Asthma & COPD
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
What is obstructive lung disease manifested by?
Increase resistance to airflow
What are examples of obstructive lung disease?
Asthma
Emphysema
Bronchitis
Cystic Fibrosis
What does restrictive lung disease result from?
Decreased lung expansion due to alterations in lung tissue, pleura, chest wall or neuromuscular function
What is an example of restrictive lung disease?
Pneumonia
What is Asthma?
A Chronic obstructive lung disease
What are characterizations of asthma?
-Airway inflammation
-Reversible airway obstruction
(either spontaneous or w/ Tx)- but may not always e fully reversible
-Airway hypersensitivity + Hyperreactivity = Hyperresponsiveness
-Airway remodeling over time
How can we test reversibility of airway obstruction?
By administering a bronchodilator during a pulmonary function test
What is airway hypersensitivity?
When bronchial smooth muscle shows increased response to even low doses of a stimuli
What is airway hyperreactivity?
When bronchial smooth muscle constricts way more stronger in response to a stimuli
Is asthma episodic?
Yes, it tends to be episodic w/ acute exacerbations & symptom-free periods
Spasmodic bronchial contractions are manifested by which symptoms?
-Paroxysmal diffuse wheezing
-Dyspnea
-Cough
-Tightness sensation in the chest
What is the pathogenesis of asthma
1. Initiation: from a combination of genetics & environment.
-symptoms usually begin during childhood
2. Damage to lower airways due to inhaled agents (includes ETS, environmental tobacco smoke)
-Will stimulate abnormal immune response in susceptible individuals
3. Over time, the recurrent episodes & aberrant repair leads to:
-Sustained presence of inflammatory cells & mediators
-Airway remodeling
-Airway hyperresponsiveness (AHR)
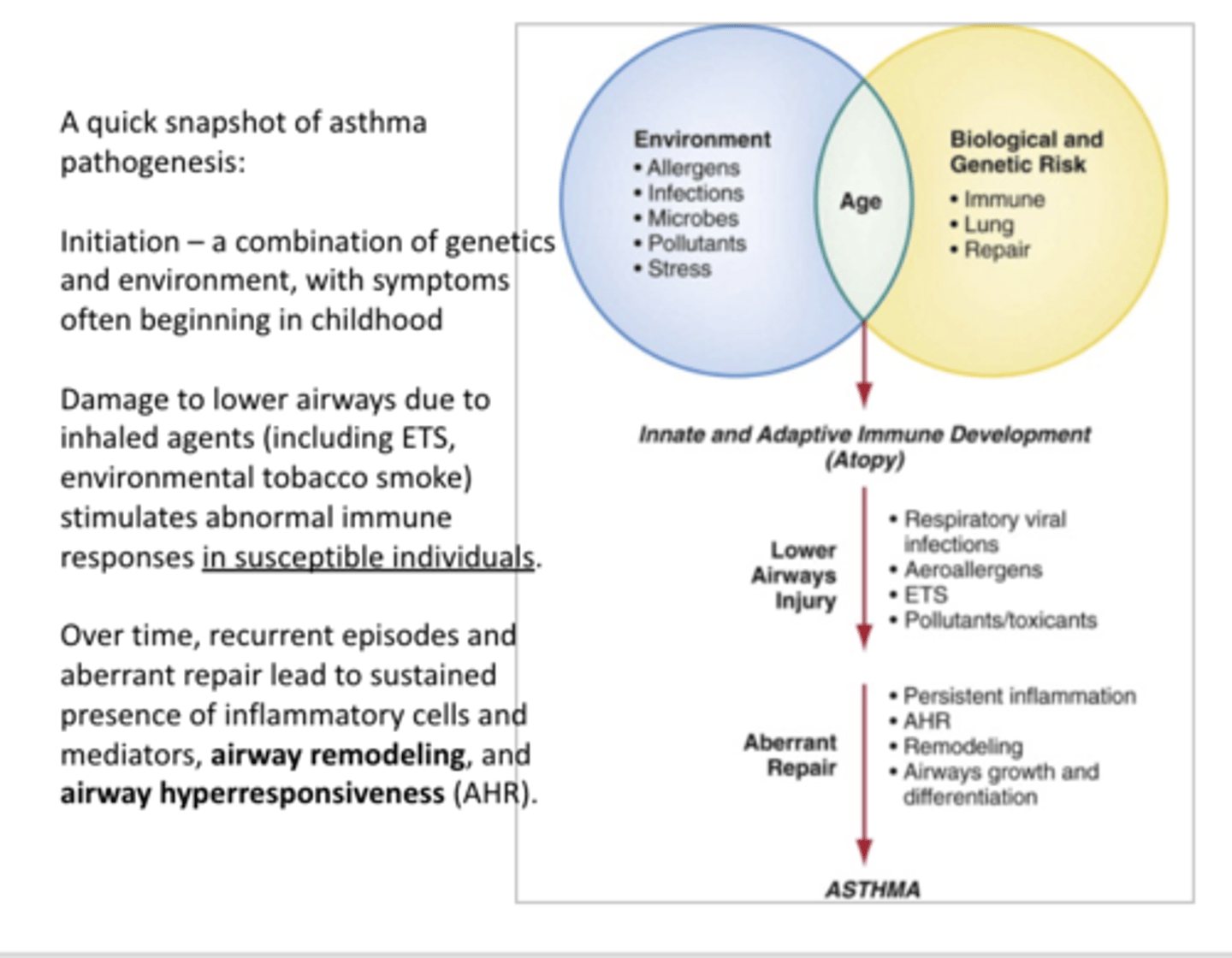
What is one of the most common chronic diseases of childhood?
Asthma
-Its severity can vary from child
What is different about children airways compared to adults?
Children have narrower airways can causes inflammation to have a greater effect on them
What are some environmental contributors to asthma?
-Pollution in industrial areas or highways
-Mold
Can asthma be fatal?
Yes
When do most adult cases of asthma develop?
Before 25, but can still occur throughout lifespan
What most adult cases triggered by?
Many adult cases are non-atopic
Triggered by:
-Viral infections
-Drug induced (aspirin-sensitive asthma)
-Occupational asthma
-Exercised induced bronchoconstriction (EIB)
What are risk factors for developing asthma?
-Family Hx (parent w/ asthma)
-Severe or recurrent respiratory infections (esp. during early life)
-Allergies: atopic dermatitis (eczema) or allergic rhinitis (hay fever); hygiene hypothesis
-Smoking, maternal smoking or secondhand smoking
-Exposure to cockroach allergens or dust mites
-Air pollution
-Obesity (connection w/ inflammation)
-Poverty
-Urban environment vs. rural
-Occupational exposure to dust, fumes , vapors or molds
-Mode of delivery (c-section make increase risk more than vaginal delivery)
-Gut microbiota dysbosis
-Race/Ethnicity
-Genetics
How does gut microbiota dysbosis increase the risk of asthma?
-Gut microbiota role is to train the immune system to recognize pathogens vs. "friendly" bacteria
-Gut microbiota dysbosis is implicated w/ development of allergies & asthma b/c is skews the helper T-cells toward the increased type 2 T-H cells
-Atopy (allergy) is a/w decrease in gut microbiota diversity & decreases butyrate-producing bacteria (which normally keeps epithelial cells healthy)
What is Atopy
A predisposition toward developing allergic hypersensitivity
-Includes development of IgE antibodies to specific antigens
-Typically a/w heightened immune responses to common allergies
What are the two types of asthma?
Allergic & Non-Allergic asthma
Can a pt have both types of asthma?
Yes
-Many symptoms of non-allergic & allergic asthma can be the same but their triggers are different
What can trigger the symptoms of non-allergic asthma?
-Cold air
-Viral or bacterial infection
-Exercise
-Related conditions like gastroesophageal reflux disease (GERD)
What are common triggers of asthma?
-Pollen
-Mold
-Dust mites, cockroach feces & saliva
-Pet dander
-Upper respiratory infections
-Cigarette smoke
-Pollution
-Perfumes, strong scents
-Food allergies
-Cold
-Exercise
-Stress
-Pregnancy
-Menstrual cycles
-Aspirin, other NSAIDs
What is allergic asthma also known as?
Atopic asthma
-Most common form of asthma
What are symptoms of atopic asthma triggered by?
Exposure to an allergen to which the person is sensitized to
(Type 1 Hypersensitivty)
What is the allergic response mediated through?
IgE Antibodies
What are the phases of Atopic Asthma?
