OP: Potentially malignant lesions
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
Leukoplakia Definition
White patch / plaque of questionable behaviour that cannot be characterised clinically / pathologically as any other disease, clin dx defined by exclusion of other white
Differential diagnosis of leukoplakia
o lichen planus,
o oral hairy leukoplakia
o leukoedema,
o frictional hyperkeratosis,
o tobacco pouch
o keratosis,
o stomatitis nicotinica,
o white sponge naevus
8 Clin Features of leukoplakia
o Male predilection
o >40years, Mean age: 60 years (5 years younger than pt’s w/ OSCC)
o >90% tongue, lip vermilion, FOM show dysplasia/carcinoma
o Early lesions: slightly elevated, grey- white plaques
o Fissured, wrinkled, soft/ flat, sharply demarcated borders
o Mild / thin leukoplakia seldom shows dysplasia
o Continued tobacco habit grows 2/3 larger, thicker & white, deepening of fissures
o May change from dysplastic→ SCC w/out change in clin appearance
What is the aetiology of lekoplakia?
o Tobacco (80%) ▪ Lesions get smaller/disappear 1st year cessation
o Alcohol ▪ Synergistic effect w/ tobacco
o Betel quid (areca nut, betel leaf, slaked lime)
o Sanguinaria ▪ Herbal extract found in toothpaste/mouth rinses ▪ Malignant potential = uncertain
o UV light ▪ sun-exposed skin • Lower lip ▪ Esp. in fair skinned, immunocompromised, transplant patients
o Iron deficiency ▪ Plummer- Vinson Syndrome ▪ ↑ risk of malignant transformation in oesophagus, oropharynx, post. mouth • impais immunity & function of epithelial cells
o Vitamin A deficiency: play protective/preventative role
o Syphilis,
o Micro-organisms ▪ Candidal leukoplakia and HPV 16,18
o Immunosuppression: HIV / immunosuppressive therapy(corticosteroids)
o Trauma ▪ Stomatitis nicotinica, risk of malignant transformation is low vs Reverse smoking stomatitis nicotinica ↑ risk
Clinical Types of Leukoplakia
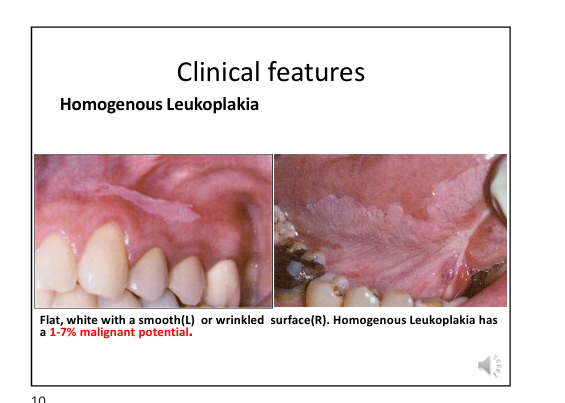
Homogenous leukoplakia
Clinical Features: ▪ Flat, white w/ smooth/ wrinkled surface, has 1-7% malignant potential.
Non homogenous leukoplakias
Erythroleukoplakia
Clin Features: ▪ Speckled leukoplakia (white & red lesion) predominantly white surface on buccal mucosa & ventral surface of tongue, has18-47% malignant potential.
Nodular leukoplakia
Clin Features: ▪ High recurrence rate, high surface irregularity, small rounded nodular red&white outgrowths
Verrucous leukoplakia
Clin Features: ▪High recurrence rate, 4-15% malignant potential, wrinkled & corrugated surface projections
Give clinical features of Proliferative verrucous leukoplakia(PVL)
-Aggressive, Persistent growth, High recurrence rates
( almost all undergo malignant transformation)
-No tobacco association
-Strong female predilection(1:4)
-gingiva, ridge, buccal
-Early lesions – single, simple, flat hyperkeratosis, Spread slowly to involve multiple sites (resembles homogenous at first)
-Late lesions – exophytic, keratotic plaques, rough surface projection(verrucous), eventually evolve to squamous cells carcinoma
Histopathological Features of different leukoplakias
Leukoplakia
▪ hyper ortho/parakeratosis
▪ with/out acanthosis ▪ atrophy
▪ Dysplasia: Loss of uniformity of architecture and disordered maturation
▪ Squamous cell carcinoma
Verrucous leukoplakia
▪ Papillary/exophytic projections
▪ Blunted rete ridges
PVL
▪ Hyperkeratosis
▪ Papillary/exophytic proliferations
▪ Broad, blunt rete ridges
▪ Invasion into lamina propria
▪ Invading epithelium less well differentiated -SCC
NB: Clinicopathological correlation for accurate Dx
Histopathological Features: Dysplastic Epithelium
▪ The more dysplastic the epithelium, more atypical changes involving full thickness of epithelium
(Dysplastic epithelial cells features similar SCC, difference is SCC is infiltritive and dysplastic is localised)
• Enlarged nuclei & cells, prominent nucleoli, and ↑ N:C ratio
• Hyperchromatic and pleomorphic nuclei
• Dyskeratosis
• ↑Mitotic activity thus abnormal mitotic figures
What are the Histomorphological changes of dysplastic epithelium?
