PHYSIOLOGY RESPIRATION
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
Respiration
The biologic process of oxygen and carbon dioxide exchanging across permeable membranes
External Respiration
Gas exchange between the environment and the pulmonary capillary blood.
Internal Respiration
Gas exchange between the blood and other tissues, and O2 use by tissues
Cellular Respiration
The process by which the chemical energy of "food" molecules is released and partially captured in the form of ATP.
Ventilation
v is defined as the process that moves gases between the external environment and the alveoli
v Is the process of moving gas (usually air) in and out of the lungs.
Gas exchange
occurs between air and blood in the lungs and between the blood and body tissues, it is the exchange of O2 and CO2
Respiratory Exchange Rate
The quantity of oxygen and carbon dioxide exchanged during a period of 1 minute
Respiratory Quotient
the ratio between the volume of oxygen consumed (V∙O2) and the volume of carbon dioxide produced (V∙CO2)
200mL
carbon dioxide produced by a normal person
250mL
Oxygen consumed by a normal person
0.8
Normal Respiratory Quotient
4 L/min
Normal Alveolar ventilation
4:5, or 0.8
Normal Ventilation-Perfusion and ratio
Zone 1
Zone with Least gravity dependent area, Alveolar pressures are higher than the pulmonary arterial pressures
Zone 2
Zone with Area of complex and varying intermittent blood flow
Zone 3
Zone Gravity dependent and has a lot of blood flow
Deadspace unit
alveolus is normally ventilated but there is no blood flow through the capillary.
Shunt Unit
alveolus is completely unventilated, whereas the adjacent capillary has blood flow V=0 Q = 1
Silent Shunt Unit
Alveolus is unventilated and the capillary has no perfusion
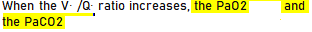
Increased V/Q ratio
An increased in ventilation and a decrease in perfusion
Rises, Falls
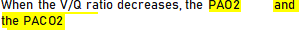
Decreased V/Q ratio
A decrease in ventilation and an increase in perfusion
V/Q ratio
ratio of ventilation to blood flow 4:5, or 0.8, this relationship is called the
Falls, Rises
Intrapleural Pressure
is the pressure in the potential space between the parietal and visceral pleurae
-5cm
Intraplueral Pressure during expiration in a normal individual
-10cm
Intraplueral Pressure during end of inspiration in a normal individual
Transpulmonary Pressure
It is the difference between the alveolar pressure (Palv) and the pleural pressure (Ppl)
40 Torr
In the healthy resting individual, venous blood entering the alveolarcapillary system has an average OXYGEN TENSION (PV–O2) of
46 torr
In the healthy resting individual, venous blood entering the alveolarcapillary system has an average CARBON DIOXIDE tension (PV–O2) of
A-a gradient
the difference between the alveolar oxygen pressure and arterial blood oxygen saturation
5-20
Normal A-a gradient
Oxygenation failure
Increased A-a gradient indicates what?
Ventilation failure
Decreased A-a gradient indicates what
Fick’s law
states that the diffusion flux (rate of movement per area) is proportional to the negative of the concentration gradient
Alveolar Ventilation
v portion of the ventilation that undergoes gas exchange (respire)
v volume of air entering and leaving the alveoli per minute
Deadspace Ventilation
v portion of the ventilation that does not undergo gas exchange (does not respire)
v This physiologically ineffective portion of ventilation requires energy expenditure for its movement into and out of the lungs but provides no respiratory benefit.
Anatomical Deadspace
comprises the gas volume that occupies the pulmonary conducting system; it does not contribute to gas exchange
Physiologic Deadspace
Both anatomical and alveolar deadspace
Alveolar Perfusion
The alveolar PCO2 essentially results from the dynamic equilibrium between CO2 molecules entering the alveolus from the blood and CO2 molecules leaving the alveolus in the exhaled gas
Transairway Pressure
Is the difference between the barometric (atmospheric) pressure (PB) and the alveolar pressure (Palv)
Transmural Pressure
v It is the pressure difference that occurs across the airway wall. The __pressure is calculated by subtracting the intraairway pressure (Piaw) from the pressure on the outside of the airway (Poaw).
Transthoracic Pressure
v is the difference between the alveolar pressure (Palv) and the body surface pressure (Pbs).
v It represents the pressure required to expand or contract the lungs and the chest wall at the same time
v PW=Palv-Pbs
Electron Transport Chain
is a cluster of proteins that transfer electrons through a membrane within mitochondria to form a gradient of protons that drives the creation of adenosine triphosphate (ATP)
Glycolysis
v The first pathway used in the breakdown of glucose to extract energy.
v It takes place in the cytoplasm
v Glucose is converted into a more usable form called pyruvate
Transition Reaction
v converts pyruvate into acetyl CoA (acetyl coenzyme A ) producing Co2 and NADH
Krebs cycle
v eries of reaction that takes acetyl CoA and produces NADH, FADH and ATP
v The Krebs cycle is an aerobic process, meaning it requires oxygen to work, so the Krebs cycle gets to business right away mixing carbon and oxygen in the respiration pathway