Early and Late phase (late is about 6 hrs. after early)
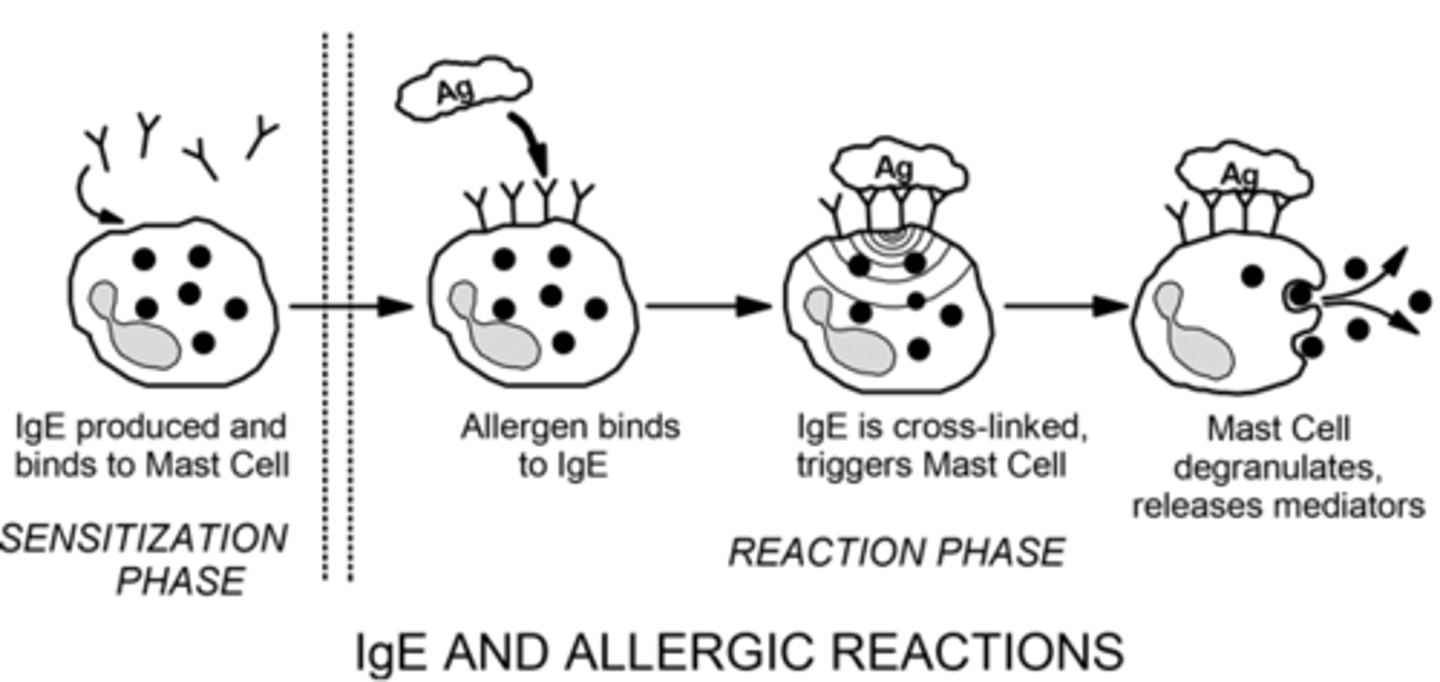
Review of Type 1 Hypersensitivity
1. Initial exposure to allergen
2. Activation of T-H2 cells & B cell class switching to IgE
3. IgE binds to mast cell receptors (they are now "primed")
4. Subsequent exposure to allergen causes 2 IgE antibodies to cross-link -> mast cells degranulation & release of histamine, leukotrienes & other mediators
-Response can be divided into early (immediate) & late phase
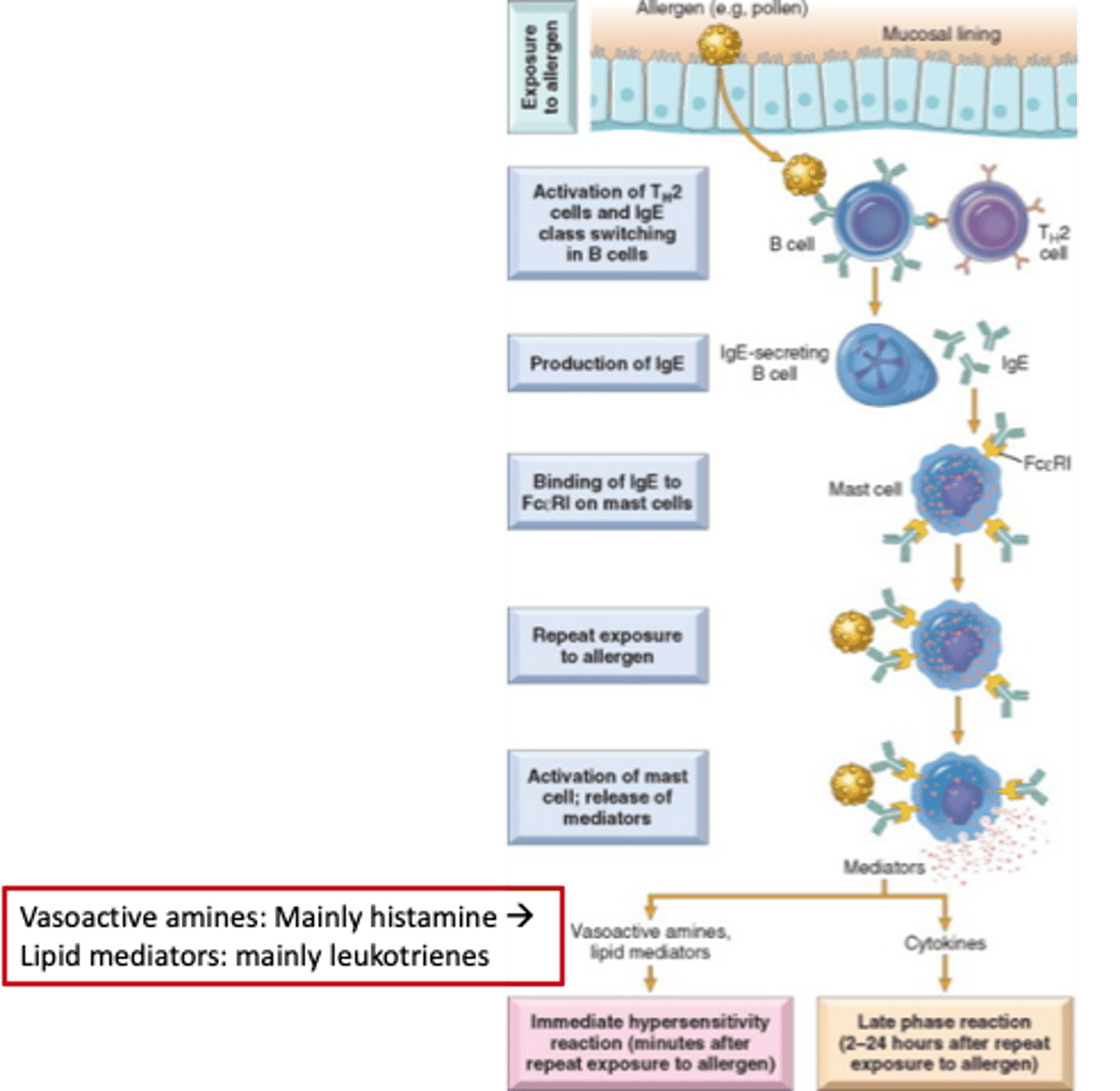
What is the importance of IgE in Allergic /Type 1 hypersensitivity rxn during first & second exposure?
First exposure: IgE is produced & binds to mast cell
Second & subsequent exposures: allergens will bind to IgE -> IgE is cross-linked, triggers Mast cell -> Mast cell degranulates, releases mediators
What are key cellular components of atopic asthma pathogenesis?
-T helper lymphocytes (specifically type 2 T-H cells)
-B lymphocyte & antibody production
-> type 2 T-H cells can cause B cells to change from IgG to IgE production (class-switching)
-Mast cells & basophills (histamine-containing)
-Eosinphils (strong a/w atopy); key "bad actors" of late phase of an asthma attack
-Macrophages & neutrophils (classic inflammatory leukocytes)
What is the role of Type 2 T helper cells?
