vas deferens + seminal vesicle.
The SRY gene is key for male development → It encodes TDF, the testes determining factor.
SRY → SOX9 activated → Transcription of Sertoli cells for AMH secretion and Testes + Transcription of Leydig cells for testosterone. AMH also represses female structures.
So at 10 weeks, if SRY → medulla of the bipotential primordium directed to develop into testis. AND AMH causes Mullerian ducts to disappear.
At birth, testosterone from the testis converts the Wolffian duct to seminal vesicles, vas deferens, and epididymis. DHT allows for prostate development.
Role of SOX9
Early on in fetus development when the gonad is undifferentiated, there are low levels of SOX9 → If chromosomes become XX with no SRY → No SOX9 → Ovaries develop → B-catenin develops → represses SOX9.
If chromosomes become XY with SRY → high levels of SOX 9 → Testis develop → Even higher levels of SOX9 → B-catenin is repressed and male structure loops develop.
Females don’t want SOX9 because it initiates the differentiation of Sertoli cells.
SOX9 activates transcription of genes → This promotes proliferation and differentiation of Sertoli cell precursors
→ Sertoli cells then organize around clusters of germ cells.
Hormones in male development
SRY gene in the Y chromosome → produces the testis determining SRY protein → initiates the production of other proteins → cause gonad medulla to differentiate into testis → Testis have:
Leydig cells → secrete testosterone → controls the development of the Wolffian duct into other structures and uses 5 alpha reductase to turn into DHT → causes development of male external genitalia.
Sertoli cells → secrete AMH → causes regression of Mullerian duct.
DHT vs testosterone
Testosterone is primarily responsible for the development of internal male reproductive structures (from the Wolffian duct)
Dihydrotestosterone (DHT) is primarily responsible for the development of external male genitalia and the prostate.
Hormones in female development
Beta catenin suppresses he expression of SOX9, allowing development of female organs and thus estrogen and estradiol.
CNS vs PNS
CNS is made of the brain and spinal cord.
Has ventricles filled with CSF that cushion the brain and prevent mechanical stress.
Lateral ventricle → 3rd ventricle → fourth ventricle → Central canal
Has gray matter with nerve cell bodies arranged in layers or clusters called nuclei, unmyelinated axons, and dendrites.
Has white matter with myelinated axons in bundles called tracts
Most neurons are in the CNS
Neurons and parts of neurons outside of the brain and spinal cord are only in the PNS.
Parts because sometimes neuron can be in the CNS but send messages to parts in the PNS.
PNS is made of two parts
Somatic nervous system which controls voluntary actions through skeletal muscles (Ex. moving your arm to pick up a cup)
Autonomic nervous system which controls visceral functions (Ex. heart rate and breathing).
Autonomic nervous system is separated into the enteric nervous system which controls digestion and gut movement. Can do it alone or based on spinal cord.
Has clusters of neurons called ganglia and bundles of axons called nerves
Both PNS and CNS have glial cells that protect the neurons.
CNS vs other things
Compared to other organs, the CNS uses lots of energy.
very light but uses 15% of the blood pumped by the heart.
The CSF makes it lighter
It also uses half of the body’s glucose.
It still saves energy by limiting communication between neurons.
Neurons communicate with each other using action potentials down axons but those take lots and lots of energy → the energy supplied to the CNS can’t support a high rate of firing of action potentials → only 4% of neurons can fire action potentials.
Therefore, communication is very expensive so the CNS has to use that energy sparingly.
Spinal cord
31 segments → each has a pair of spinal nerves on the right and left side → each nerve has a dorsal root → each dorsal root carries afferent signals which are the incoming sensory ones → the dorsal root ganglion has the cell bodies of the neurons that carry those signals.
each spinal nerve also has a ventral root → ventral root carries the efferent signals which are the outgoing ones that the CNS is sending to the body like the motor signals
Dorsal root is in the back, ventral root is in the front.
Set up in a butterfly shape.
Gray matter in the middle
Dorsal horn on the upper side on each side
Ventral horn on the lower side on each side.
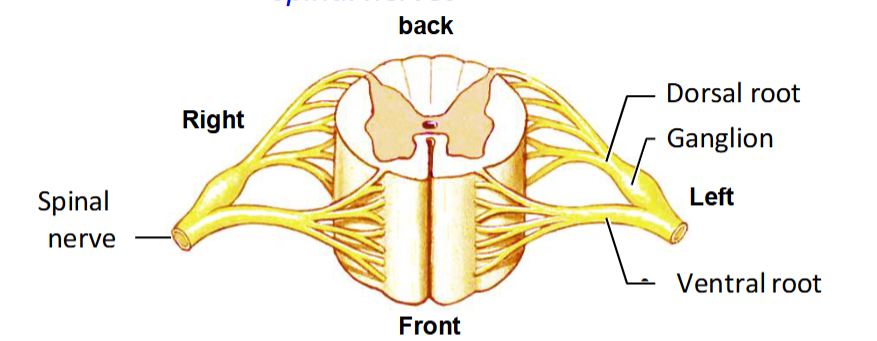
Gray matter
Made of sensory and motor nuclei
Somatic sensory nuclei → visceral sensory nuclei → autonomic efferent nuclei → somatic motor nuclei
Sensory nuclei are in the dorsal horn cuz the sensory signals arrive on the dorsal root.
