Week 3: Anterior/ Posterior Pituitary
1/139
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
140 Terms
What is the feedback control for the thyroid gland?
hypothalamus → TRH → (+) anterior pituitary (thyrotrophs) → TSH → (+) thyroid gland → T4/T3 → has its effects on the body
T4/T3 → (-) anterior pituitary thyrotrophs & (-) hypothalamus
TRH in excess can stimulate lactotrophs to release PRL
What are the 3 effects of stimulating TSH-R on the thyroid gland?
growth of thyroid gland
increased T4/T3 synthesis
increased Na+/ I- symporter activation
What is the importance of I- ?
iodine is important for making thyroid hormone (T4/T3)
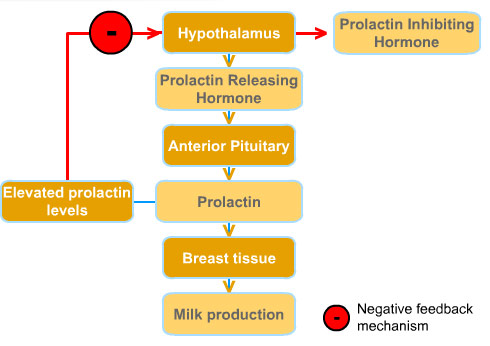
What is the feedback control for prolactin?
hypothalamus → DA → (-) anterior pituitary lactotrophs → prolactin → (+) milk production
estrogen → (+) anterior pituitary lactrotrophs → prolactin → (+) milk production
excess TRH can also stimulate (+) anterior pituitary lactrotrophs → prolactin → (+) milk production
What is hyperprolactinemia?
high levels of PRL in blood
What are the 5 cell types of the anterior pituitary?
corticotrophs
gonadotrophs
somatotrophs
thyrotrophs
lactotrophs
What do each of these 5 cell types release when stimulated by hypothamalic releasing hormones?
corticotrophs → ACTH
gonadotrophs → FSH/LH
somatotrophs → GH
thyrotrophs → TSH
lactotrophs → PRL
What are the 2 hypothamalic releasing hormones that act on lactotrophs?
TRH (excess) → stimulatory
DA → inhibitory
Describe the roles of TRH, DA, and ER (estrogen receptor) on lactotrophs
TRH → in EXCESS amounts, can stimulate secretion of PRL
DA → MAJOR regulatory hormone; inhibits PRL secretion
ER → stimulates secretion of PRL
What are the 5 major causes of hyperprolactinemia?
prolactinoma (lactrotroph adenoma/tumor)
decreased DA inhibition
increased ER stimulation
increased TRH receptor stimulation
other drugs
How does prolactinoma contribute to hyperprolactinemia?
something is wrong with the lactotroph that is causing it to make more of a hormone it typically makes (excess PRL)
What are the 3 things that can cause decreased DA inhibition, leading to prolactinemia?
pituitary stalk damage
hypothamalic damage
D2 receptor antagonists/anti-psychotics/other drugs
Why does pituitary stalk damage lead to increased PRL secretion?
the pituitary stalk is what carries DA from the hypothalamus to the anterior pituitary
if the pit stalk is damaged, DA can’t get to the lactotrophs in the ant pit to inhibit
What are the 2 things that can cause increased estrogen receptor stimulation?
combined hormonal contraceptives
pregnancy
How do oral contraceptives & pregnancy contribute to increased PRL?
increased levels of estrogen = increased estrogen receptor stimulation and PRL secretion
What is the name of the disease state that causes increased TRH receptor stimulation and how?
1 hypothyroidism
leads to decreased T3/T4 = decreased (-) feedback to TRH = increased TRH (+) of lactotrophs
What are the 2 primary affects we see in hyperprolactinemia?
galactorrhea
decreased sex steroids (hypogonadism)
Describe how we get galactorrhea from PRL secretion?
PRL acts on breast tissue → milk production → galactorrhea
Describe how we get decreased sex steroids from PRL secretion?
PRL leads to decreased GnRH release → decreased LH/FSH (gonadotropins) → decreased sex steroids and gonad function
What does hyperprolactinemia present as in premenopausal women? (3 main presentations)
infertility (no ovulation)
amenorrhea (no menses)
galactorrhea
What are the 3 typical symptoms seen in women due to decreased estrogens?
hot flashes
vaginal dryness
decreased bone mineral density
Why is it harder to detect decreased ovarian estrogen symptoms in post-menopausal women?
they usually already exhibit these symptoms because they are menopausal symptoms
What does hyperprolactinemia present as in men? (3 presentations)
infertility
gynecomastia
galactorrhea
What are the 4 typical symptoms decreased testicular androgens?
decreased libido
decreased muscle mass
erectile dysfunction
decreased bone mineral density
What is the extra clinical finding that can occur if hyperprolactinemia is caused by a lactotroph adenoma (ant pit tumor)?