Releases IL-4, IL-5 & IL-13 cytokines w/ many effects that promote asthma
-Increases eosinophils presence
-Increase airway remodeling (smooth muscle hypertrophy & hyperplasia; subepithelial fibrosis/stiffening of airway)
What is a response to a repeat exposure to an allergen in a pt w/ asthma?
Eosinophils will play a prominent role in the late phase of an asthma attack
What are key mediators of atopic asthma in the initial pathogenesis & promotion?
Allergen
-Causes release of inflammatory cytokines
-Causes increased production of IgE
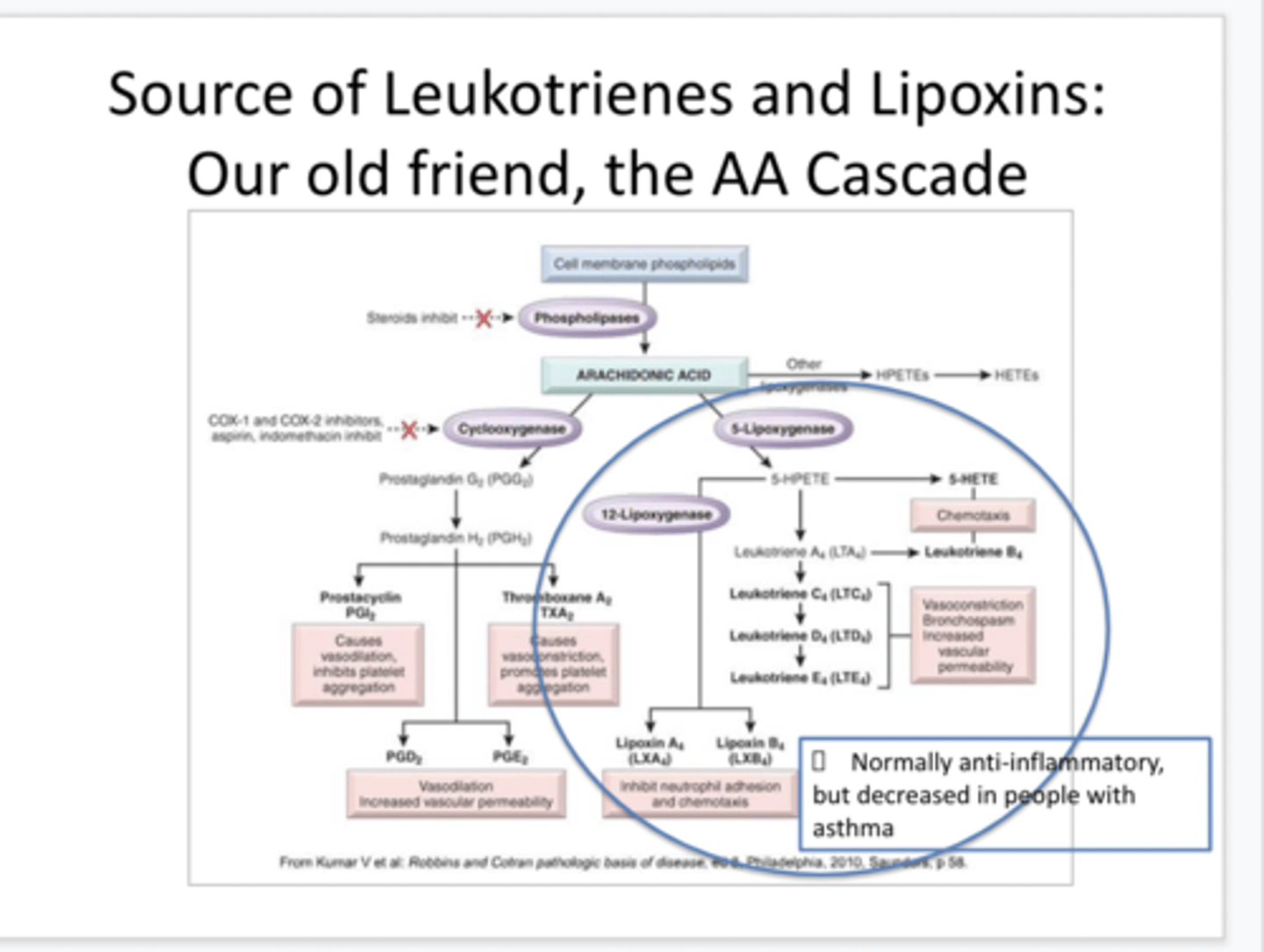
What are key mediators of atopic asthma during the early phase of bronchoconstriction, edema, mucosal thickening & secretions
-Acetylcholine (vagus n. innervation of airways): ACh is a bronchoconstrictor
-Histamine from mast cells & basophils
-> Causes bronchoconstriction, vascular permeability & leakiness (edema), increases mucus viscosity
-Leukotrienes: promote bronchoconstriction, increases vascular permeability, increases mucus secretion & eosinophil recruitment
-Lipoxins: anti-inflammatory but are decreased in asthma
-Adenosine & AMP can cause bronchoconstriction in asthma & COPD pts
What is the source of leukotrines & lipoxins
Arachidonic Acid Cascade
What are the key mediators of atopic asthma during the late phase?
-Eosinophil Chemotactic factor: released by mast cells ( & other cells); Attracts more eosinophils to the inflamed region
-Eotaxins: released by epithelial cells; Attracts eosinophils & mast cells
-Eosinophil major basic protein: releases into/onto tissues by eosinophils & can cause additional tissue damage
-ROS: released by eosinophils & cause tissue damage
-Interleukins: released by Type Typer 2 T-H cells; promote eosinophil survival & activity
-> Important example: IL-5
-Inflammatory mediators (IL-1, IL-6, TNF-α, Leukotrienes): released by eosinophils & amplify inflammatory response
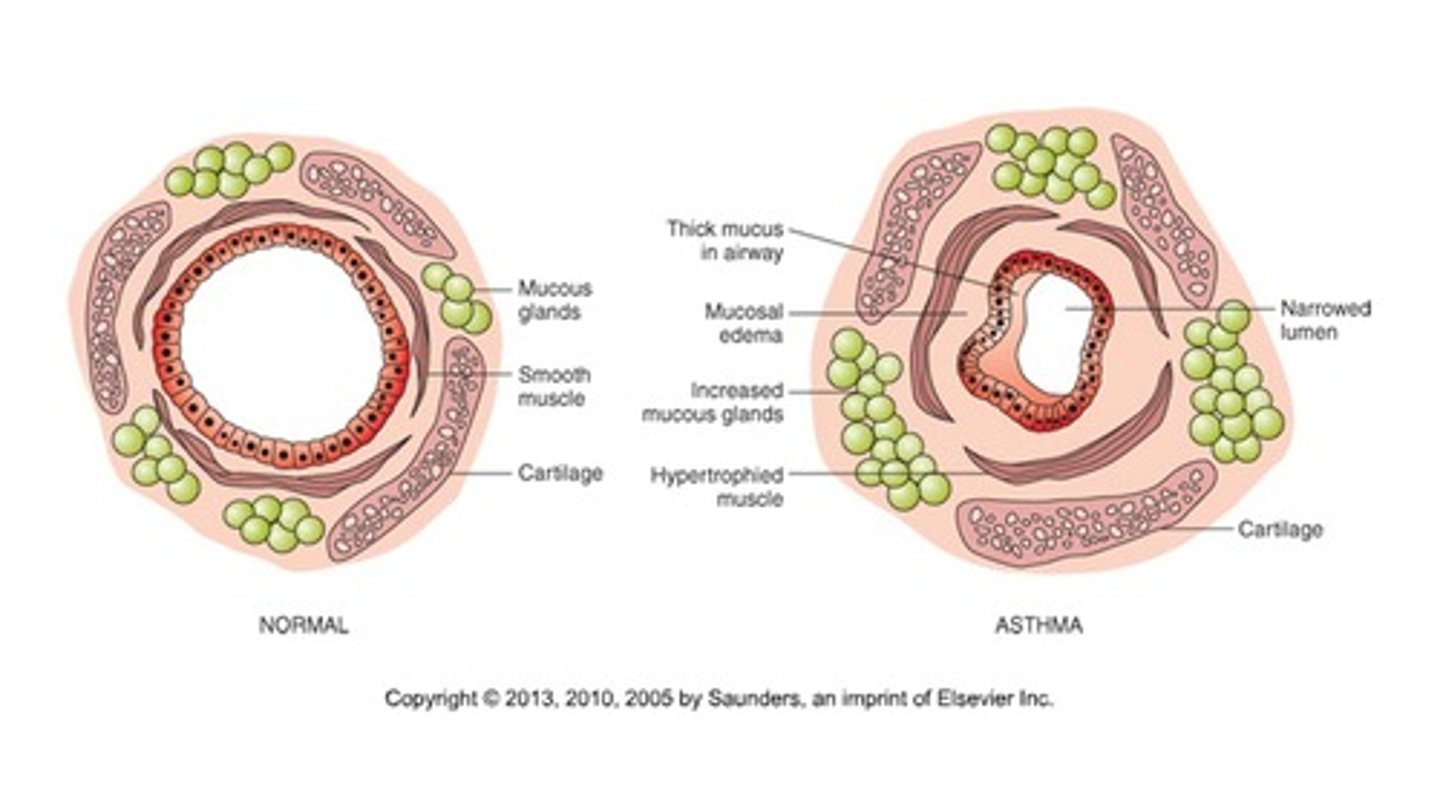
What is airway remodeling?