The somatic ones get signals from the skin
the visceral ones get signals from the viscera which are the internal organs.
Efferent nuclei are on the ventral horn cuz that is where the signals are sent from.
Autonomic ones send signals to the glands and smooth muscles
The motor ones send commands to skeletal muscles.
White matter
Has axon tracts
Ascending tract is on the upper side and carries sensory signals to the brain
Dorsal/on the top because sensory signals received in the dorsal horn.
Descending tract is mainly on the bottom side and carries signals from the brain
ventral (bottom) because thats where signals leave the CNS.
Propriospinal tract stays in the spinal cord.
Spinal reflex
In a spinal reflex, the spinal cord responds to stimuli without consulting the brain.
Ex. In a knee jerk, the rubber hammer hits the kneecap → sensory fibers carry news to dorsal horn + excite neurons in the ventral horn → sends signals to the leg muscle to contract.
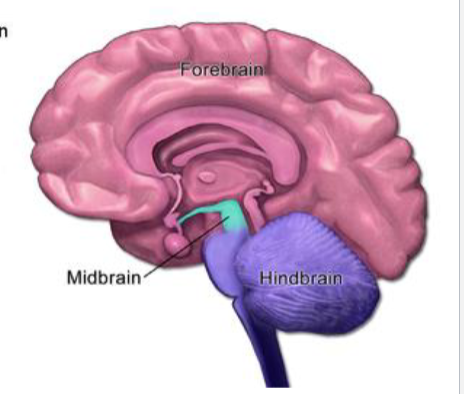
Brain
Made of the hind brain, midbrain, and forebrain.
Hindbrain:
Reticular formation
Medulla = Continuation of the spinal cord, relays info like blood pressure, reflexes
Pons = responsible for autonomic functions like breathing
Cerebellum = the center for movement
Midbrain:
Responsible for the visual and auditory functions.
Brainstem:
Made of the midbrain, pons, and medulla.
Center for autonomic functions and reflexes.
Ex. breathing, swallowing, vomiting, blood pressure.
Has cranial nerves 3 to 10 and also 12.
Forebrain:
Diencephalon = made of the thalamus, hypothalamus, pituitary, and pineal.
Thalamus processes information going to and from the cerebral cortex.
Hypothalamus regulates behavior and endocrine and autonomic homeostasis.
Pituitary and pineal glands secrete hormones.
Cerebrum = 2 hemispheres connected by the corpus callosum.
there is cortex on the outside made of gray matter
Limbic system
Basal ganglia.
Communication between the two sides happens with corpus callosum which has myelinated axons.
Hemispheres of brain
Part of the forebrain.
Left hemisphere responsible for speech, writing, language, and math.
Right hemisphere responsible for analysis of touch and spatial analysis.
Each hemisphere has 4 lobes
Frontal
Parietal
Temporal
Occipital.
Each hemisphere also has cingulate gyrus
Part of the limbic system
Regulates emotional behavior and balances emotion with logic
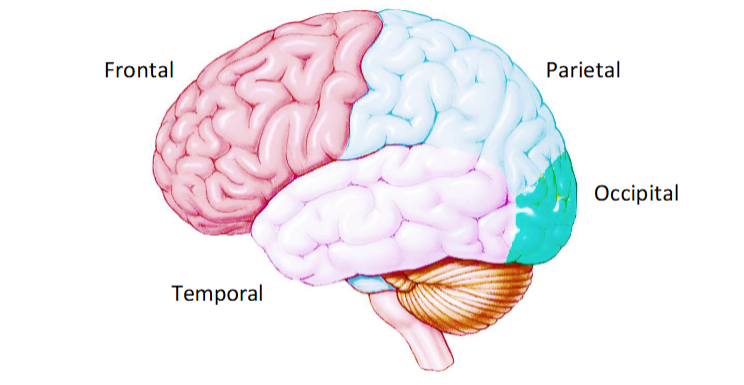
Limbic system
Cingulate gyrus (emotion), amygdala (fear), and hippocampus (memory)
Responsible for motivation, emotion, and memory.
Remove this system and no more fear.
Sensory receptors
The sensory system has receptors that convert the sensory stimulus into electrical signals.
