McGill PSYC 100 Lectures 22-24: Clinical Psychology
1/130
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
131 Terms
Psychological disorder
A disturbance in an individual's emotional regulation, cognition, or behaviour that is clinically significant,
i.e. usually associated with significant distress or disability in social, occupational, and other important activities.
Symptom
A deviation from norms in emotions, thoughts or behavior (norms can be personal or societal)
Point prevalence
The percentage of people in a given population who have a given disorder at any particular point in time.
12-month prevalence
the percentage of a population affected by a condition over a one-year period
Lifetime prevalence
The percentage of people in a certain population who will have a given disorder at any point in their lives.
Incidence
The number or rate of new cases of a particular condition during a specific time.
Diagnostic and Statistical Manual of Mental Disorders (DSM)
major classification scheme used in Canada and the United States.
Advantages of Diagnostic Labels
• Improves research
• Can improve the identification of effective treatments
• Can reduce confusion for individuals struggling with symptoms
• Allows access to treatment
• Allows access to workplace/school accommodations
• Can facilitate advocacy
Disadvantages of Diagnostic Labels
• Emphasizes distinctions between disorders
• Can slow research progress and be isolating for affected individuals
• Can foster the notion that psychological disorders are fixed and enduring
• Can cause stigma
• Can be associated with self-stigma
• Makes it difficult to get help for subsyndromal (milder, less frequent, or shorter in duration) conditions
"Cause" in Mental Illness
An agent, event, condition or characteristic that plays an essential role in producing the illness.
Examples:
• Huntington's Disease (autosomal dominant gene)
• Wernicke-Korsakoff syndrome (lack of thiamine)
• Neurosyphilis Dementia (spirochete gets into CNS)
No known cause for the majority of mental illnesses, only contributing factors.