Persistent cellular & structural changes in the airway wall
What are changes that occur due to airway remodeling?
-Bronchial smooth muscle hypertrophy (mainly) & hyperplasia
-Goblet cell hyperplasia (mucus-producing)
->tend to hypersecrete mucus; mucus is thicker than normal
-Subendothelial mucous gland hypertrophy (mainly) & hyperplasia
-> Mucus plugs cause partial or total occlusion of lumen
-> Mucus in airway lumen
-Deposition of collagen & fibrocytes in epithelial basement membrane -> thickening & stiffening
-Loss of ciliated epithelial cells -> more exposure allergens, toxins & microbes to airway
-Increases number & size of blood vessels in bronchial tissues -> tend to be leaky -> edema of airways
What is airflow proportional to?
Airflow (F) proportional to pressure (P) gradient (from mouth -> alveoli)/airway resistance
Normally, is resistance to airflow high or low?
Normally Low which allows air to move w/ a small pressure gradient
What is the primary determinant of resistance to airflow?
Radius of airway
What can a decrease in airway radius in asthma?
-Bronchoconstriction
-Mucus production
-Inflamed/thickened airway wall
What happens to the work of breathing in asthma?
Increased work of breathing d/t increased airway resistance
Accumulation of air behind closed airways -> air trapping & lung hyperinflation