Conversion is called transduction
Stimulus → receptor → change in membrane potential → called receptor potential → can release neurotransmitter to affect neuron. If receptor is a neuron, action potentials can be fired.
In some systems, the receptors are neurons and in others, they are non-neuronal epithelial cells.
Vision = neuron
Hearing = non neuron
Each receptor type has an adequate stimulus
A stimulus with a form of energy that its most responsive to.
Will respond to other forms of energy if strong enough.
Also has a receptor threshold
Weakest stimulus that it will respond to
Receptor classes
Chemo receptors
pH, O2, organic molecules
Mechanoreceptors
vibration, acceleration, sound
Photoreceptor
Light
Thermoreceptor
Temperature
Nociceptor
Tissue damage/pain
Perceptual threshold
Diff from receptor threshold.
Weakest stimulus that causes conscious perception in the organism.
Ex. number of odorants needed for you to smell something.
Hierarchy of sensory processing
Brain distinguishes between
Stimulus modality
Stimulus intensity
Stimulus duration
Stimulus location
Stimulus modality
The type of stimulus
Sound, light, touch.
Know what the modality is based on what neurons/axons are carrying the signal.
If neuron in visual pathway is carrying signal, modality is light.
Stimulus intensity
The strength of a stimulus can be understood in 2 ways
Population coding of intensity
The stronger a stimulus is, the more neurons get activated.
Louder sound = more neurons.
So strength = number of neurons.
Frequency coding
The stronger the stimulus, the faster neurons fire.
Both can happen together.
Stronger stimulus = more neurons firing faster.
Stimulus duration
The response to a stimulus can depend on how the stimulus changes over time.
Some cells signal changes in the stimulus but when it is steady, they are not active.
The cell type determines this dynamic.
Phasic: Only active and responsive when there is a change in stimulus intensity.
Tonic: Active as long as the stimulus is present.
Phasic-Tonic: Responsive to change but also a constant stimulus.
Retinal cells are phasic, so they only recognize changes in the visual world so basically when something moves.
If something is not moving at all, your eyes won’t see it.
Stimulus location
Each sensory receptor has an area on you that it responds to.
Called its receptive field.
Flow of information
The first neuron that responds is the primary sensory neuron → synapses onto the secondary sensory neuron → synapses on tertiary….
Can combine data to really understand your surroundings.
This data can be combined into one cell through convergence.
Increases neuron’s sensitivity (weaker stimulus threshold) but decreases spatial resolution (hard to tell where its from)
Spatial changes
Difference between neighboring areas.
Comparing one skin patch to the skin patch next to it
The difference between them is called contrast
How much a stimulus stands out compared to what is beside it
(Bright light in a dark area stands out)
Areas with very high differences or strong contrast are called edges.
Lateral inhibition
When one cell inhibits is neighbors or inhibits cells that neighbors excite
Sensory processing
Our brain has to infer the data it receives because sense data is incomplete and ambiguous.
This allows the brain to be fooled. .
The eye anatomy
The eye has a lens that is a transparent disk that focuses light.
Suspended by zonules which are ligaments.
In front of the lens is the anterior chamber which is filled with a plasma-like fluid called the aqueous humor.
Behind the lens is the vitreous chamber which is filled with a clear jelly called vitreous body/humor.
Keeps the eyeball’s shape.
The cornea bulges out of the front of the eye and is continuous with the outer wall of the eye called the sclera.
Together, the cornea and lens focus light into the retina which is the inner lining of the eye with our photoreceptors.
On top of the lens is a lining called the iris. An opening in the iris is called the pupil and this is where light from the cornea and lens pass through.
Cornea → anterior chamber → iris → pupil → lens → vitreous humor.
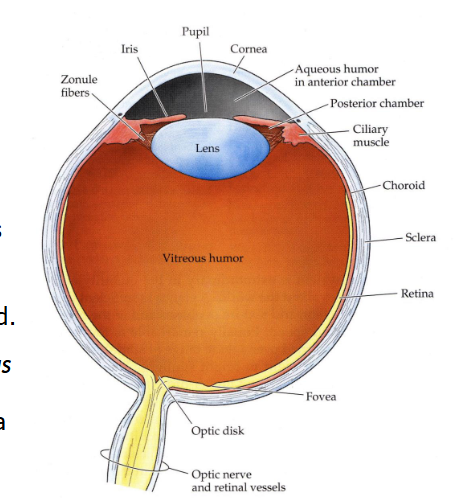
Humor pathway
The cornea and lens are avascular, meaning they don’t have any blood vessels → no access to nutrients in the blood → rely on the humor pathway to bring them the nutrients, remove waste, and maintain their intraocular pressure.
Disrupting leads to glaucoma
It is produced by ciliary processes.