Diathesis-stress model
A model of clinical disorders where the expression of the disorder occurs when an underlying vulnerability interacts with an environmental stressor.
diathesis -> stress -> psychological disorder
Bucket Analogy
Diathesis: the size of the bucket
Water: Environmental Stressors
Taps: Healthy Strategies for Managing Stress
Diathesis (Zubin and Spring, 1978)
"Genetic Inheritance and Acquired Propensities"
-DNA from your parents
-Prenatal or Perinatal Brain Injury
-Childhood Experiences, Cognitive Attributional Style, Personality, etc.
Stress (Zubin and Spring, 1978)
Endogenous/biological or exogenous/life event stress
-Drug use
-Infection, Hormonal Changes etc.
-New Job/City/Role, Relationship Loss, Financial Stress, Illness
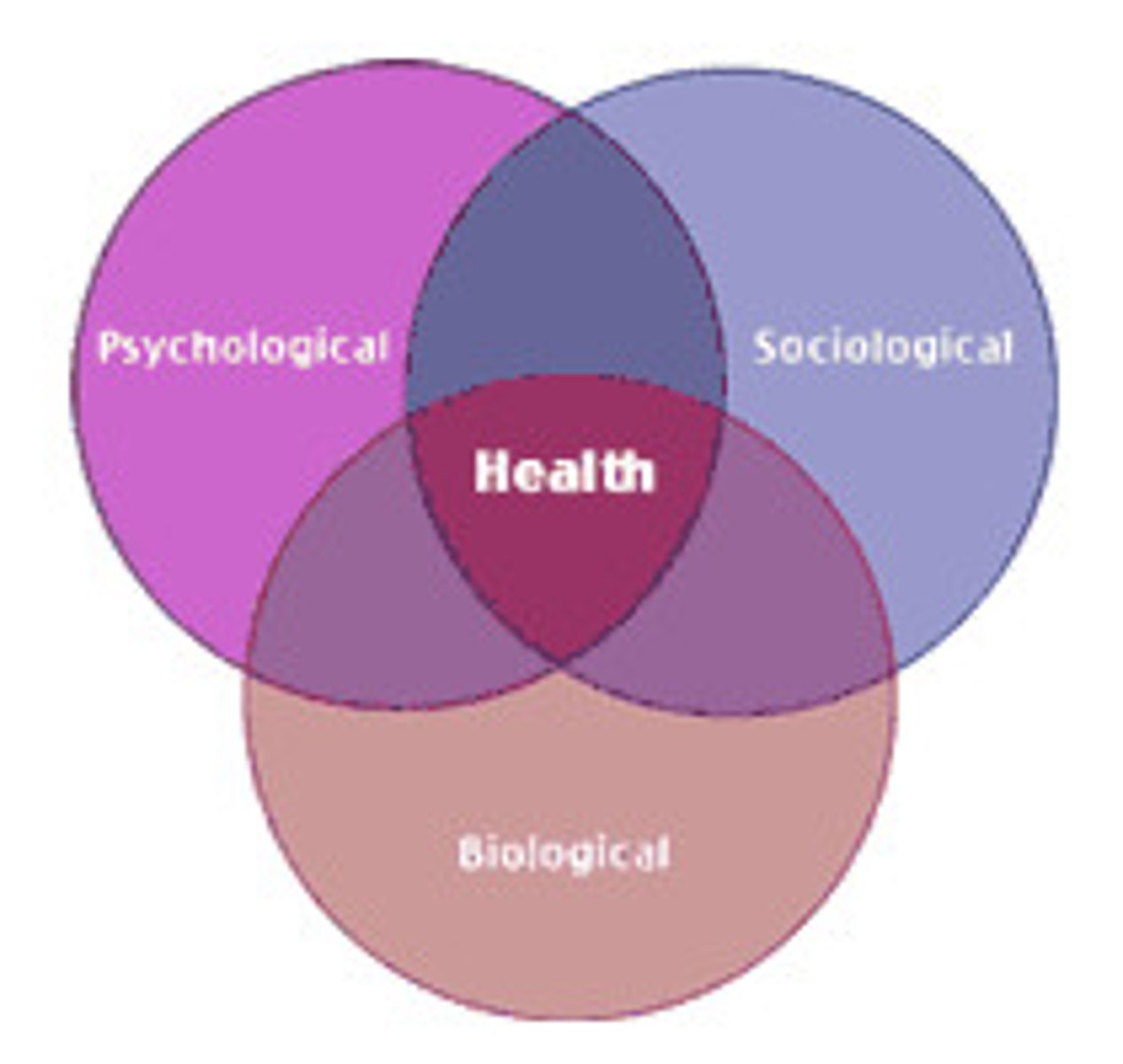
Biopsychosocial Model
biological, psychological, and social factors combine to influence mental health outcomes.
-Within the Diathesis-Stress Model of Psychological Disorders
-Each domain influences the other.
-There is no biological primacy
Major Depressive Disorder
A mood disorder in which a person experiences two or more weeks of significantly depressed moods, feelings of worthlessness, and diminished interest or pleasure in most activities.
2 Criterial Symptoms of Major Depressive Disorder
- Depressed Mood
- Anhedonia
Anhedonia
Diminished interest or pleasure in nearly all of the activities that usually bring pleasure (e.g. eating, exercising, spending time with friends etc.)
Depressed Mood
enduring period of sadness
depersonalization
feeling detached from one's body, sense of watching yourself from the outside
-can be a symptom of Major Depressive Disorder if it is present for most of the day, more days than not, for at least 2 weeks
rumination
preoccupation with depressive thoughts
-can be a symptom of Major Depressive Disorder if it is present for most of the day, more days than not, for at least 2 weeks
Prevalence of Major Depressive Disorder
In Canada:
- ~7 % pre-COVID pandemic, 16 % in fall 2020.