What can happen to the work of breathing in severe cases of asthma?
There is a complete closure of some airways & causes isolation of portions of the lung
-> no gas exchange can occur d/t the blocked alveoli -> hypoxemia
Is expiration or inspiration more difficult for a pt w/ asthma?
Expiration (esp. active expiration)
What happens during inspiration in a pt w/ asthma?
Negative pleural pressure (from the expanding thorax) "pulls" the airways open at the same time that it expands the alveoli
-Air will flow in easily
What happens during expiration in a pt w/ asthma?
Increase in closing tendency of the airways d/t the extra positive pressure required in the chest to cause expiration
-Since bronchioles in asthmatic lungs are already narrowed, further narrowing resulting from the external pressures will create obstruction during expiration
-> Air will tend to get trapped in the lungs
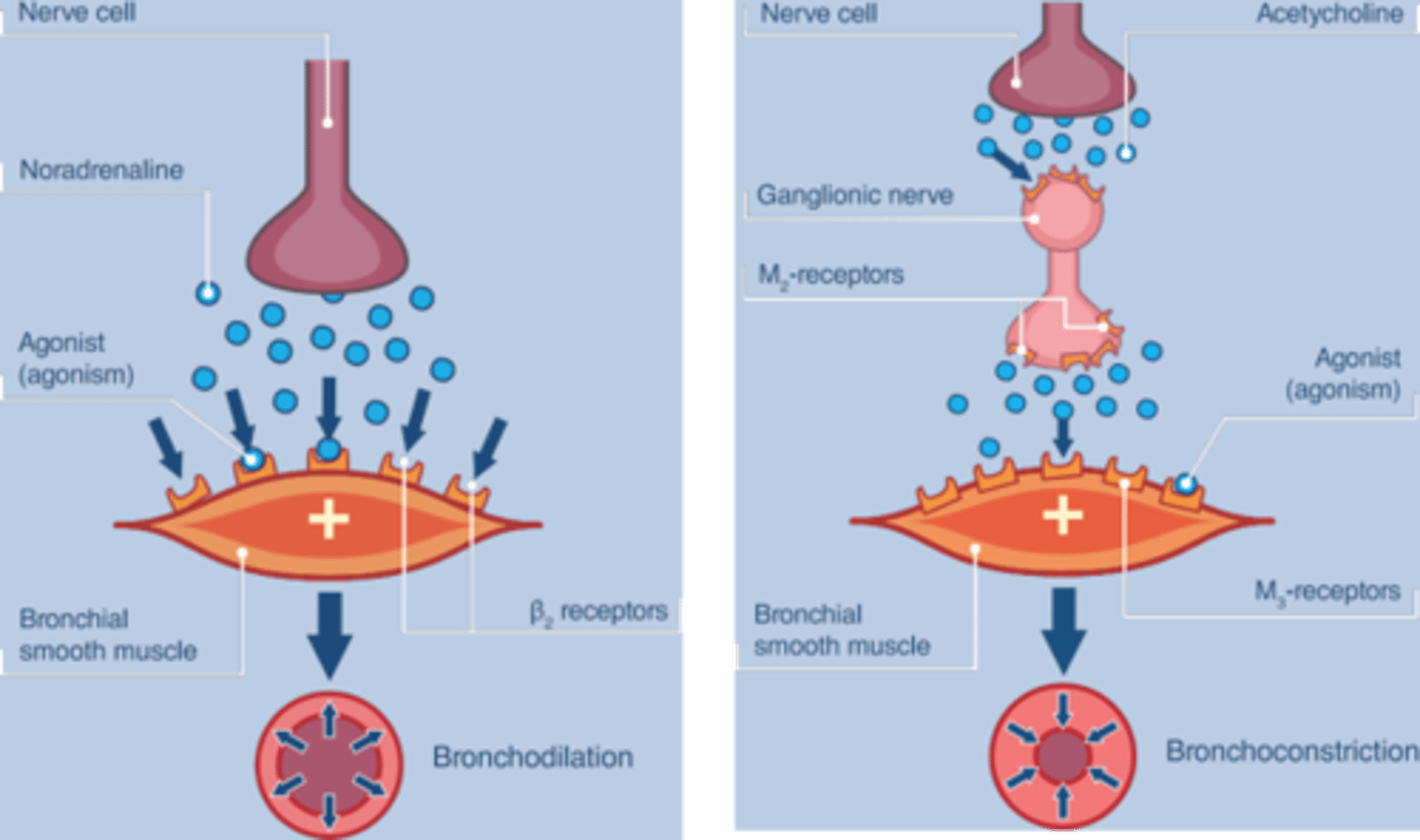
Bronchial smooth muscle tone regulation by autonomic & local influences
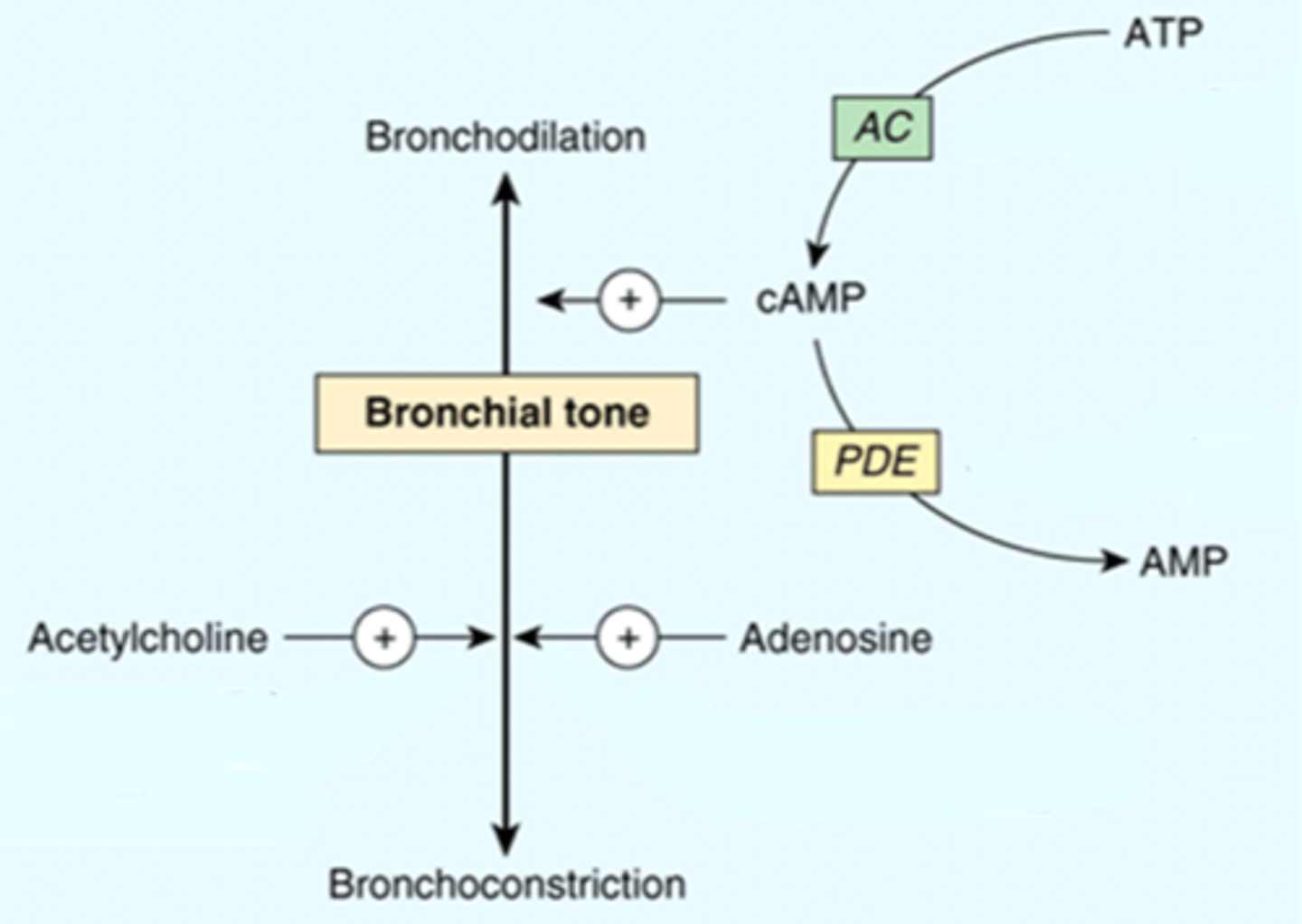
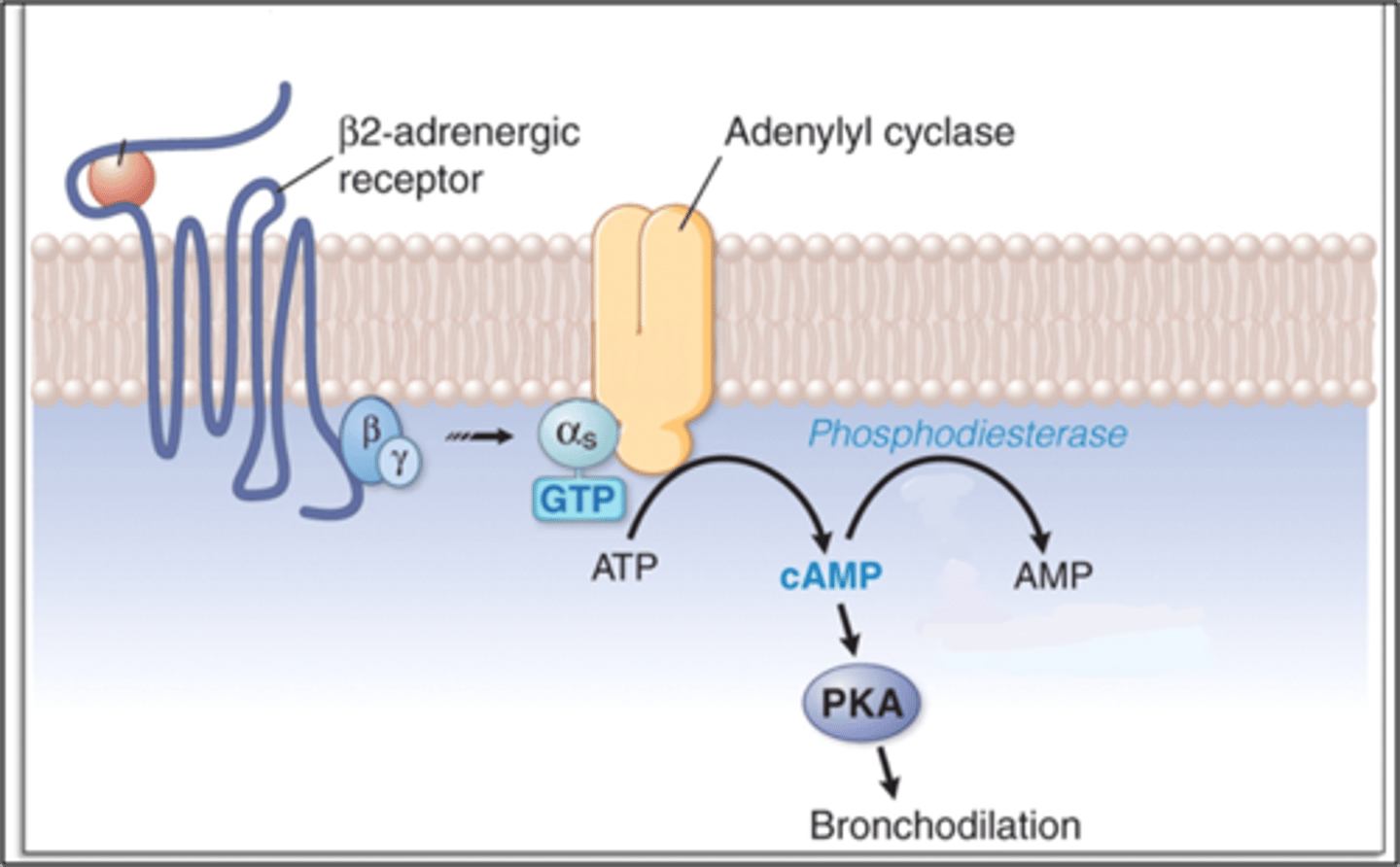
What is sympathetic regulation of bronchial smooth muscle?
β2 adrenergic receptor is activated & airway diameter increases -> bronchodilation
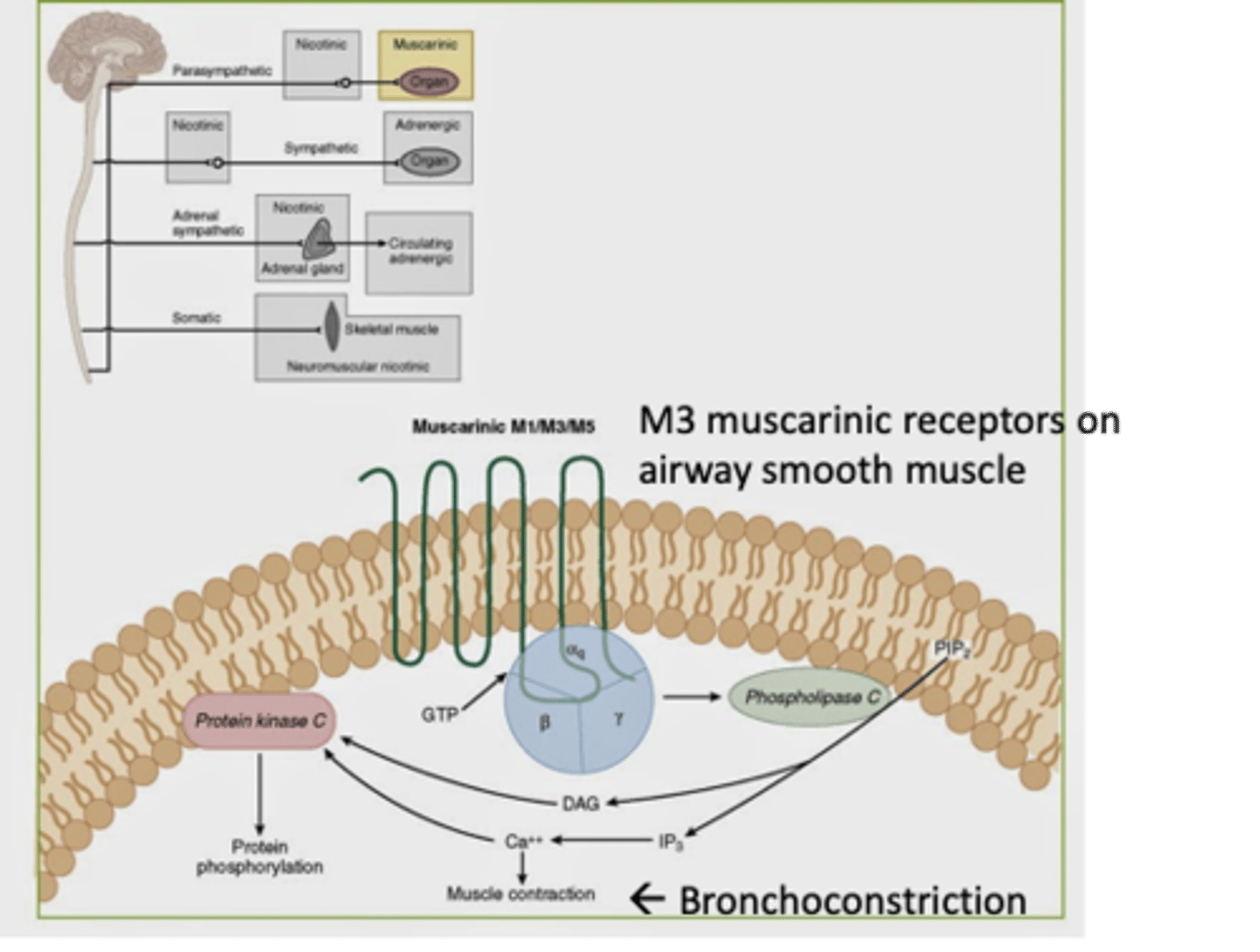
What is parasympathetic regulation of bronchial smooth muscle?