Posterior chamber→ pupil → anterior chamber → trabecular meshwork → canal of Schlemm
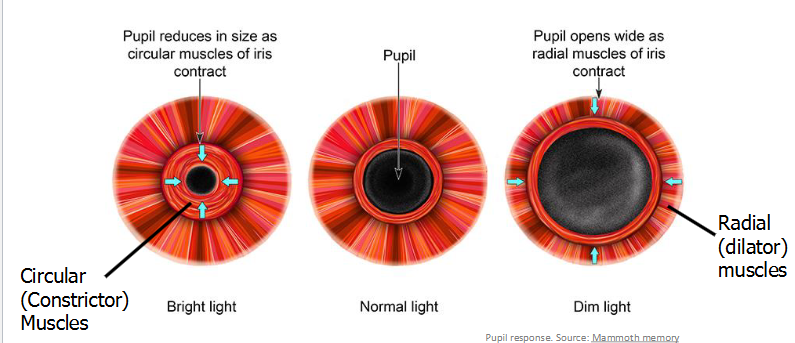
Pupil
An opening in the iris on top of the lens that light passes through.
Can change size in response to light.
In bright light, parasympathetic signals from the brain tell the circular constrictor muscles in the iris to constrict → shrinks the pupil → less light reaches the lens
In darkness, the sympathetic signals tell the radial dilator muscles in the iris to dilate → widens the pupil → more light reaches the lens
Changes in size can then focus light
A small pupil lets light only come in from one angle → each point in the retina to receive light from only one direction → more sharpened and focused vision
Changes in size can also control depth of field
A tightly constricted pupil allows for a full depth of field (everything is equally focused)
A dilated pupil causes a shallow depth of field (only objects at a certain distance are in focus).
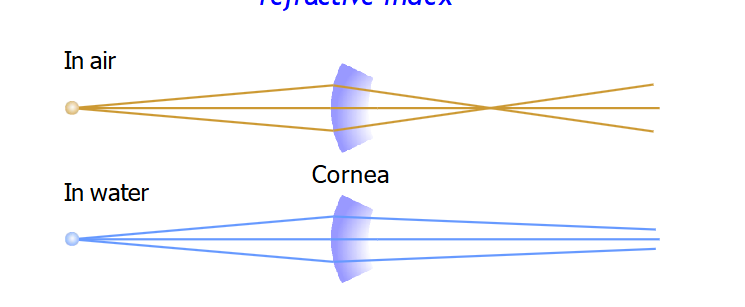
Refraction
With the pupil focusing light, the retinal image becomes dim because the hole of the pupil doesn’t allow much light to come in.
But we also can’t enlarge the hole cuz then it would become too blurry.
Overcome this through refraction.
The bending of light as it moves from one material to another
Light goes from the air to our cornea → The cornea is made of clear collagen and has a different refractive index than air → difference in material causes the light to bend → sharper vision
The cornea does 2/3 of the refraction and the lens does 1/3
Lens
The lens is made of clear cells with no nuclei
Cells are packed into structures called crystallins with no proteins.
They are arranged in a zipper manner in layers for flexibility.
Since it has no blood supply, it absorbs its nutrients from the aqueous humor.
The lens is convex
Fatter in the middle and thinner at the edges.
Makes light rays converge to a focal point.
How much light bends depends on the angle it hits the lens
Its refraction depends on the angle of incidence.
The angle depends on the shape of the lens and direction of the light.
Right angle → no bend
Obtuse angle → downward bend
Acute angle → upward bend
Can change the shape of the lens to alter the angle and thus bend the light more or less.
Rounder lens = more bending = closer focal point,
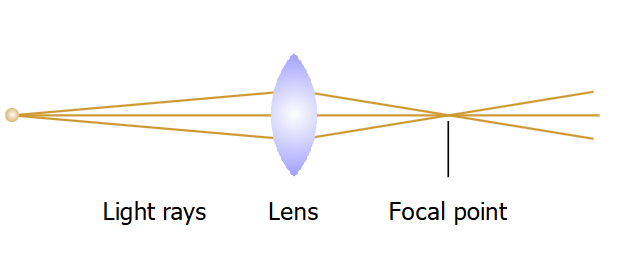
Accommodation
Rounding the lens for near vision.
If you want clear vision, the focal point needs to fall on the retina.
When the object is too close, the focal point falls behind the retina → Can bring the focal point back into focus by rounding the lens.
Parasympathetic nerve signals tell the ciliary muscle to contract → less tension in the zonulas → lens rounder → light rays bend more → focal point comes forward.
For far vision, the sympathetic signals can relax these ciliary muscles to make the lens flatter instead of rounder.
With age, the lens stiffens and accommodation becomes harder
Causes issue called presbyopia.