Bitemporal Hemianopia
What is Bitemporal Hemianopia?
loss of the peripheral field vision of BOTH eyes
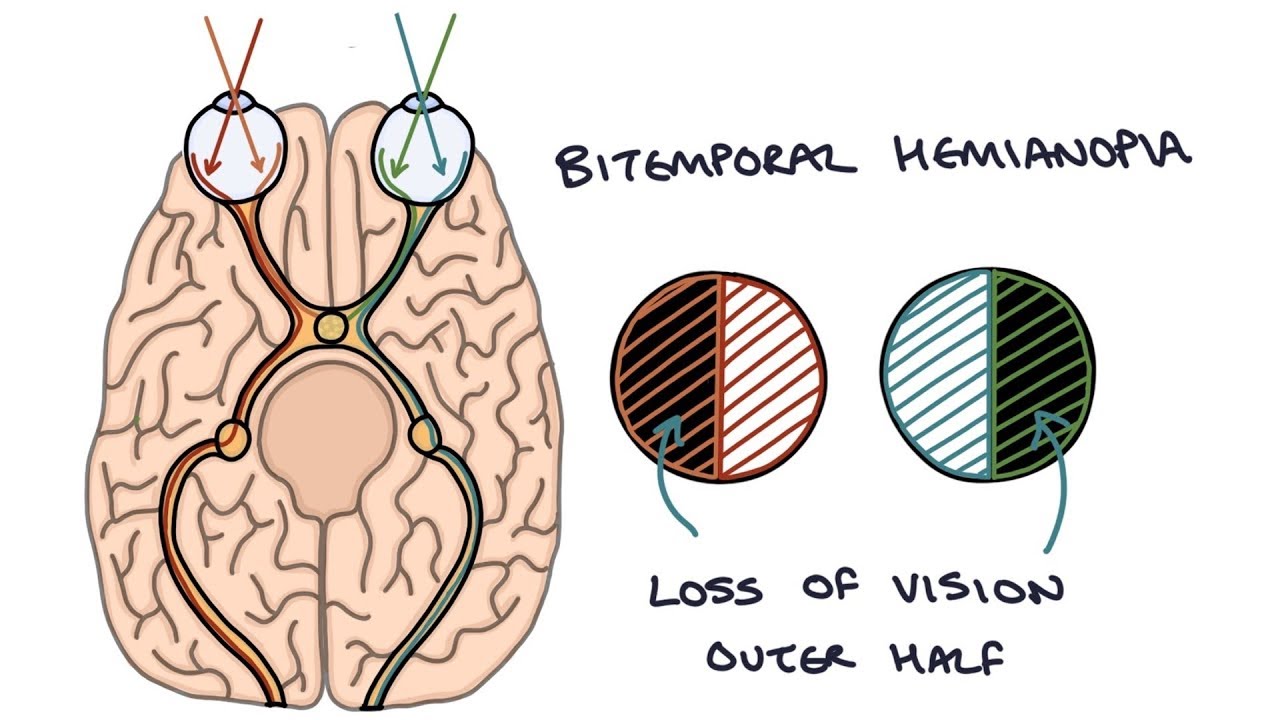
How does bitemporal hemianopia happen?
as the ant pit tumor grows UPWARDS from BELOW the optic chiasm, it compresses the OPTIC CHIASM
the optic chiasm carries peripheral visual field information from both eyes → compression leads to loss of peripheral vision
What does the peripheral vision loss initially look like when the tumor first begins to grow?
initially impacts the upper vision fields first
the upper vision fields travel through the bottom of the optic chiasm
What are the 2 additional symptoms we can get due to the lactotroph adenoma in the ant pit?
headaches
mass effect of decreased ant/pit hormones
Why do we see a mass effect of other hormones being decreased with an ant pit tumor?
as the tumor grows, the other cell types by the tumor become crowded out and can become damaged
What are the 2 main methods of treating hyperprolactinemia caused by prolactinoma?
Pharmacological treatment
surgical treatment
What are the 2 classes of pharmacological drugs used for treatment?
DA receptor agonists
hormone replacement
What are the names of the 2 DA receptor agonists?
Cabergoline
Bromocriptine
What is the MOA of Cabergoline/Bromocriptine?
inhibit PRL secretion and decrease the size of the tumor
What are the 3 main AEs of DA-R agonists?
nausea/vomiting
orthostatic/postdural hypotension
impulse control symptoms
Why do we get impulse control symptoms with DARAs?