- Females more frequently affected
- Frequently co-morbid with other disorders, including anxiety disorders, psychotic disorders, substance use disorders and eating disorders
- Can present with psychotic symptoms (~18%) such as delusions and voices
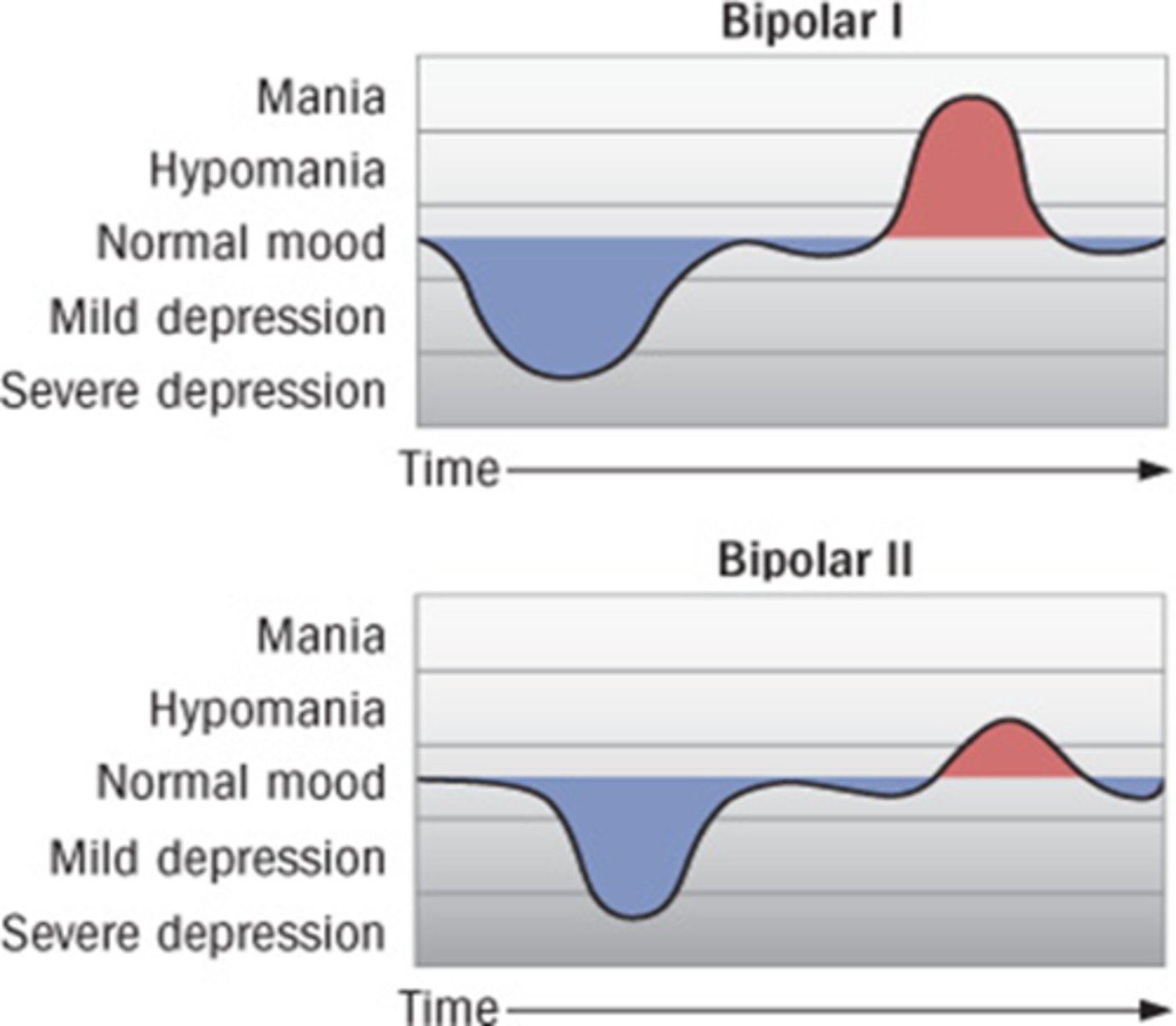
Bipolar Disorder
severe mood swings between major depressive episodes and manic episodes
-Diagnosis does NOT require a depressive episode
Bipolar 1
at least one manic episode
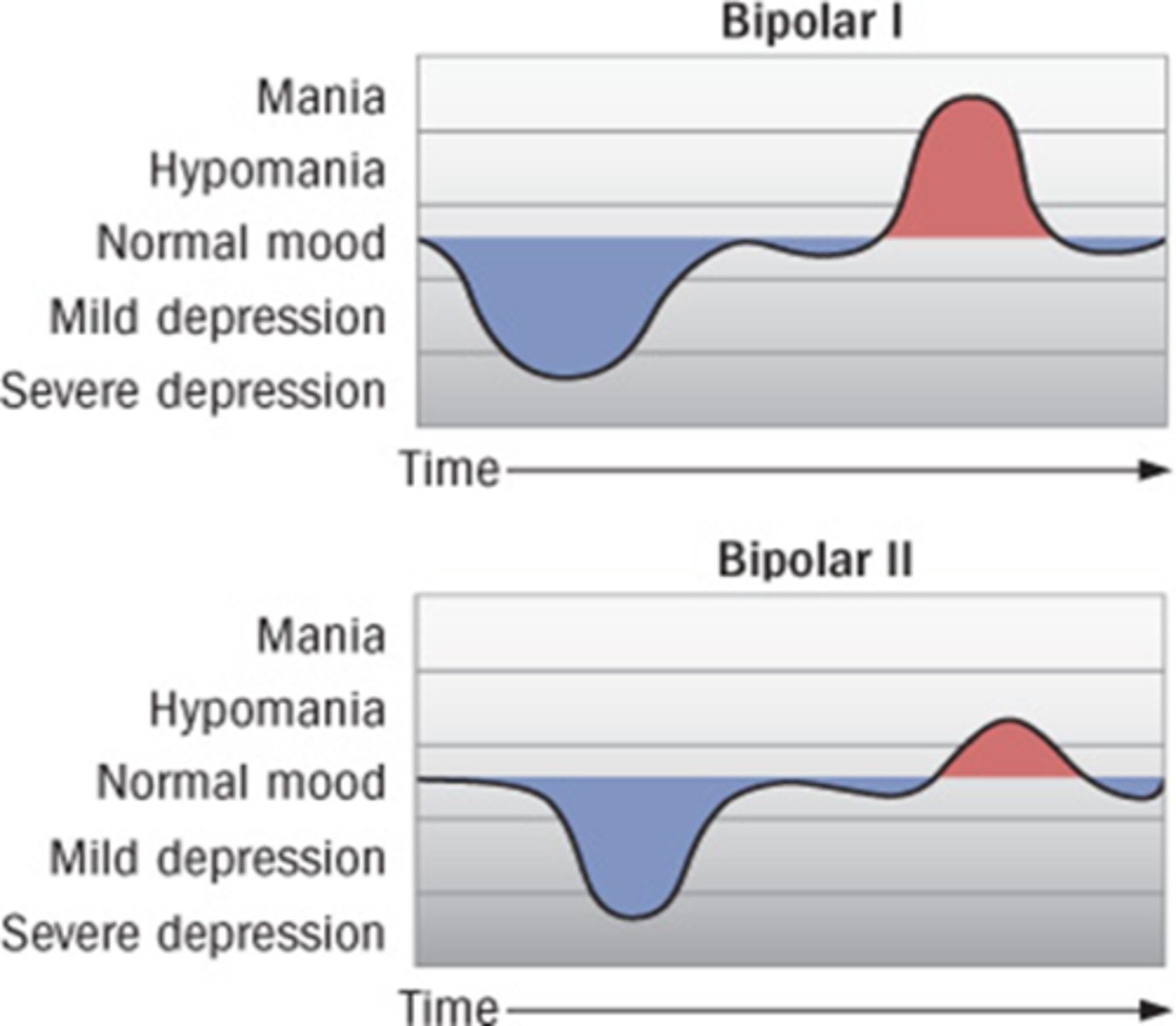
Bipolar 2
alternating periods of extremely depressed and mildly elevated moods (at least one hypomanic episode plus depressive episodes)
Criterial manic symptoms of Bipolar Disorder
• feeling like one has extraordinary powers
• needing much less sleep, feeling energetic or never tired
• racing thoughts and pressured speech
• impulsive, risky behaviour
• excessive spending
• hypersexuality
Contributing Causes of Mood-Related Disorders
-Cognitive
-Social
-Biological
Cognitive Causes of Mood-Related Disorders
-Negative cognitive schema
-Explanatory style
Negative cognitive schema
A mental framework in which a person consistently interprets events negatively.
Explanatory style
How a person explains why bad things happen to them. Higher risk of depression when explanatory style is :
• internal
• global
• stable
Social Causes of Mood-Related Disorders
• Early parental loss
• Depressed mother/caregiver
• Childhood maltreatment
• Low income
• Racism, discrimination
• Chronic illness
• Recent stressful life events
Biological Causes of Mood-Related Disorders
• Genes (~30% of variance for depression; 60-85 % for Bipolar)
• Hormonal Changes (e.g. Postpartum depression (PPD): 13% of women post childbirth)
• Sleep Deprivation and Sleep Cycle Disruption
• Substance use
• Substance use withdrawal
Schizophrenia
a group of severe disorders characterized by disorganized and delusional thinking, disturbed perceptions, and inappropriate emotions and actions
-Diagnosis requires at least 2 symptoms, at least one Positive
"Positive" symptoms
Presence of behaviours that are not present inhealthy people.
"Negative" symptoms
An absence of behaviours seen in healthy people.