Hyperopia
Far sightedness
Focal point falls behind the retina → light is not being bent enough
Adding a convex lens solves this issue because it bends the light rays the way the lens couldn’t → light hits the retina
Myopia
Near sightedness
The focal point falls in front of the retina → light is being bent too much
Adding a concave lens causes the light rays to be more spread out → light hits retina
Photoreceptors
In the retina
Light sensitive neurons that convert light energy into electrical signals.
Conversion is called phototransduction
2 main types
Cones
6 million
Detect color and work better in bright light.
Rods
120 million
Used for night vision and very light sensitive.
The outer segments contain visual pigments that respond to light
Fold into disk layers
The inner segment has the nucleus and organelles needed for protein synthesis.
Basal layer contains a synapse that releases glutamate.
Photoreceptors respond to stimuli with graded potentials, not action potentials.
Light hits pigment molecules → shape change → chemical cascade → cell hyperpolarization → less glutamate release
There are millions of pigment molecules but each type of photoreceptor has one type of pigment; rhodopsin in rods and 3 other pigments in the 3 types of cones.
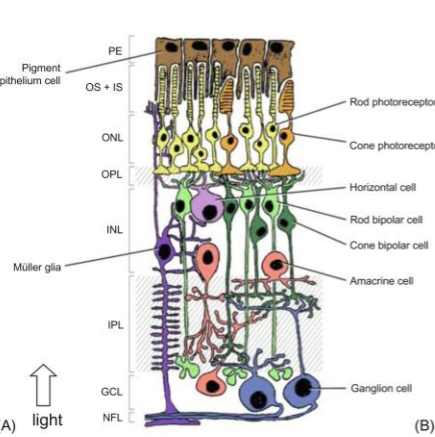
Passage of light
Light enters the eye → hits the retina → has to pass through multiple layers before it can get to the photoreceptors → once it its the photoreceptors, travels all the way back forward to hit the optic nerve
Starts with NFL (Nerve fiber layer)
Contains the axons of the ganglion cells
Eventually form the optic nerve
Next is the GCL (Ganglion cell layer)
Cell bodies of the ganglion cells.
has the output neurons of the retina that sends the final visual signal to the brain.
IPL (Inner plexiform layer)
Where synapses between bipolar cells, amacrine cells, and ganglion cells happen.
Motion and contrast
INL (inner nuclear layer)
Middle management layer
Contains the cell bodies of bipolar (carry signals from photoreceptors to ganglion cells), horizontal (refine signals), amacrine (motion and contrast), and muller glial cells (Support).
OPL (Outer plexiform layer)
Synapses happen between photoreceptors and horizontal and bipolar cells.
ONL (Outer nuclear layer)
Contain the cell bodies of cones and rods
OS (Outer segments)
Where phototransduction happens
Has the stacks of membrane discs with visual pigments
RPE (Retinal pigment epithelium)
Supports, nourishes, and regenerates the photoreceptors.
Light needs to pass through all of these layers to get to the photoreceptors in the back.
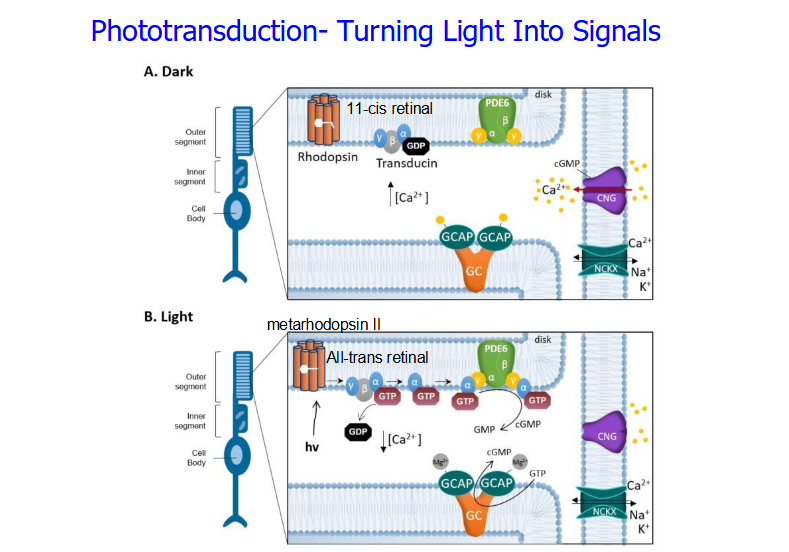
Phototransduction
The process of turning light into signals.
Rods:
There is a key pigment called Rhodopsin
Made of Opsin which is the orange membrane bound protein.
Made of 11-cis retinal which is the light sensitive molecule derived from vitamin a.
Opsin alone can’t detect light, the light detector is 11-cis retinal.
In the dark, the 11-cis retinal is stable and bound to the opsin → Rhodopsin is in its inactive form. In the outer segment, guanylyl cyclase is producing cGMP → binding to CNG ion gated channels → open → influx of calcium and sodium → rod depolarization → glutamate release. NCKX brings sodium and calcium in in exchange for calcium to maintain depolarized state.