DA is involved in the reward system → when stimulated it could cause these issues
What are the 2 impulse control symptoms we would see with DARAs?
hypersexuality
pathological gambling/shopping
How do we prevent development of these behavioral changes?
take DARA at a lower dose
What is an additional AE of Cabergoline?
VALVULAR HEART DISEASE (regurgitation/stenosis)
What is the name of the receptor involved in cardiac valvulopathy as an AE of Cabergoline? Where is it located?
5HT2B receptor located on heart valves
What are the 2 different hormones that can be given to a man or woman as treatment of prolactinoma? Why are they given?
estradiol + progestin → women
testosterone → men
given to REPLACE the hormones that are low due to high PRL supressing them
If the patient were worried about their fertility, what additional thing should we do to preserve that?
have to suppress PRL in addition to replacing the missing hormones to get the gonads to work again
What is the name of the surgery that is done as treatment for prolactinoma?
transsphenoidal surgery → removal of tumor
What is Acromegaly/Gigantism?
disorder caused by the pituitary gland production of too much growth hormone
What are 4 causes acromegaly/gigantism?
somatotroph tumor
GHRH tumor
IGF-1 tumor
exogenous GH
What does a somatotroph tumor lead to (in terms of hormone production)?
increased GH = increased IGF-1
What is the feedback control for growth hormone?
hypothalamus → SST and GHRH → SST (-) anterior pituitary somatotrophs / GHRH (+) ant pit somatotrophs → (+) GH → liver → IGF-1 and glucose
IGF-1 → (-) ant pit & hypothalamus (release of GHRH)
IGF-1 → (+) hypothalamus (release of SST)
glucose → (-) ant pit somatotrophs

What is a common cause of a somatotroph tumor?
a mutation in the GTPase enzyme that keeps GHRH signaling ON → causes lots of growth and GRH release
What type of GPCR is GHRH-R coupled to?
Gs
What type of GPCR is SST-R coupled to?
Gi
Describe the normal function of GHRH-R stimulation
GHRH binds its receptor on somatotroph → Gs-GTP active stimulates AC → increases cAMP/PKA → PKA stimulates GRH release and growth of somatrophs
GTPase typically makes Gs-GTP inactive to Gs-GDP
What does a GHRH tumor cause (in terms of hormone levels)?
increased GHRH = increased GH = increased IGF-1
What does an IGF-1 tumor cause (in terms of hormone levels)?
increased IGF-1 = negative feedback to decrease GHRH = decreased GH
What does exogenous GH cause (in terms of hormone levels)?
increased IGF-1
What are the 5 categories of clinical findings we’d see in someone with acromegaly/gigantism?
skin/soft tissue proliferation
bones/joints stimulated to grow
other places enlarge
metabolic
CV disease
What are the 3 clinical findings we see due to skin/soft tissue proliferation?
increased sweating/oily skin
heat intolerance
fatigue
What are the 5 clinical findings we see due to bones/joints being stimulated to grow?
degenerative arthritis
thickening skull
enlargement of jaw
increased hand/feet size
carpel tunnel syndrome
What is the term for thickening skull called?
frontal bossing → frontal bones enlarged
What is the term for enlargement of the jaw called?
macrognathia
Why do we get carpel tunnel syndrome?
when the bones grow, they entrap the median nerve in the wrist and cause damage
What are the the 2 other places that can enlarge?
increased tongue size
increased organ size
What is the term for enlarged heart?
visceromegaly
What are the 3 clinical findings we can see due to CV disease/visceromegaly?
hypertension
cardiac hypertrophy (muscle thickening)
HF
What is the most common cause of death in patients with acromegaly?
HF due to enlarged heart valves
What is the metabolic associated clinical finding we see?
increased blood glucose (due to high GH)
Which type of cancer is at increased risk with high GH levels?
colorectal cancer
What clinical finding would we see in someone with increased GH/IGF-1 secretion before the epiphyseal/growth plates close?
GIGANTISM → dramatic increase in linear height
Describe the 3 extra clinical findings that could occur if a patient has a somatotroph tumor
bitemporal hemianopia
headaches
mass effect of decreased ant pit hormones
Describe the roles of SST and GHRH on somatotrophs
somatotroph has SST and GHRH receptors
GHRH (Gs) → release of GH → increases IGF-1 → effects
SST (Gi) → inhibits GH → no IGF-1
What are the 2 medications used for treating the somatotroph GH secreting tumor?
Octreotide
Peguisomant
What is the MOA of Octreotide?
somatostatin receptor agonist
What are the 2 beneficial effects of Octreotide?
shrink somatotroph tumor
decrease GH release
What are the 4 AEs of Octreotide?
nausea
abdominal bloating
fat malabsorption
gallstones
Why do we see GI related effects with Octreotide?