M3 muscarinic (cholinergic receptor is activated & airway diameter decreases -> bronchodilation
the activation of M3 will increase muscle contraction
Adrenergic & Muscarinic agonism
noradrenaline = norepinephrine
What is an asthma attack?
An acute worsening of asthma symptoms caused by an exposure to a trigger
What are symptoms of an asthma attack caused by?
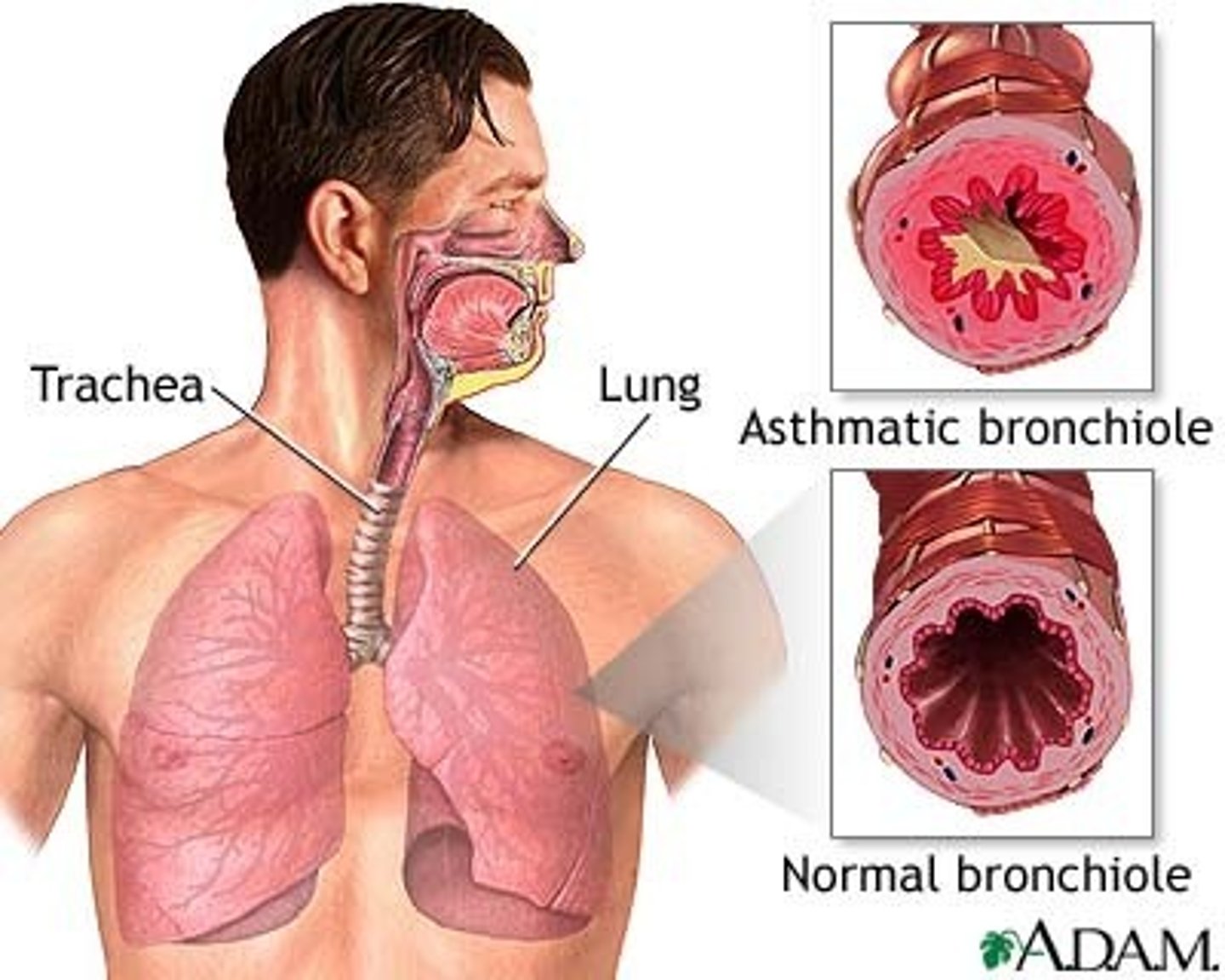
-Airway narrowing: due to bronchospasm/sudden constriction
-Edema/swelling
-Increased mucus production and/or thickening
What occurs in the early phase of an asthma attack?
-Histamine is released
-Leukotrienes
-Swelling
-Bronchoconstriction
-Excess mucus production
What occurs during the late phase of an asthma attack?
Cytokine-mediated leukocyte recruitment: eosinophils, basophils, neutrophils & monocytes
Leads to:
-Swelling
-Refractory bronchospasm
-Mucus plugging
What is important patient teaching for an asthma attack?
1. Have them recognize the sign & symptoms of an impending or worsening asthma attack
2. Use their rescue/reliever inhaler sooner than later
Goal: minimize frequency, duration & severity of asthma attacks
What is the difference between breathing in health lungs vs. during an asthma attack?
Healthy Lungs: airways are wide & amount of air is about the same as it comes in and out
During Asthma Attack:: airways are narrow & air gets trapped in the lungs
(less air expired)
What are clinical manifestations of an asthma attack?
-Coughing, wheezing (high-pitched, whistle sound) & SOB
-> more mild wheezing occurs between attacks
-Chest tightness sensation
-Anxiety, tachycardia & palpitations
-Tachypnea, cyanosis & use of respiratory muscles of respiration
-Increasing asthma severity -> increased frequency of symptoms
-Status Asthmaticus (worst outcome)
What is Status Asthmaticus?
An acute exacerbation of asthma that remains unresponsive to initial Tx w/ bronchodilators
-Can be fatal, but not always
-May only speak 1 or 2 words at a time
-Wheezing can disappear as airway constricts more & more (don't be fooled by this)
What are the 2 types of asthma severity?
-Intermittent
-Persistent: further divided into mild, moderate or severe
Sign & Symptoms of Intermittent asthma
Daytime symptoms: ≤ 2 times/week
Nighttime symptoms: ≤ 2 times/week
Use of rescue med to control symptoms: ≤ 2 times/week
Interference w/ daily activity d/t asthma: NONE
Lung function: FEV1 > 80%
Exacerbations: 0-1 per year
Signs & Symptoms of Persistent asthma
Daytime symptoms: > 2 times/week
Nighttime symptoms: > 2 times/month
Use of rescue med for symptom control: > 2 times/week
Interference w/ daily activity d/t asthma: ANY
Lung function: FEV1 ≤ 80%
Exacerbations: ≥ 2 per year
What is used for self-care and an office's measure for the assessment of asthma control?