In the light, 11-cis retinal isomerizes into an all-trans retinal → opsin gets activated → rhodopsin becomes metarhodopsin II which is its active form → sets off a g-protein cascade that activates g protein called transducin → alpha subunit diassociates → activates PDE6 → cGMP is broken to GMP → cGMP doesn’t bind to CNG → no calcium influx → no depolarization → hyperpolarization → reduced glutamate release → bipolar cells understand that light has been detected.
Normally calcium inhibits GCAP protein → less calcium because of light → no more inhibition → GCAP turns GTP to cGMP → can activate CNG to reset the system.
Cones vs rods
Cones are less sensitive than rods → responsible for vision in bright lights and distinguishing colours. BUT doesn’t operate in dark.
Rods detect single photons but only work in low light.
In daylight, they are bleached out (Rhodopsin is broken so can’t sense light)
But when lights become dim, rods dark adapt, meaning they rebuild rhodopsin over 30 mins.
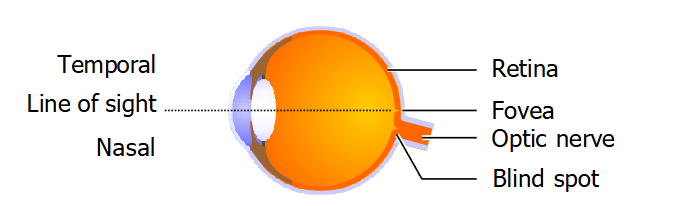
blind spots
The photoreceptors are densely packed into the macula which is a central disc and also into the fovea.
Fovea is used for detailed vision.
Under the fovea is a blind spot with no receptors. This is where axons with the visual information leave the eye and form the optic nerve.
Not noticeable normally because objects in one eye’s blind spots are not in the other eye’s blind spots and your brain fills in the gap.
Convergence
When light comes in, it goes through all those layers, ignoring them and then hits the photoreceptors at the back → photoreceptors synapse onto bipolar cells → bipolar cells synapse onto ganglion cells.
45 photoreceptors can converge into one bipolar cell, condensing the ganglion cells required.
Visual field
The region in the retina where light affects cell activity.
Bipolar cells have a center surround field
Center circle
Donut ring around it
Can be on center or off center
On center = excited by light in the center of the field and inhibited by light around it. Most responsive when surrounding is dark and center is light.
Off center = excited by light around and inhibited by light in the center. Respond best when dark in the middle light around.
On and Off receptor bipolar cells respond differently to glutamate based on the type of receptor they have.
On center receptor has a mGluR6 receptor which is metabotropic → Binding of glutamate makes them less excited → Hyperpolarization
Off center receptor has an AMPA receptor which is ionotropic → Binding of glutamate causes depolarization
If Light in the center → Photoreceptor in the center gets hyperpolarized → Less glutamate release → On center bipolar cell gets depolarized → Transmitter tells on center ganglion cell to fire more. Less glutamate → off center receptors less excited → hyperpolarization → firing of off center ganglion cell decreased. Dark in the surroundings → photoreceptor in the surroundings depolarized → glutamate released → horizontal cells activated → accentuate contrast.
If dark in the center → Photoreceptor in the center gets depolarized → more glutamate released → On center bipolar cell hyperpolarized → less transmitter → less firing of on center ganglion cells. More glutamate → off center bipolar cell depolarized → more transmitter released → more firing of off center ganglion cell. Light in the surroundings → photoreceptor in surroundings hyperpolarized → less glutamate released → horizontal cell activity decreased.
The ganglion cells that are activated start an action potential.
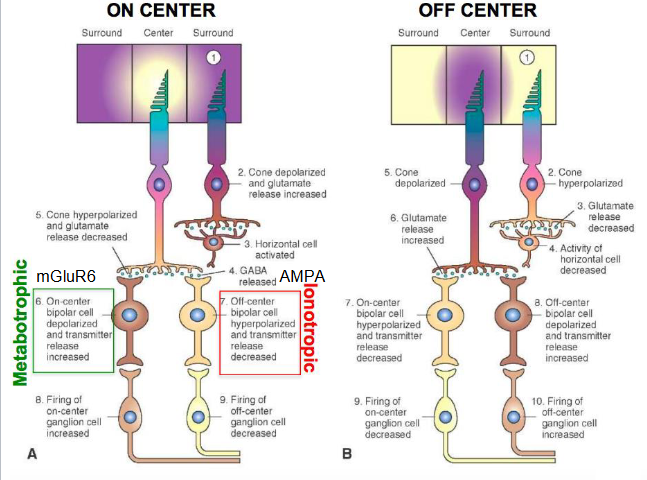
Contrast
When the lighting is uniform, bipolar cells do not react because the effects of the light in the center and surrounding cancel.