SST plays a role in the GI tract to inhibit some normal processes in the GI tract
Why do we get gallstones with Octreotide?
due to decreased CCK and decrease gallbladder contraction
What is the typical role of CCK and why does its downregulation lead to gallstones?
CCK = cholecystokinin
GI hormone that contracts bile bag to release bile acid for fat digestion
if decreased CCK = decreased contraction = gallstones bc decreased bile acid
What is the MOA of Peguisomant?
GH receptor antagonist
What are the 2 beneficial effects of Peguisomant?
blocks the effects of GH
decreases IGF-1 (which typically drives growth)
What is the AE of Peguisomant?
hepatotoxicity
Why can we sometimes use Cabergoline/Peguisomant as an add on with Octreotide?
octeotride = tried first
add on other drugs if octeotride doesn’t work bc sometimes DA receptor stimulation by a tumor could be the cause for increased GH
Which surgery could be done to remove the somatotroph tumor?
transsphenoidal tumor removal surgery
In someone with a somatotroph tumor, why is it not helpful to block GHRH?
GHRH is not typically driving the problem with a somatotroph tumor → GHRH is typically LOW due to (-) feedback
the problem is increased GH
What is the name of the posterior pituitary hormone that is synthesized in the hypothalamus?
ADH - antidiuretic hormone (acts on the kidney)
Which body system does ADH control? Through which receptors?
plasma osmolarity
V2 (Gs coupled) receptor on the kidney for water reabsorption
V1 (Gq coupled) on vascular smooth muscle for vasoconstriction
When Posm increases, ADH ____ and H2O reabsorption ___
ADH increases and H2O reabsorption increases
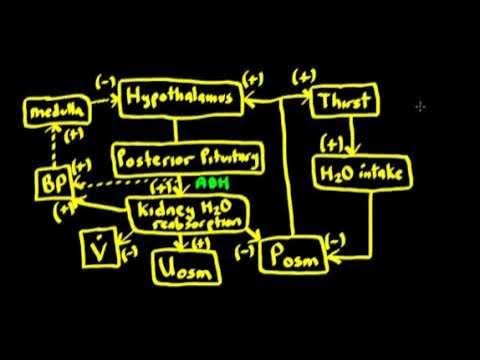
Draw the feedback control system Posm and BP
hypothalamus sends ADH down to the pituitary gland through the pituitary stalk → posterior pituitary releases ADH →
(+) kidney (H2O reabsorption) → (-) V (urinary flow rate) / (+) Uosm / (-) Posm → (+) hypothalamus / (+) thirst → (+) water intake → (-) Posm
(+) kidney (H2O reabsorption) → (+) BP → (+) medulla → (-) hypothalamus
ADH also has (+) effects on BP through V1
Describe what happens when ADH from the blood binds the V2 receptor on the CD of the kidney
ADH binds V2 on CD → V2 (Gs) → increase cAMP/PKA → PKA stimulates insertion of AQII channels onto the apical membrane → H2O from tubular fluid is REABSORBED
What is the role of ENaC in the CD? Which ions can enter?
it is responsible for Na+ gradient into the CD
Li+ can enter ENaC and cause disruption Gs signaling
What is SIADH?
syndrome of inappropriately HIGH ADH
Why do you have to be careful with drinking excess water with SIADH?
could get HYPONATREMIA
too much ADH = excess water reabsorption and dilution of plasma sodium
What are the 3 main causes of SIADH?
CNS disturbances
malignancies
drugs
How does a CNS disturbance contribute to SIADH?
something in the CNS could be damaged and cause excess ADH release
How do malignancies contribute to SIADH?
ECTOPIC ADH secretion from a tumor
What does ectopic secretion mean?
ADH production is happening from a source that doesn’t usually make ADH
What is an example of a malignancy that could secrete excess ADH?
lung tumor
What are examples of 2 drugs that could increase ADH release, even with low plasma osmolarity?
SSRIs and ecstasy
How do SSRIs and ecstasy cause excess ADH?
SSRIs → block 5HT reuptake
ecstasy → increase 5HT release
5HT stimulates SST → which leads to increased ADH release
What happens to plasma sodium with SIADH?
due to excess ADH → taking in extra water and unable to get rid of it = HYPONATREMIA
What are the effects of hyponatremia on the brain?
it causes neurological dysfunction from swelling neurons
with hyponatremia, we have low Na+ outside the cell but increased water going in to the cell to reach equilibrium→ causes swelling of the neuron
What is the severity of the neural swelling dependent on? (2 things)
MAGNITUDE and how QUICKLY we decrease PNa+