Peak expiratory flow (peak flow)
-Measured w/ handheld peak flow meter
-Measures maximal expiration after maximal inspiration
-Used in combination w/ a written asthma action plan for the pt or caregiver to follow
What should a pt keep a daily diary of when assessing their asthma control?
Medication use, Peak flow & Symptoms
How can asthma control be assessed?
By the "Rule of 2s"
When is asthma considered well-controlled?
If the pt:
-reports symptoms ≤ 2 days/week
-use rescue inhaler ≤ 2 days/week
-awakened by symptoms ≤ 2 times/month
-reports no interference w/ daily activity from asthma & has normal PFTs between exacerbations
ALL of the above criteria must be met for asthma to be considered well-controlled
What is a Pulmonary Function Tests (PFTs)?
An indicator of function in asthma is the forced expiratory volume in 1 second (FEV1) & the ratio of FEV1 to forced vital capacity (FVC): FEV1/FVC
-Normal FEV1/FVC is also biological/birth sex, body size and ethnic group-dependent
What is Spirometer used for?
To measure lung volumes & airflow
(how fast & how much air you breath out)
What is Body Plethymography?
A more complexed test used to measure residual volume (RV), total lung capacity (TLC) & any other lung volume that incorporates RV
When looking at pulmonary function studies, what will be DECREASED in a pt w/ obstructive lung disease?
FVC & FEV1
When looking at pulmonary function studies, what will be INCREASED in a pt w/ obstructive lung disease?
RV (air trapping) & TLC (hyperinflation - more prominent in COPD pts)
What is asthma exacerbation?
-Deterioration in symptoms (may require corticosteroids)
-Decreases in airflow
-Time course: gradual
-usually a clinical diagnosis (based on pt Hx & presentation)
What is COPD?
Chronic Obstructive Pulmonary Disease
-chronic
-progressive
-heterogeneous presentation
-treatable
-inflammation plays a significant role in airway changes that lead to airflow obstruction
What are the most common respiratory symptoms seen in COPD?
Dyspnea, cough &/or sputum production
dyspnea is considered the cardinal symptom
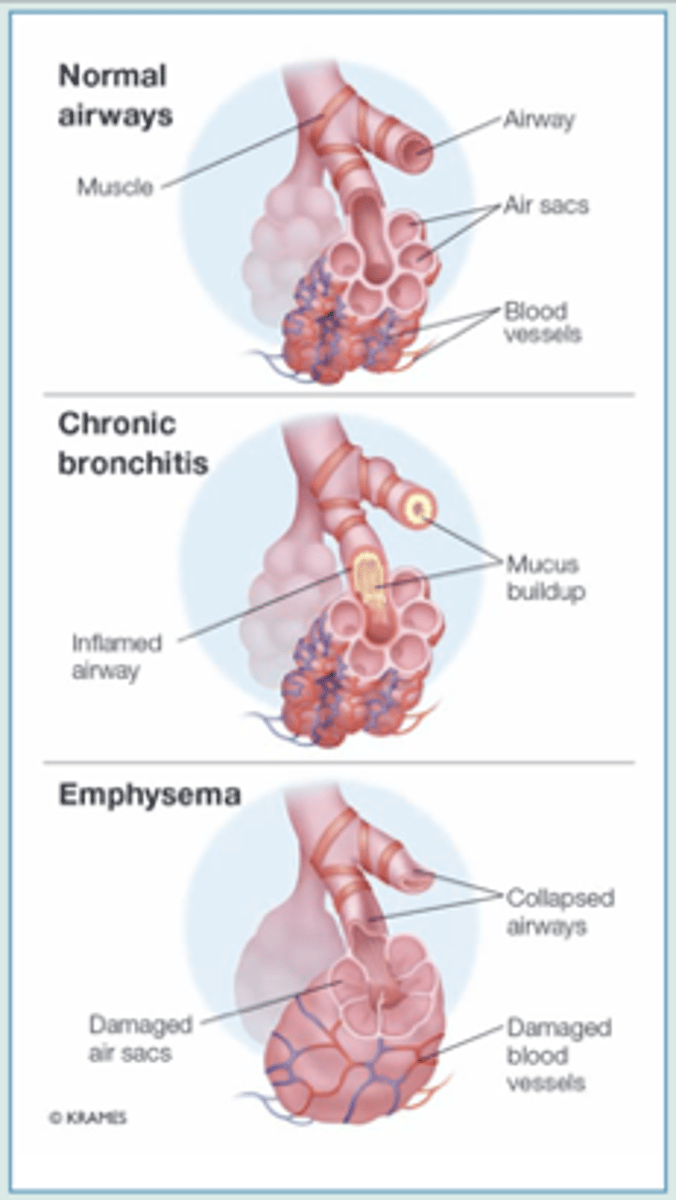
What can a pt w/ COPD have?
Chronic bronchitis, emphysema &/or other diseases of small airways (includes obstructive bronchiolitis)
What is chronic bronchitis?
Cough & sputum production for at least 3 months in at least 2 consecutive years
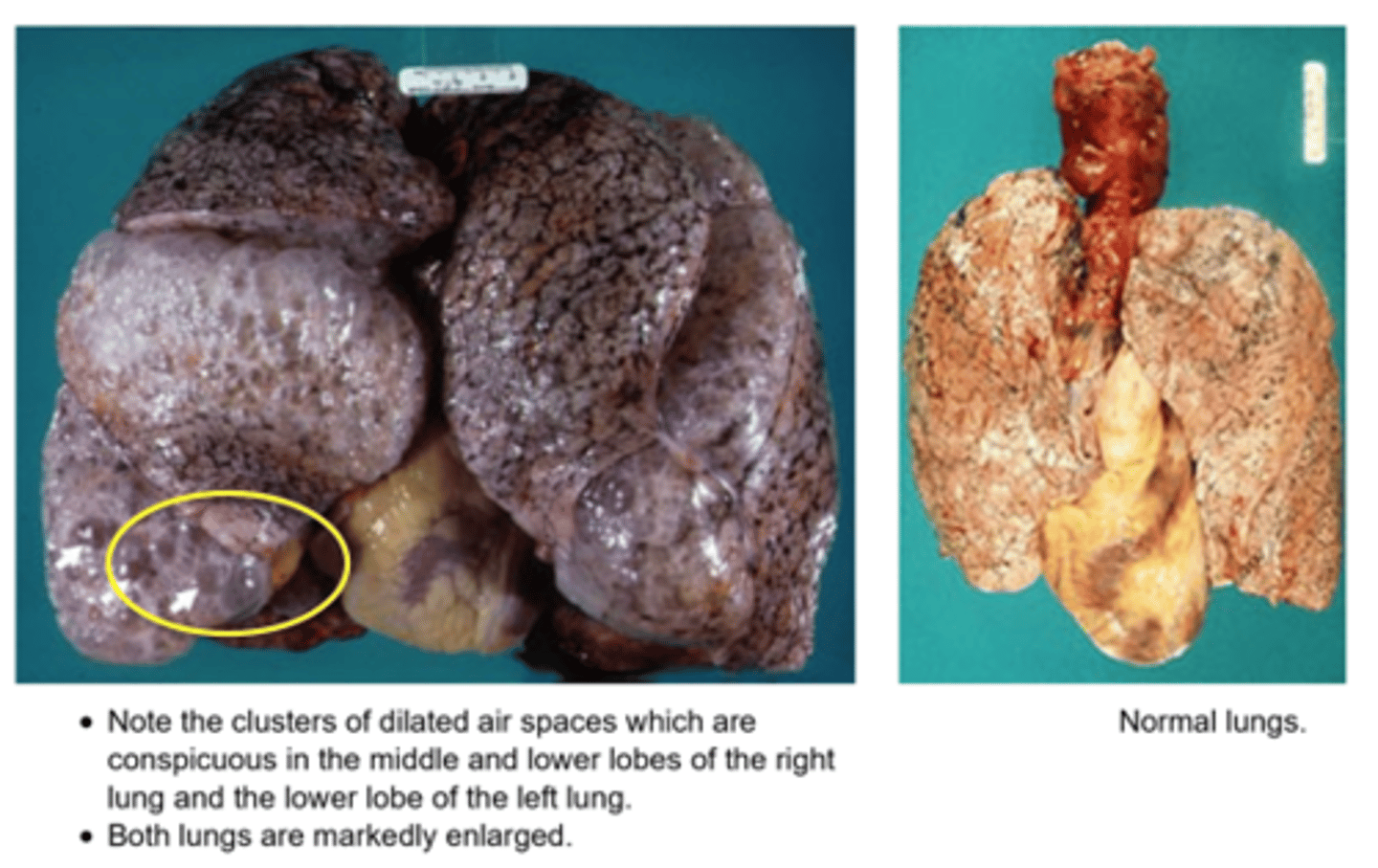
What is emphysema?