But they react when there is contract with a graded potential.
Ganglion cells also detect contrast because they also have on center off center receptive fields.
Ganglion cells
Ganglion cells in different parts of the retina have different receptive fields.
Near the fovea, they get most of their input from not a lot of photoreceptors, but mostly from the cones via bipolar cells → Near the fovea, less sensitive to light but better resolution because information from few receptors.
Further from the fovea, they get input from more photoreceptors and mostly rods → This means in your periphery, ganglion cells are very sensitive to light but bad at detail because so many receptors are giving information.
The ganglion cells are classified based on their signal use
M cells give information about movement
P cells give information about fine details and form like texture
Melanopsin cells have visual pigments called melanopsin that project to the suprachiasmatic nucleus for circadian rhythm
movement of visual information
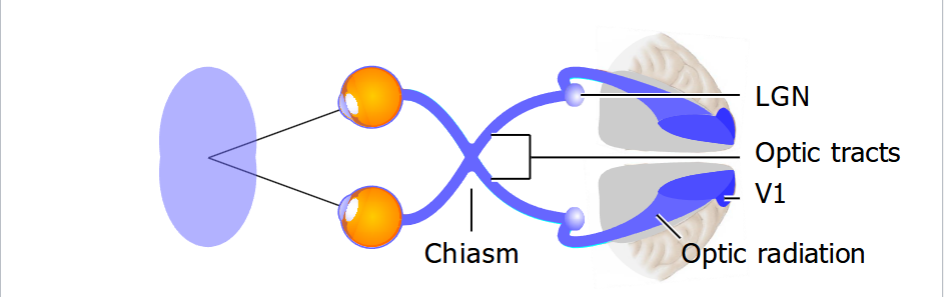
Ganglion cell sends axons out the back of the eye in the blind spot → these axons form the optic nerve (cranial nerve II) → optic nerves from both eyes meet at the optic chiasm → nasal retinal fibers cross to the other side, temporal retinal fibers do not cross → information from the left visual field goes to the right hemisphere, information from the right visual field goes to the left hemisphere → From the chiasm, the nerve bundles are called optic tracts → end in the 2 lateral geniculate nuclei (LGN) in the thalamus → project optic radiations to the primary visual cortex called V1
V1 is in occipital lobe and is responsible for processing visual information
Neuron organization
Neurons are organized retinotopically, meaning neurons close together in the brain get information from the close together parts of the retina.
Color
We see color depending on the wavelength of light.
Diff wavelengths = diff colors.
We can see from 400 nm to 800 nm
Power in the sunlight peaks at these wavelengths
Color cones
We have 3 kinds of cones that let us sense color
Red green and blue
Each type has its own visual pigment that prefers its own wavelength of light.
Red and green cone pigments prefer yellow and yellow green light
Blue cone pigments prefer blue.
Rhodopsin prefers blue green
Melanopsin prefers blue
your brain understands what color you’re looking at by comparing cone data.
This allows your brain to be fooled cuz if there red and green with no yellow, your brain still sees yellow
We can mix the 3 wavelengths to produce any color.
Screens use those 3 lights.
Spectral colors
Evoked by light in 1 wavelength.
Rainbow colors.
Extraspectral colors
Purple and white
Evokes by a mix of wavelengths.
Processing color
Ganglion cells combine cone signals to signal color
R+G cells are excited by red and green light → Called the yellow channel
R-G cells are excited by red but inhibited by green
G-R cells are excited by green but inhibited by red.
Together, the red-green opponent channel.
B-(R+G) cells are excited by blue and inhibited by red and green.
(R+G)-B cells are excited by red and green but inhibited by blue.
Together, the blue-yellow opponent channel.
color blind
Most of color blindness is red green.
Called Daltonism.
Chromosome linked issue
Red and green cones are on the X chromosome
Women are less affected than men cuz 2 X’s so if one is broken the other works.
Reflectance
Tendency to reflect a certain wave length of color and absorb others.
But the light sent to our eyes depends on the illumination too.
If you put a yellow banana in greenlight, it looks green.
But our brain usually understands what the color is away from the light'
Color constancy.