Positive symptoms of schizophrenia
Delusions, Hallucinations, Disorganized Behaviour
Delusions
False beliefs rigidly maintained despite overwhelming contradictory evidence; not accepted by one's culture or subculture
-Grandiosity: Believing one has incredible powers (e.g. controlling the weather).
-Persecution: Believing one is being stalked, or singled out for punishment, often by gov't agencies
-Delusions of reference: Receiving personal messages from neutral events like newscasts, street signs, etc.
-Thought-broadcasting: thoughts are broadcast out loud
(positive symptom of schizophrenia)
Hallucinations
Sensory experiences, such as sights and sounds, that happen in the absence of any true sensory input.
• Auditory hallucinations (e.g. in the form of voices, frequently critical)
• Tactile hallucinations (e.g. feeling someone's hands on your body)
• Visual hallucinations (e.g. seeing numbers or writing, people or ghostly figures etc.)
• Olfactory hallucinations (e.g. smelling decay,dead bodies, rotting)
• Gustatory (e.g. taste metallic or like poison)
(positive symptom of schizophrenia)
Disorganized Behaviour
Unusual actions not usually seen in healthy individuals.
-Incoherent speech
-Public agitation
-Laughing at inappropriate times or childlike silliness
-Inappropriate sexual behaviour
(positive symptom of schizophrenia)
negative symptoms of schizophrenia
-Affective Flattening
-Motor Slowing and Catatonic Behaviour
-Anhedonia
-Social Withdrawal
Affective Flattening
reduced outward expression of emotion, unresponsiveness
(negative symptom of schizophrenia)
Motor Slowing and Catatonic Behaviour
moving slowly, moving little,or sitting "frozen" for hours, sometimes in unusual postures.
(negative symptom of schizophrenia)
Genetic Contributing Causes of Schizophrenia
• Risk increases as a function of genetic relatedness to an affected individual
• Concordance rates are almost 3x higher for monozygotic twins than dizygotic twins.
• Advanced paternal age (presumed to relate to genetics)
• Specific genes implicated are of small effect (no major genes has been ID'ed)
Environmental Contributing Causes of Schizophrenia
-Prenatal/Perinatal Complications; maternal illness during pregnancy, birth complications
-Living Environment Risk Factors: urban living, migration (as minority)
-Neurodevelopmental Risk Factors: delayed motor milestones, attentional deficits
-Behavioural Risk Factors: marijuana use
Dopamine Hypothesis of Schizophrenia
Reduced frontal dopamine activity is associated with negative symptoms, while excessive subcortical dopamine release is linked to positive symptoms.
-All effective antipsychotics block the D2 dopamine receptor
-Drugs that increase synaptic levels of dopamine (e.g. amphetamine, cocaine) can cause psychotic episodes
-Synaptic dopamine levels are higher in acutely psychotic patients than remitted patients
Dopamine (DA) Hypothesis: Positive and Negative Symptoms
- People with schizophrenia have reduced frontal DA activity (associated with negative symptoms)
-Reduced frontal inhibition of subcortical DA allow excessive dopamine release in response to stress (associated with positive symptoms)
Demographic Risk Factors of Suicide
• Males more likely to die by suicide (3x higher than women)
• Suicide rates are 2-3x higher in LGBTQ+
Clinical Risk Factors of Suicide
• Any mental disorder
• History of self-harm or suicide attempt
Life Stress Risk Factors of Suicide
• Relationship conflict or legal problems in last month
• Social isolation
Psychological disorders at highest risk for suicide
-Major Depression
-Borderline PD
-Bipolar Disorder
-Schizophrenia
-Alcohol/substance use disorder
Factors of Suicide Attempts
• childhood abuse and maltreatment
• sexual assault
• gender and sexual minority status
• parental suicide
• homelessness and incarceration
• intimate partner violence
Suicide in Indigenous Populations
• Inuit have among the highest risk of suicide death in the world (9x as high as the general population)
• First Nations have suicide rates 3x as high as general population
Contributing factors:
• generational trauma and substance abuse rates
• high poverty levels
• poor access to health services
• lack of culturally informed mental health care
• social stigmatization
Effective Approaches to Reducing Suicide Rates
• Educating primary care physicians to screen for and treat depression
• High school mental health and suicide education
• Decrease availability of suicidal means: (gun access, bridge access)
• Depression treatment with Cognitive-behavior therapy or antidepressants
• Clinician follow-up with phone and text after discharge/ER visit.