Abnormal, permanent enlargement of the air spaces distal to the terminal bronchioles
-accompanied by destruction of their walls & w/o obvious fibrosis
What is obstructive bronchiolitis?
Inflammation, narrowing or obliteration of bronchioles
What is an important point about COPD?
COPD is an umbrella term
-if a pt has emphysema, chronic bronchitis or other disorders like bronchiolitis, they have COPD
How can COPD affect a pt's quality of life?
Can limit the pt's:
Ability to work
Normal physical exertion capacity
Sleep
Ability to perform household chores
Participation w/ social or family activities
What is the primary cause of COPD?
Smoking
-accounts for 75% of COPD risk
-BUT about 25% of pts w/ COPD have never smoked
Which sex has a higher risk of COPD?
Females have greater risk/rate of COPD than men throughout most of their lifespan
-Most vulnerable before 65 yrs old
Why do females have higher rates of COPD?
-Have smaller lungs -> higher concentration of cigarette toxins in lungs
-The role of estrogen in metabolism & inhibition of excretion of toxins
-Females are 1.5x > likely than to males to never smoke, but still develop COPD
Transgender man/AFAB pt will have smaller lungs. PFTs must be interpreted carefully
What is the function of Alpha-1 Antitrypsin and where is it synthesized?
Synthesized: in the liver
Function: Inhibits proteolytic breakdown of alveolar tissue
-esp. by inhibiting neutrophil elastase thats produced by the pulmonary neutrophils in the presence of infection, inflammation or smoking (elastase is capable of breaking down elastin in alveolar walls)
-Macrophages can also produce proteases (which can be damaging)
What happens if there is a deficiency of AAT or the liver cannot produce it?
The neutrophils elastase & macrophage proteases can function unchecked -> destructs alveolar walls & emphysema develops
AAT deficiency is a genetic disease that creates a risk factor for COPD & liver disease
What happens to mucus in chronic bronchitis? What goes thorugh hyperplasai and hypertrophy?
Increases in mucus production 2/2
-Hyperplasia primarily of goblet cells
-Hypertrophy primarily of bronchial mucous glands
Mucus becomes thicker & more tenacious -> plugging of airway
What causes chronic infection in chronic bronchitis?
Bacteria that has become embedded in the airway secretions
What happens to cilia in chronic bronchitis?
Ciliary function is impaired -. Decreased mucociliary clearance
-fewer cilia & the remaining cilia is less able to function
What causes narrowing of airways in chronic bronchitis?
Edema & accumulation of inflammatory cells -> bronchial wall inflammation & thickening -> narrow airway lumen
What happens in chronic bronchitis pertaining to airway obstruction?
-Diffuse airway obstruction occurs
-Initially affects only larger bronchi (eventually involves all airways, alveoli)
-Airway wall enlarges, loss of elastic recoil in the alveoli trap air (limits outflow)
-Obstructed airways are likely to close on expiration
-Traps air in the distal portions of the lungs
What does trapping air in the distal portions of the lungs cause?
-Hypoventilation (-> hypercapnia)
-Hypoxemia
How does smoking lead to emphysema?
Smoking -> inflammation -> recruitment & activation of neutrophils, macrophages
Also, Alpha-1 antitrypsin is inactivated smoking (even in the absence of genetic AAT deficiency)
-> So, AAT cannot perform its normal function of inhibiting the breakdown of alveolar tissue
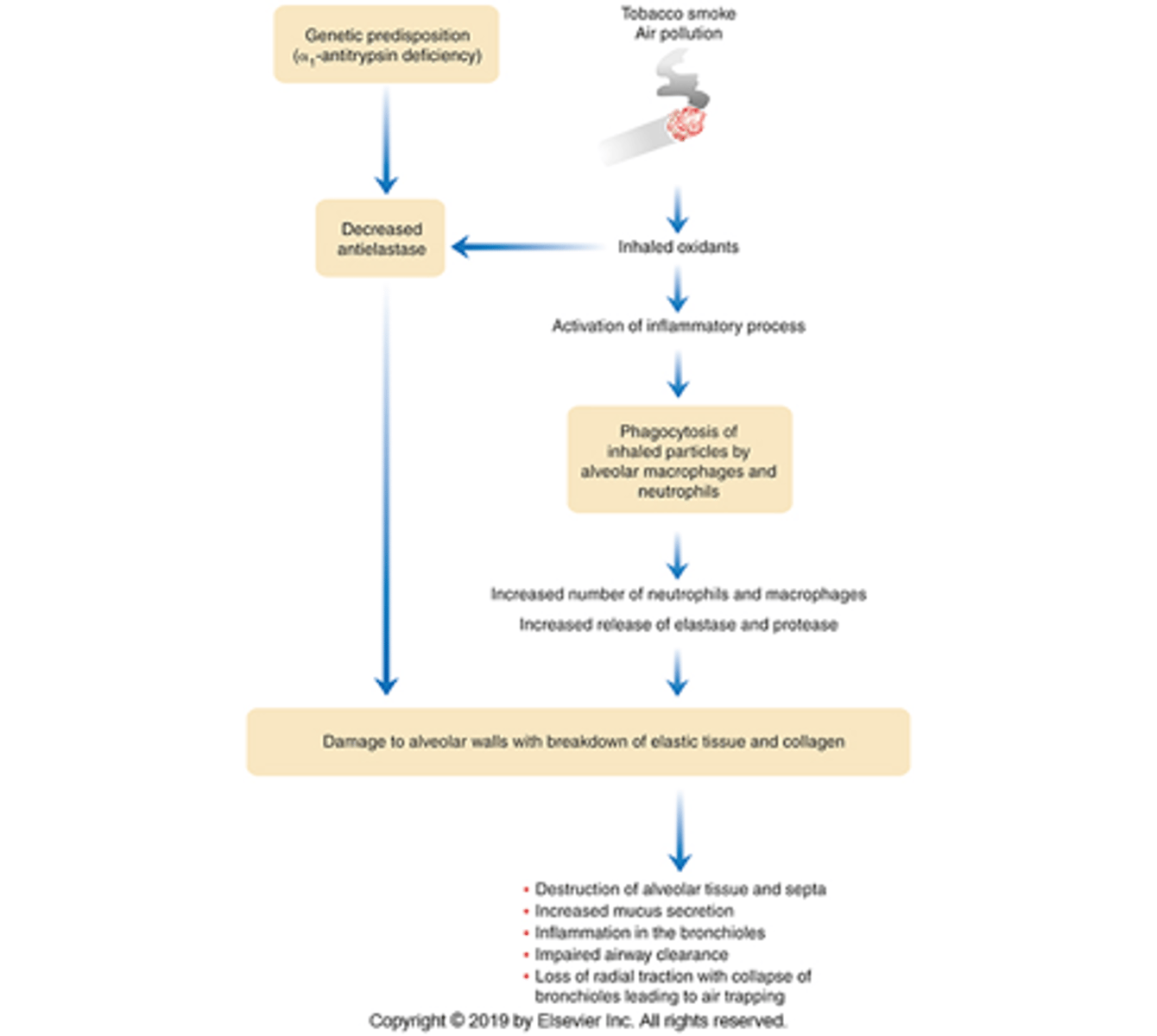
What released by the neutrophils & macrophages and what do they do during emphysema?
Elastase & other proteases are released by neutrophils, macrophages
Will cause alveolar wall destruction & breakdown of elastic tissue
-> alveoli become untethered from small airways & lose their normal elastic recoil
What is the result of emphysema?
Narrowing & collapse of small airways
Reduction of pulmonary capillary bed (which is necessary for gas exchange)
Alveolar enlargement + loss of elastic recoil = trap air & causes lung hyperinflation
What happens to airway resistance in emphysema?
Its increased d/t compromised alveolar walls that surround bronchioles -> airway lumen narrowed
When are airways likely to close during emphysema?
Likely to close on expiration
-In severe disease, normal quiet expiration becomes difficult
In emphysema, what becomes enlarged?
Lungs & alveoli
Can a pt have both chronic bronchitis & emphysema?
Yes, in severe cases
-But one type usually dominates