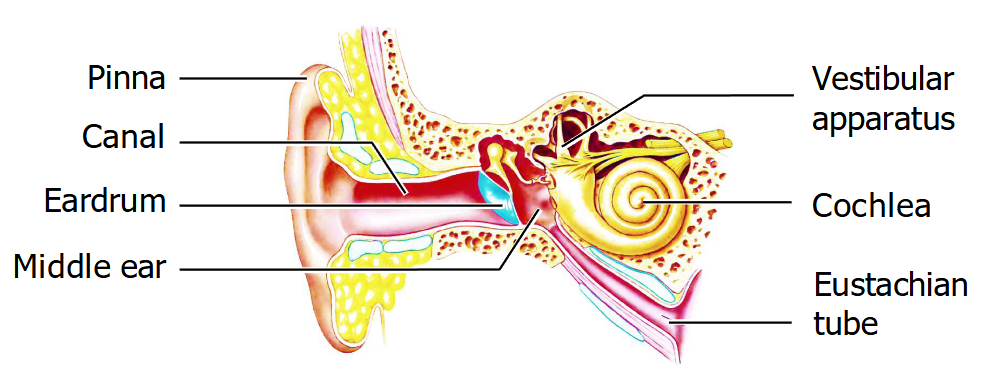
Ear anatomy
The ear has 3 parts
External ear: Pinna and ear canal, and is sealed at the end by the tympanic membrane (ear drum)
Middle ear: Air-filled space made of 3 bones (malleus, incus, stapes) that take vibrations to the oval window. Connected to the pharynx by the Eustachian tube.
Inner ear: Cochlea for hearing and the vestibular apparatus for equilibrium
Hearing
The sound we hear is pressure waves.
At peaks, air molecules are close together → high pressure
At troughs, air molecules are further apart → low pressure
The pitch we hear is frequency.
Low frequency = low pitch
High frequency = high pitch
The loudness we hear is the amplitude.
Larger amplitude = louder sound.
Sound vibrations
Soundwaves cause vibrations in the ear drum (tympanic membrane) → ear drum vibrates the malleus bone (hammer)→ moves the incus (anvil) → moves the stapes (Stirrup) → pushes a piston against the oval window which is a membrane between the middle and inner ear → vibrations enter cochlea with the auditory receptor cells → wave energy exits cochlea → middle ear through the round window.
The 3 bones, malleus incus and stapes, are the ossicles that act as a lever system that carries vibrations to the oval window.
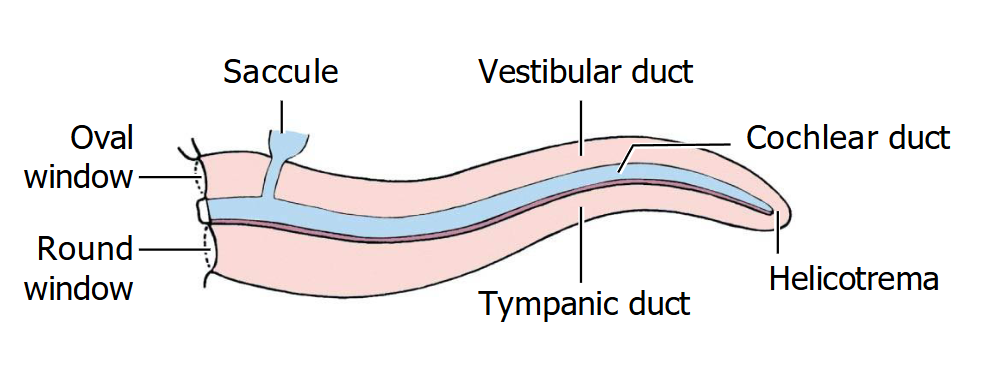
Cochlea
Cochlea is made of 3 ducts
Vestibular duct → perilymph fluid
Tympanic duct → perilymph fluid
Connect at the helicotrema
Cochlear duct → endolymph
Sound waves push against the stapes at the oval window → vibrations in the oval window → transferred to the perilymph of the vestibular duct → tympanic duct → exits to the middle ear through the round window
As the waves are passing through, they shake the cochlear duct which contains auditory receptor cells.
The organ of Corti is within the cochlear duct → contains hair cells (mechanoreceptors) → each hair cell contains stiffer hairs called stereocilia → these stiff air cells bend when waves in the perilymph cause the basilar membrane to move.
If the stereocilia bend toward the tallest cillium, the hair cells depolarize → neurotransmitter released → primary sensory neurons activated → axons form the auditory nerve which is part of cranial nerve VIII
If stereocilia bend away from the tallest cillium, the hair cells hyperpolarize → less neurotransmitter released → less neuron excitation
Basilar membrane
At different locations, the basilar membrane responds to different frequencies’
Near the oval window, there are high frequencies so the membrane is stiff and narrow.
Near the helicotrema, there are low frequencies so the membrane is wider and more flexible.
This pattern tells the brain the pitch
Auditory pathway
Auditory signals received by each ear go to both sides of the brain.
Cochlear hair cells → auditory nerve → cochlear nuclei in medulla → midbrain → MGN of the thalamus → primary auditory cortex (A1) in the temporal lobe
The timing and loudness of sound allows your brain to understand which side the sound is coming from
Louder in the right ear than left → coming from right side of the head
Loudness = more neurons fired at a faster rate
If the sound reaches the right ear before the left, coming from the right side.