Differentiate the changes between the different dysplasia
1. Bulbous rete ridges 2. Loss of polarity 3. Keratin/epithelial pearls 4. Loss of typical epithelial cohesiveness
▪ Mild Dysplasia: Changes extend lower 3rd of epithelium, and lowest malignant potential
▪ Moderate Dysplasia: Changes extend to middle 3rd of epithelium, 4-11% malignant potential
▪ Severe Dysplasia: Changes extends to upper 3rd of epithelium, malignant potential 20-35%
▪ Carcinoma-in-situ: Full thickness dysplastic alteration, no invasion, no breach of BM (yet), hyperplastic/atrophic epithelium
▪ 1 in 3 dysplasia's recur
Tx & Prognosis of leukoplakia
Leukoplakia
▪Definitive dx required, biopsy will guide treatment, must be most clinically severe area of lesion, multiple biopsies may be required.
Mild dysplasia
▪ Smoking cessation ▪ No dysplasia observation 6 monthly
Moderate/severe dysplasia
▪ Surgical excision/ electrocautery/ cryosurgery/ laser ablation
What is Erythroleukoplakia?
How do we obtain the diagnosis?
DDx (3)
Clinical features (2)
Histopathological Features (4)
Treatment & Prognosis (7)
Definition: 1.Red patch that cannot clinically/pathologically be Dx as any other lesion 2. Assoc. w Leukoplakia 3. Risk of malignant transformation linked to degree of dysplasia 4. Often shows severe dysplasia, Carcinoma-in situ on biopsy 5. Rarer 6. Found in old man (65-74 years) 7. Floor Of Mouth, tongue & soft palate.
Definitive Dx: biopsy needed
Clinical DDx: candidiasis, nonspecific mucositis, vascular lesions
Clin Features: well demarcated erythematous macule, plaque velvety texture. Redness from immature epithelial cells, can no longer produce keratin.
Histopathological Features: 1. 90% are severe dysplasia/Ca-in-situ, superficially invasive SCC 2. Atrophic epithelium 3. Lack of keratinisation & atrophy allows underlying microvasculature to show through 4. May be hyperplastic 5. Chronic inflam.
Tx & Prognosis: 1. High suspicion index, biopsy, guided by definitive Dx. 2.Moderate/ severe dysplasia needs surgical excision
3. Scrutinize to exclude focal invasive SCC
4. Recurrence w/ multifocal involvement
5. Long term follow up indicated
Describe Smokeless tabacco keratosis
Clinical Features: White plaque, gingival recession, loss of alveolar bone, tobacco stained teeth, and halitosis.
Histopathological Features: Hyperkeratosis, acanthosis, spongiosis. Parakeratin chevrons. Increased subepithelial vascularity. Mild epithelial dysplasia.
Tx & Prognosis: Low malignant potential. Biopsy only severe/advanced lesions: induration, ulceration, verruciform and haemorrhage
Oral Submucous Fibrosis
Is a chronic disease that affects oral mucosa as well as pharynx & upper 2/3rds of oesophagus. High-risk precancerous condition
Aetiology & pathogenesis:
Chronic irritation: From Betel nut, i.e., areca nuts (alkaloids) , chillies capsaicin (active ingredient causing irritation) tobacco, lime, areca nut, quid chewing habit & development of OSMF = dose dependent
Clin Features:–Palpable fibrous bands–Tough and leathery mucosa–Blanching of mucosa
Age & sex: Equally affects both in 2nd and 4th decade
Site: buccal mucosa (98%) & retromolar areas, soft palate (49%) palatal fauces, uvula, tongue & labial mucosa.
Prodromal symptoms: Onset is insidious over 2- to 5-year duration. Common initial symptom, burning sensation of oral mucosa, aggravated by spicy food followed by either hypersalivation/dryness.1st sign = erythematous lesions, followed by paler mucosa. Later disease fibrotic bands located beneath atrophic epithelium. ↑ fibrosis → trismus. Atrophic epithelium.
Histopathologic features-atrophic epithelium, hyalinization of lamina propria
Dx: Based on clin features & report of habit of betel quid chewing.
Tx: o Stop areca nut chewing habits lesions may regress. Supportive treatment Vitamin rich diet and iodine, B-complex preparations.
Sideropaenic Dysphagia
• Severe chronic iron deficiency→ impaired cell mediated immunity
• ↑ epithelial turnover→ production of immature mucosa
• → Elevated risk for SCC of oesophagus, oropharynx, post. oral cavity. Pt’s have oesophageal webs which ↑ malignant potential.
NICOTINE STOMATITIS
Causes: Cigar and pipe smoking. Heat induced, hot beverages. Reverse smoking: ↑ malignant potential.
Clinical Features: Male predilection, >45 yrs, diffuse white palatal mucosa, elevated papules w/ punctate red centres.
Histo Features: Hyperkeratosis, Acanthosis, Squamous metaplasia Epithelial hyperplasia, dysplasia rarely seen Mild patchy chronic inflam, .
Tx & Prognosis: Reversible upon cessation of habit, no tx required, persistence of lesion for >1month post habit cessation, = true leukoplakia & must treated accordingly
ACTINIC CHEILITIS
• Common potentially malignant lesion of lower lip vermillion
• Long term/excessive UV light exposure, esp. in setting of immunosuppression → p53 gene mutations
• Fair skinned individuals called farmer’s/ sailor’s lip
• Prevalence ↑ w/ advancing age
Clin Features: >45 yrs, male predilection, atrophy of lower lip vermilion border, blurring of vermillion-cutaneous border, with rough scaly areas. Persistent focal ulceration suggests malignant transformation.
Histo Features: Atrophic stratified squamous epithelium, Hyperkeratinisation, Epithelial dysplasia, Solar elastosis.
Tx & Prognosis: Changes irreversible, lip balms with sunscreen, biopsy areas of ulceration, induration, leukoplakia. Lip shave/vermilionectomy. SCC – surgical excision. Recurrence = rare. Additional lesions in adj. sun damaged skin. Long term follow up