• Access to 24-hour support
Medical Assistance in Death (MAID)
legal health service where eligible individuals with grievous and irremediable medical conditions can receive help from a doctor or nurse practitioner to end their lives under strict laws, ensuring it's a voluntary choice with safeguards against suffering and focusing on intolerable suffering not relieved by other means.
-Extends to mental illness in 2027
Specific phobia
A marked fear of or anxiety about a particular object or situation.
• May have significant impact on the life of a person when they develop elaborate strategies to avoid the phobic object
• The lifetime prevalence of any kind of phobia is 10% in Canada.
• Women are twice as likely as men to have a specific phobia.
Social anxiety disorder (social phobia)
Extreme fear of being watched, evaluated, and judged by others.
• Typically emerges in childhood or adolescence and places a person at increased risk for depression and substance abuse.
• Fear of being evaluated and being embarrassed
• Fear of being unable to perform
• Fear of physical symptoms (blushing, heart racing, sweating)
Panic Disorder
An anxiety disorder characterized by the occurrence of unexpected panic attacks.
Panic attack
A sudden episode of uncontrollable anxiety, accompanied by laboured breathing, choking, dizziness, tingling hands and feet, sweating, trembling, heart palpitations, and/or chest pain.
Agoraphobia
A fear of being in situations in which help might not be available or escape might be difficult or embarrassing.
• Tendency to not venture outside of designated "safe" places
Generalized Anxiety Disorder
Excessive, pervasive, difficult-to-control anxiety, occurring more days than not, for 6 months or more
• More common in women
• Frequently co-morbid with depression (70%)
Cognitive symptoms of Generalized Anxiety Disorder
Feelings of inadequacy and fear, difficulty concentrating and decision making
Bodily symptoms of Generalized Anxiety Disorder
Muscle tension, fatigue, jumpiness, elevated heart rate, weakness, sweating, insomnia
Risk Factors for Anxiety-Related Disorders
• low self-esteem
• family history of Major Depression
• female gender
• years of education before age 21
• childhood sexual abuse
• white race
• traumatic events before age 21
Obsessive-Compulsive Disorder (OCD)
An anxiety disorder characterized by unwanted repetitive thoughts (obsession) and/ or actions (compulsions).
-Lifetime prevalence: ~4% (3% 12-month, i.e. persistent)
Obsession
A recurrent unwanted or disturbing thought.
Compulsion
A ritualistic action performed to control an obsession.
trauma and stressor related disorders
triggered by an event that involves actual or threatened death, serious injury, or sexual assault.
Symptoms of trauma and stressor related disorders
• Dissociation (numbness)
• Intrusive symptoms (recurrent nightmares and waking flashbacks)
• Arousal symptoms (e.g. exaggerated startle reflex)
• Avoidance symptoms (avoiding thoughts, activities, people, and places that relate to the trauma)
• Negative alterations in cognition and mood (anger, loss of pleasure, survivor's guilt)
Acute stress disorder
Trauma-related disorder , with the symptoms of PTSD, that differs in duration (3 days to <1 month).
Posttraumatic stress disorder (PTSD)
A trauma-related disorder that lasts one month or longer.
Attention-Deficit/Hyperactivity Disorder (ADHD)
a psychological disorder marked by extreme inattention and/or hyperactivity and impulsivity
-Symptoms must occur in 2+ settings, and be clinically significant
Examples of Inattention
Difficulty organizing tasks, loses things, distractible, misses deadlines, fails to follow instructions, daydreams, avoids tasks requiring sustained mental effort
Examples of Hyperactivity/Impulsivity
Fidgeting, getting out of seat in class, "driven by a motor," has trouble waiting turn,excessive talking, interrupting, intrudes on others
Inattentive ADHD
Difficulty paying attention in the classroom, unable to concentrate on schoolwork, skipping from one task to another
Combined ADHD
Mix of inattentive and hyperactive-impulsive symptoms.
Hyperactive-Impulsive ADHD
Hyperactivity without inattentiveness
concordance rate
The percentage of twin pairs or other pairs of relatives that exhibit the same disorder. (nature vs. nurture)
comorbid
Presence of two or more unrelated disease conditions at the same time in the same person
Trephination
An ancient operation in which a stone instrument was used to cut away a circular section of the skull, perhaps to treat abnormal behavior and melancholy.
-Thomas Willis
general paresis
disease that leads to paralysis, insanity, and eventually death; discovery of this disease helped establish a connection between biological diseases and mental disorders
-Discovered to be a consequence of syphilis
-Syphilis discovery provided proof that psychological disorders could have medical causes (paved the way for a biomedical approach to psychological disorders)
Sigmund Freud's "talking cure"
foundational psychoanalytic technique where patients talked through traumatic memories and suppressed emotions with a therapist, allowing them to release pent-up feelings and gain insight, reducing hysterical symptoms
-first formal therapy for psychological disorders that drew attention to environmental and social factors in mental illness.
Classical Psychoanalysis
• Freud believed that emotionally charged memories and conflicts were repressed (pushed out of consciousness) i.e. “motivated forgetting.”
• Emotions around repressed memories were expressed in symptoms like aggression, anxiety, depression and in physical symptoms like “psychogenic pain”
• The goal of psychoanalysis was to bring unconscious conflicts and emotions into consciousness where they could be dealt with rationally.
Freud's motivated forgetting
emotionally charged memories and conflicts were repressed (pushed out of consciousness)
Freud's psychogenic pain
individual feels pain but the cause is emotional rather than physical
Classical Psychoanalysis: Strategies to Access the Unconscious
-Free association
-Resistance
-Transference
-Slips of the Tongue
-Interpretation of Dreams
Freud's "Free association"
A method in which the patient says anything that comes to mind, no matter how apparently trivial, embarrassing, or disagreeable.
Freud's "Resistance"
A patient's self-censorship or avoidance of certain topics.
Freud's "Transference"
Interpreting how the patient acted toward the therapist, considered to be a re-enactment of significant relationships (emotional re-education)
Freud's "Slips of the Tongue"
mis-speaking provided insight into true beliefs
Freud's "Interpretation of Dreams"
considered the content of dreams to be an expression of the unconscious that could be interpreted thru Interpreting symbols which he thought of as the language of dreams.
Psychodynamic Approaches
Modern version of psychoanalysis
• less frequent than Freud's (daily) sessions and lasts months to a year, not years
• meet face-to-face (rather than out of sight while the patient reclined on a couch)
• conscious thoughts receive as much consideration as unconscious conflicts
• includes focus on improving current responses to stressors to improve functioning + relieve symptoms
Interpersonal therapy (IPT)
Psychodynamic approach; assumption is that mood is tied to relationship quality and life events.
• Targets problems like life transitions, complicated grief, interpersonal disputes, and interpersonal deficits
• Time limited (usually 12-16 weeks)
• First weeks are spent collecting information, creating an "interpersonal inventory" of relationships, and choosing a focus for therapy
• Subsequent sessions consider actions that could improve the situation
Humanistic Approaches
-Focus on self-actualization, growth, the present and the future
-Assumes all humans are oriented toward growth, the search for meaning and self-actualization
-Therapy focuses on the present and the future
-Helps patients see themselves as agents in their lives, and take productive action and responsibility
Motivational interviewing
focuses on helping a client reduce ambivalence about a problematic behavior by clarifying the discrepancy between their stated goals and their actual actions
-used in Serious Mental Illness (e.g. schizophrenia), before beginning an intervention
Client-centred therapy (person-centred therapy)
"Rogerian therapy"; the therapist's genuineness, unconditional positive regard, and empathic understanding are crucial to therapeutic success
• Seeks to help clients accept themselves as they are without pretense or self-imposed limits
Behavioural Therapy
A style of psychotherapy in which the therapist uses the principles of classical and operant conditioning to change the person's behaviour from maladaptive to adaptive.
Exposure Therapy
Remove the anxiety connected to a feared stimulus through repeated approach toward the feared stimulus.
Exposure Techniques:
• Systematic desensitization
• In vivo exposure
• Exposure and Response Prevention
In vivo exposure
Exposure technique; Patient is exposed to the phobic stimulus in the real world or through interactive computer programs (VR)
Systematic desensitization
Exposure technique; gradually increasing encounters with the feared stimulus with periods of relaxation between
Exposure and Response Prevention
Exposure technique; Behavioural treatment of OCD where the patient delays performing the compulsion to relieve anxiety
Rational Emotive Therapy
Cognitive approach; therapist challenges the patient's irrational beliefs.
• Pioneered by Albert Ellis
• Assumes that beliefs (B) link activating events (A) and consequences (C)
• If a client's beliefs are irrational, they will lead to negative consequences. The therapist disputes the irrational beliefs and offers more effective substitutes.